The current state of studies proves that mechanical thrombectomy with stent retrievers is nowadays the standard therapy in cerebrovascular accident patients with proximal vessel occlusion in the anterior circulation. Systemic thrombolysis and endovascular thrombectomies are in many ways complementary procedures. Systemic thrombolysis appears to be very effective for peripheral vascular occlusions in the 4.5-hour time window; at the same time, mechanical thrombectomy is more difficult and risky here because of the vessel caliber. Proximal large vessel occlusions (ICA, MCA), on the other hand, should be treated endovascularly. The role of systemic thrombolysis in proximal vascular occlusion is currently the subject of clinical trials. Thus, the relevant criterion for patient selection is the site of vascular occlusion, which must be visualized with MR angiography or CT angiography before initiation of therapy. Advanced imaging techniques such as CT or MR perfusion are helpful in decision making in many cases, especially imaging of infarct volume with MRI.
Clinical treatment of acute ischemic stroke has changed fundamentally in recent years: In addition to systemic thrombolysis, mechanical thrombectomy has become established as a standard procedure.
Several randomized trials in 2014 and 2015 showed a clear advantage of endovascular therapy (thrombectomy) in combination with best drug therapy (mostly systemic thrombolysis) compared with best drug therapy alone. Nevertheless, not all stroke patients are suitable for endovascular intervention; clinical and neuroradiological aspects determine patient selection.
Development of stroke therapy
After an initial three negative randomized controlled trials (RCT) of endovascular therapy for acute ischemic stroke in 2012 (IMS III3, Synthesis-Expansion, and MR Rescue) [1–3], a total of five positive randomized trials (MrClean, Escape, Extend IA, SWIFT Prime, Revascat, Fig. 1) followed in 2014 and 2015 [4–8]. Here, the patient population studied showed significantly better neurological recovery as measured by the Modified Rankin Scale (mRS) after three months in the endovascular treatment arm of the study. The efficiency was excellent. According to a meta-analysis of individual patient data from the five randomized trials, the NNT is 2.6. Thus, it is the most efficient acute phase treatment for ischemic stroke [9].
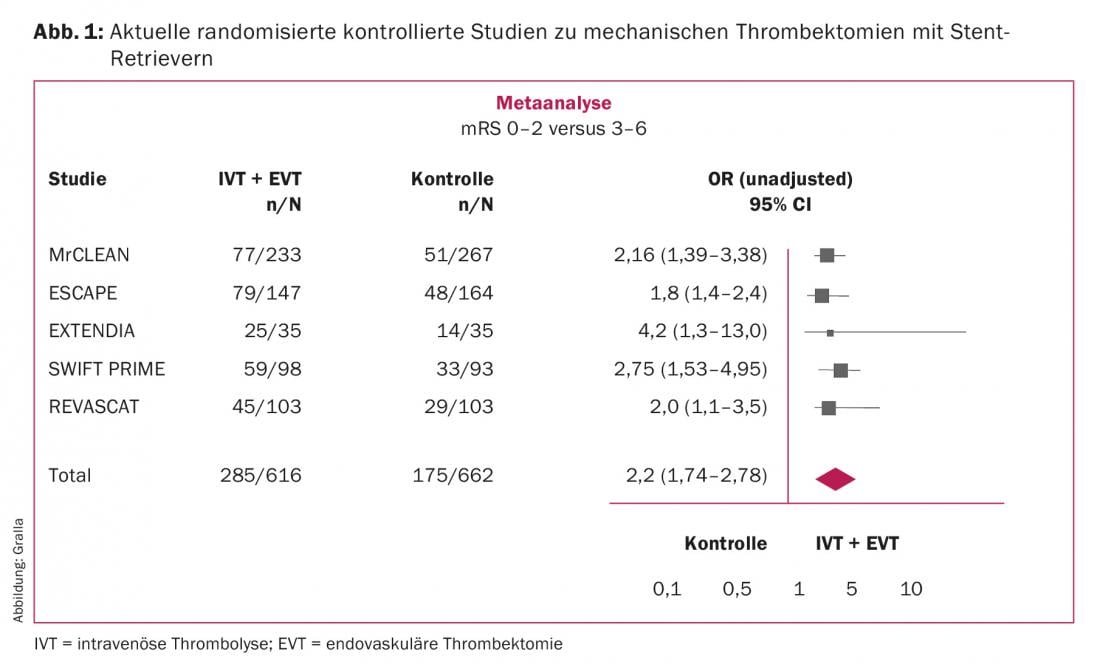
Basically, all studies investigated the effects of endovascular therapy in combination with best drug therapy for acute stroke (mostly systemic thrombolysis) compared with best drug therapy alone. The methodological difference between the negative studies in 2012 and the positive studies that followed was ultimately the more focused patient selection in 2014/15, as well as the consistent use of modern thrombectomy techniques with stent retrievers. These are retractable stents that can be used to remove thrombi from intracranial vessels. Since then, stent retrievers have been considered the first choice for thrombectomy in acute ischemic stroke; aspiration catheters are currently under evaluation.
