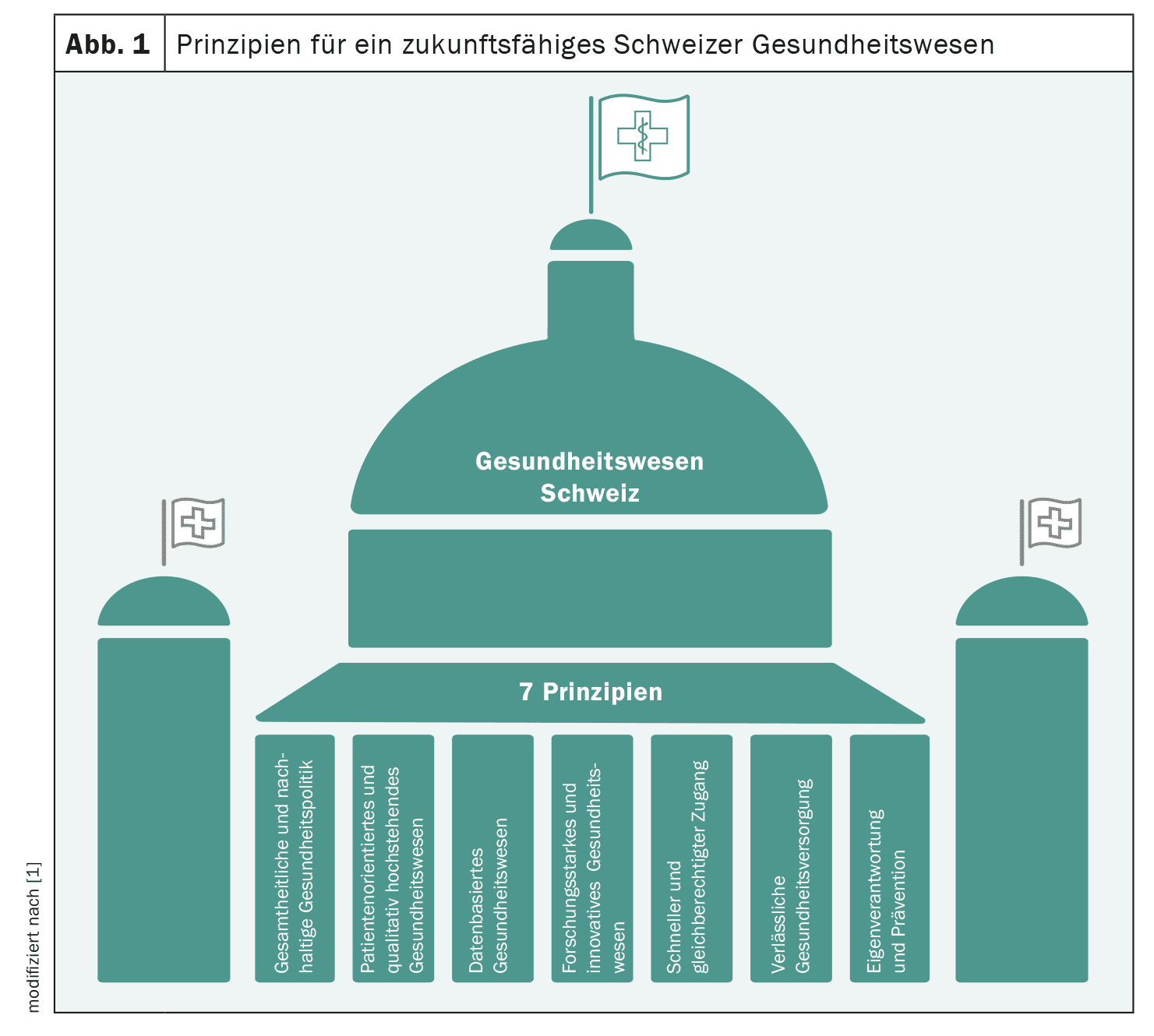
The challenges facing the Swiss healthcare system are great. An ageing population, but also growing demands as a result of medical progress, lead to cost pressure. International conflicts, increased protectionism and outdated licensing and pricing regulations are jeopardizing the security of supply. Switzerland also has a lot of catching up to do in terms of digitalization. A report by Interpharma shows which principles could make the Swiss healthcare system fit for the future.
(red) Society and politics must develop a holistic and sustainable healthcare strategy for the country. In view of the demographic development, the constantly increasing medical possibilities and the associated growing demands, new solutions are needed to ensure the quality, access and financing of the Swiss healthcare system in the long term. When defining this strategy, the focus must be on the benefits for patients. A coherent strategy with concrete goals and measures can only be developed if all stakeholders in the healthcare system are involved, seek dialog and work together constructively. Patient benefit and the quality of healthcare services should be at the heart of the healthcare system. This conviction is expressed in the patient-centered approach, which has become internationally known as “Value-Based Health Care”. For optimal, outcome-oriented treatment of patients, the focus must be on the result of the entire “treatment pathway”: This requires effective coordination beyond one’s own specialty; integrated care where the focus is on the benefit of the patient – not the outcome of the individual disciplines.
A central component for the further development of the healthcare system in Switzerland is the establishment of a nationwide digital infrastructure. Such an infrastructure enables seamless communication and collaboration between medical professionals and facilities, authorities, health insurers, manufacturers and patients. It helps to reduce bureaucracy, increase efficiency and contain costs in the long term. In addition, better networking enables stakeholders to plan, organize and make adjustments more effectively – even in crisis situations (such as during a pandemic). This in turn benefits the population and all stakeholders in the healthcare system. In addition, a digitalized healthcare system promotes transparency in the quality of healthcare providers, which in turn significantly improves the quality of care.
Dedicated to research
For Switzerland to maintain its position as the most innovative country in the world (according to the Global Innovation Index), it needs competitive framework conditions for researchers, optimal networking and collaboration between academia, spin-offs, start-ups and industry. Without the national and international networking of researchers, cutting-edge research is no longer conceivable, as research no longer knows any institutional or national borders. A research-friendly environment and attractive framework conditions are therefore crucial for basic research to produce innovations and for these to be developed through to clinical trials in Switzerland. Furthermore, education, research and innovation are key prerequisites for Switzerland to remain internationally competitive in the future.
Equal access for all
Fast and equal access to medical services is a top priority for patients. Access to healthcare via compulsory basic insurance is the foundation for this. This requires a pragmatic exchange between authorities, industry and science. A stable relationship between Switzerland and the EU as our largest sales and procurement market plays a key role here.
Last but not least, the personal responsibility and health education of the population should be promoted so that they can make decisions based on clear information and independently take measures to promote health and prevent disease – without government re-education measures. Prevention is the key to a healthier population and an important pillar of a holistic health strategy.
Source:
- Principles for a sustainable Swiss healthcare system. Interpharma, 2024.
InFo ONKOLOGIE & HÄMATOLOGIE 2024; 12(4): 35