Patient selection in studies
In the previous studies, patients were selected exclusively according to clinical criteria (the acute neurological deficit with an urgent suspicion of acute intracranial vascular occlusion). Imaging was widely used to exclude intracerebral hemorrhage before systemic thrombolysis. The cited studies evaluated exclusively patients with anterior circulation strokes (middle cerebral artery, internal carotid artery).
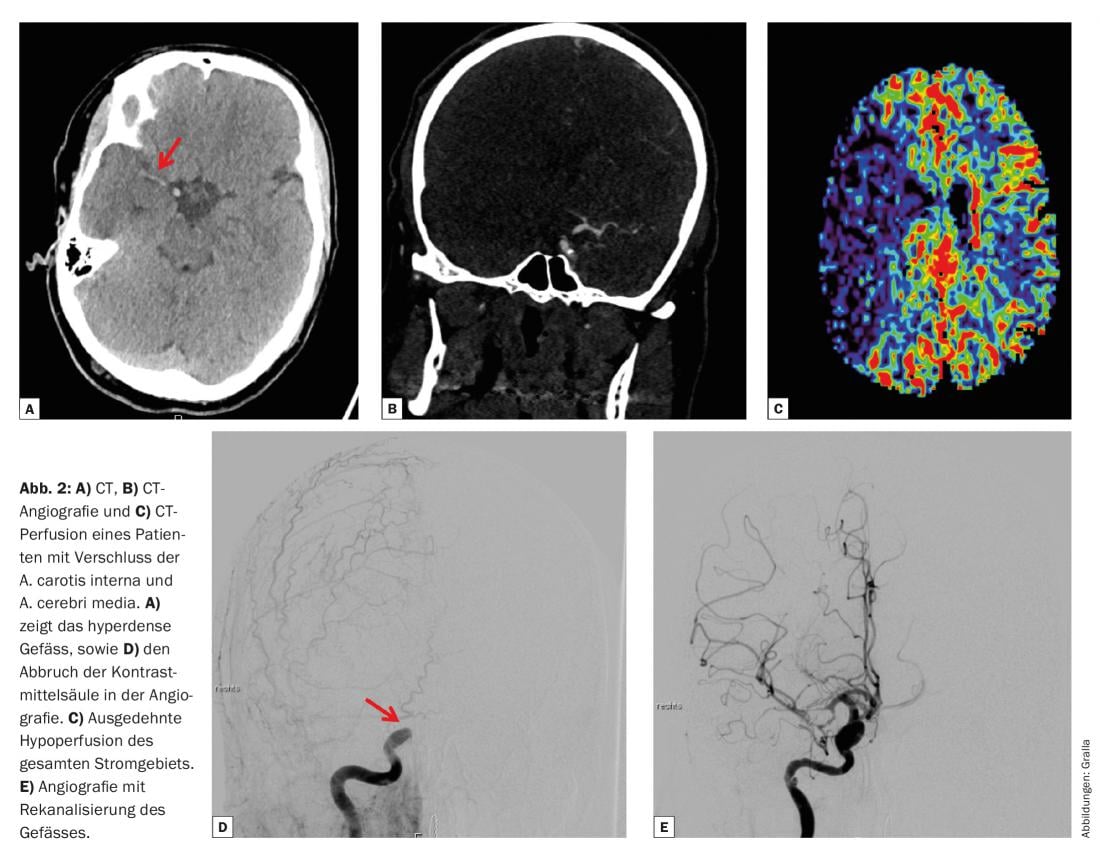
The current studies draw clear clinical and imaging selection criteria from computed tomography and magnetic resonance imaging. The goal is to identify patients with proximal vascular occlusions. Proximal vascular occlusions are occlusions of the internal carotid artery intracranially including the terminal segment, the main stem of the middle cerebral artery (so-called M1 segment), and the branches of the middle cerebral artery near the bifurcation (M2 segment) (Fig. 2).
The studies differed with respect to clinical inclusion and exclusion criteria, e.g., age, NIHSS (severity of stroke), and time window of treatment. The MrClean study had very broad inclusion criteria: Age greater than 18 years (with no upper age limit), and a low NIHSS ≤2. Other studies, for example SWIFT Prime, included only patients between 18 and 85 years of age, and only those with an NIHSS between 8 and 29 years were accepted. In fact, patients older than 80 years and with low NIHSS also benefited significantly from endovascular therapy in the trials.
The meta-analysis mentioned earlier [9] showed that both sexes, all age categories, patients with severe stroke symptoms, patients with and without prior intravenous thrombolysis, and also those in the time window after five hours benefit from endovascular treatment.
Current criteria for patient selection in clinical practice
In principle, patients with an acute stroke must be given adequate therapy as quickly as possible. In addition to systemic thrombolysis in the 4.5-hour time window, mechanical thrombectomy with or without concomitant thrombolysis has become established.
Age, NIHSS, or time window after symptom onset factor into decision making but are not sole exclusion criteria. The decisive selection criterion for stroke therapy is the site of occlusion and thus the visualization of the site of occlusion with CT angiography (CTA) or MR angiography (MRA). Thus, performing CTA or MRA in addition to native imaging to rule out bleeding is mandatory and triggers therapy:
- Peripheral occlusions, usually associated with low NIHSS (distal occlusions of the middle or anterior cerebral artery), usually have a small thrombus, this has a high probability of recanalization under systemic thrombolysis [10]. In addition, peripheral occlusions are difficult to reach with mechanical thrombectomy and are then likely to have an increased complication rate. In peripheral vascular occlusions beyond the time window for systemic thrombolysis, mechanical thrombectomy is generally not possible for the reasons mentioned; if necessary, intra-arterial thrombolysis should be discussed.
- Proximal vessel occlusions, on the other hand, have a lower recanalization rate under systemic thrombolysis, so that mechanical thrombectomy is usually indicated/necessary for ICA and MCA occlusions even after systemic thrombolysis. In principle, however, lysis and mechanical thrombectomy should generally be regarded as complementary because of their very different spectrum of action and application. The value of adjunctive systemic thrombolysis before mechanical thrombectomy for proximal vessel occlusion is currently under intense debate. The probabilities of recanalization are as low as 4-6%, depending on the site of vessel occlusion and the time interval (data from the Bern Stroke Registry, currently under review). At the same time, systemic thrombolysis is costly, may delay mechanical thrombectomy, and increases the risk of intracranial hemorrhage. These aspects are the subject of future studies.
Other imaging criteria in decision making
Decision making about therapy is often more complex in everyday clinical practice than depicted in the study setting. Patients have comorbidities, reach the center beyond the traditional treatment window, or otherwise have limitations in clinical prognosis. Both CT and MRI suggest other possible criteria for treatment decision.
Individual studies have shown that patients with unclear symptom onset in time (eg, wake-up strokes) or beyond the designated 8-hour time window may also benefit from mechanical thrombectomy. However, further imaging criteria must be used here. In these patients, MRI imaging (T2 weighting and FLAIR weighting) can be used to estimate the age of the infarct; in the absence of demarcation of the infarct, these patients can be transferred to endovascular therapy with comparative safety.
The extent of the initial brain damage and the neurological outcome can already be estimated to a certain extent on the basis of the native CT and the CTA (ASPECT score, collateral score). CT perfusion can be used to qualify the extent of hypoperfusion. Compared with CT, MRI offers several advantages, in particular good visualization of infarct volume by diffusion weighting. Thus, a true mismatch between infarct volume and critical hypoperfusion can be presented. The disadvantages of MRI imaging are a slightly longer examination time and higher costs.
Many of these parameters are currently used in the discussion of so-called “futile recanalization,” that is, recanalization or reperfusion of the territory without relevant clinical improvement. The background to this is that patients with an already completely formed infarct area no longer benefit relevantly from the therapy.
Nevertheless, in the authors’ opinion, there is currently insufficient validation of these parameters to deprive patients in principle of highly efficient endovascular therapy for stroke with mechanical thrombectomy.
Guidelines
The current state of studies and clinical practice guidelines have been summarized by the American Heart Association (AHA) and the European Stroke Organization (ESO) [11,12].
Literature:
- Ciccone A, et al: SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013; 368(10): 904-913.
- Kidwell CS, et al: MR RESCUE Investigators. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 2013; 368(10): 914-923.
- Broderick JP, et al: Interventional Management of Stroke (IMS) III Investigators. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013; 368(10): 893-903.
- Berkhemer OA, et al: A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11-20.
- Goyal M, et al: Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019-1030.
- Campbell BC, et al: Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009-1018.
- Saver JL, et al: Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285-2295.
- Jovin TG, et al: Thrombectomy within 8 Hours after Symptom Onset in Ischemic Stroke. N Engl J Med 2015; 372: 2296-2306.
- Goyal M, et al: Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016 Apr 23; 387(10029): 1723-1731.
- Riedel CH, et al: The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 2011 Jun; 42(6): 1775-1777.
- Wahlgren N, et al: Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska Stroke Update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke 2016 Jan; 11(1): 134-147.
- Powers WJ, et al: 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015 Oct; 46(10): 3020-3035.
CARDIOVASC 2016; 15(4): 14-17