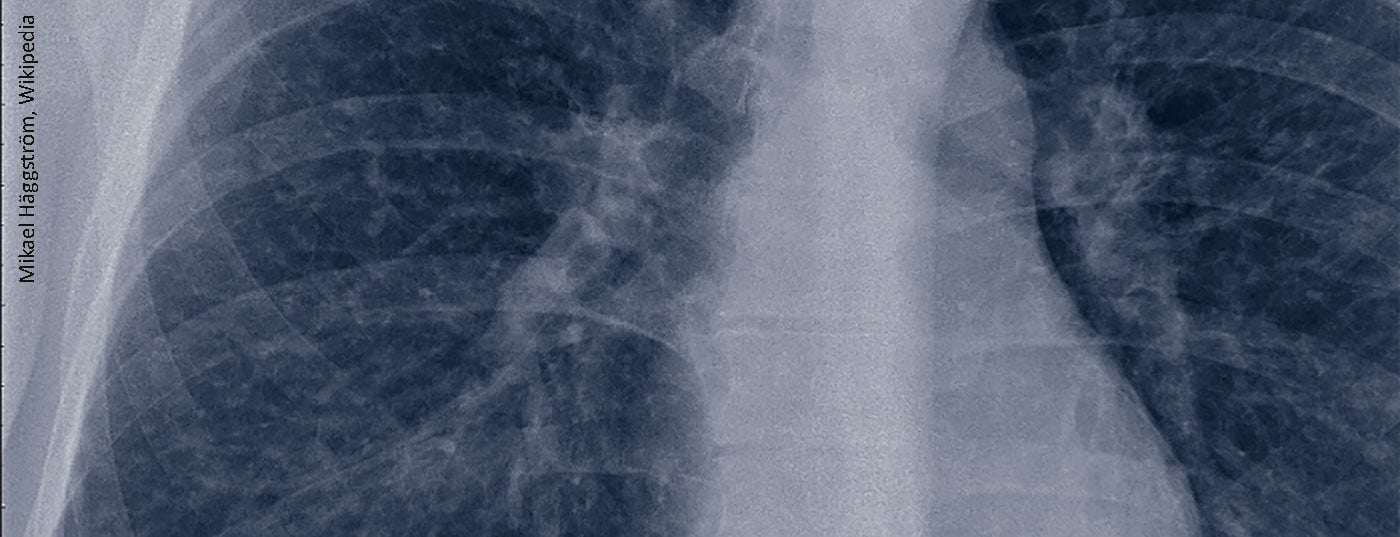
Sarcoidosis most commonly affects the lungs, but extrapulmonary manifestations also occur. Isolated involvement of a single organ or organ system is rare in sarcoidosis, so patients must be thoroughly evaluated for other disease manifestations. At the German Rheumatology Congress, an expert gave current recommendations for diagnosis and therapy of the disease.
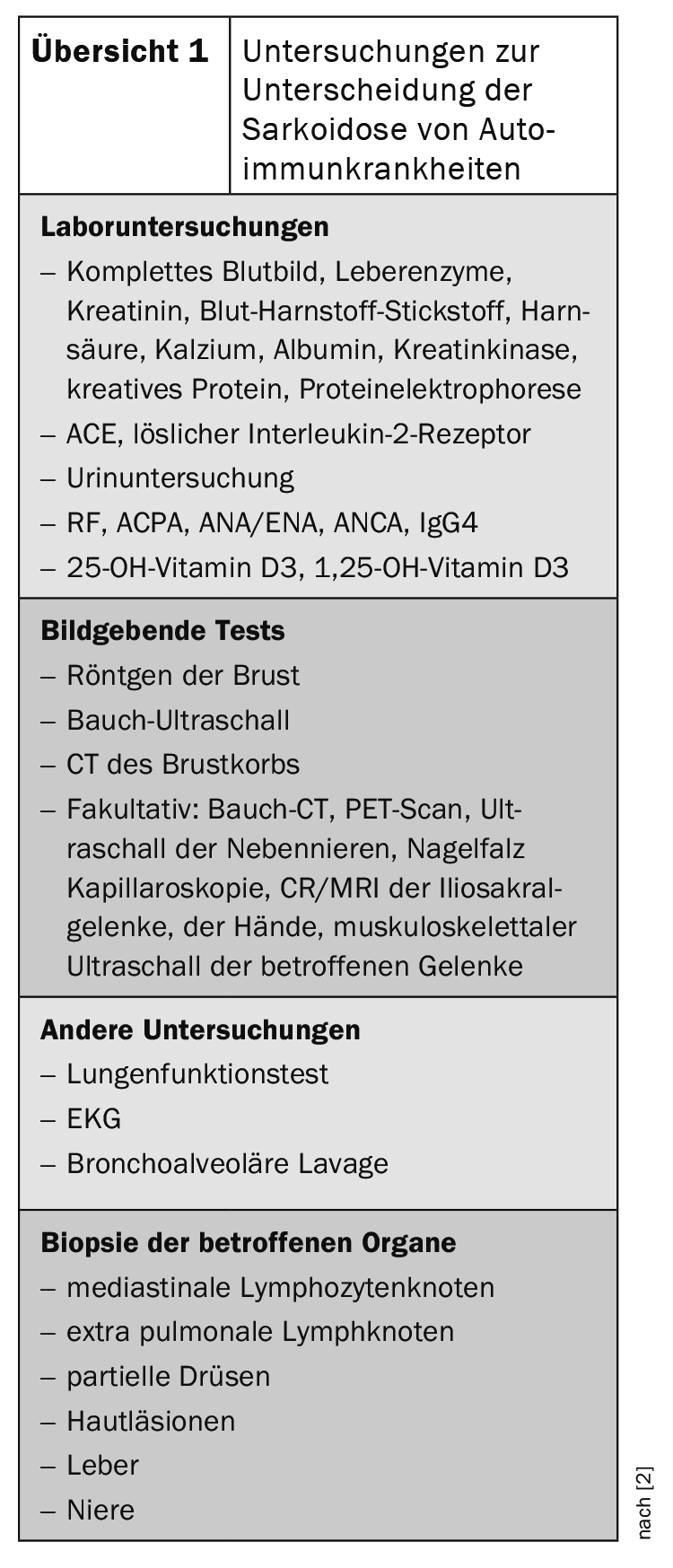
Because of the frequent lung involvement (over 90% [2]), sarcoidosis is often in the hands of pneumologists, but the clinical picture is also relevant for rheumatologists. In general, rheumatologic diseases with pulmonary involvement may also show other organ manifestations, such as renal, salivary gland, ocular, joint, and skin involvement. Differentiation from other autoimmune diseases is done by laboratory tests, imaging tests, or a biopsy of the affected organs (review 1) [3].
Current recommendations for diagnostics
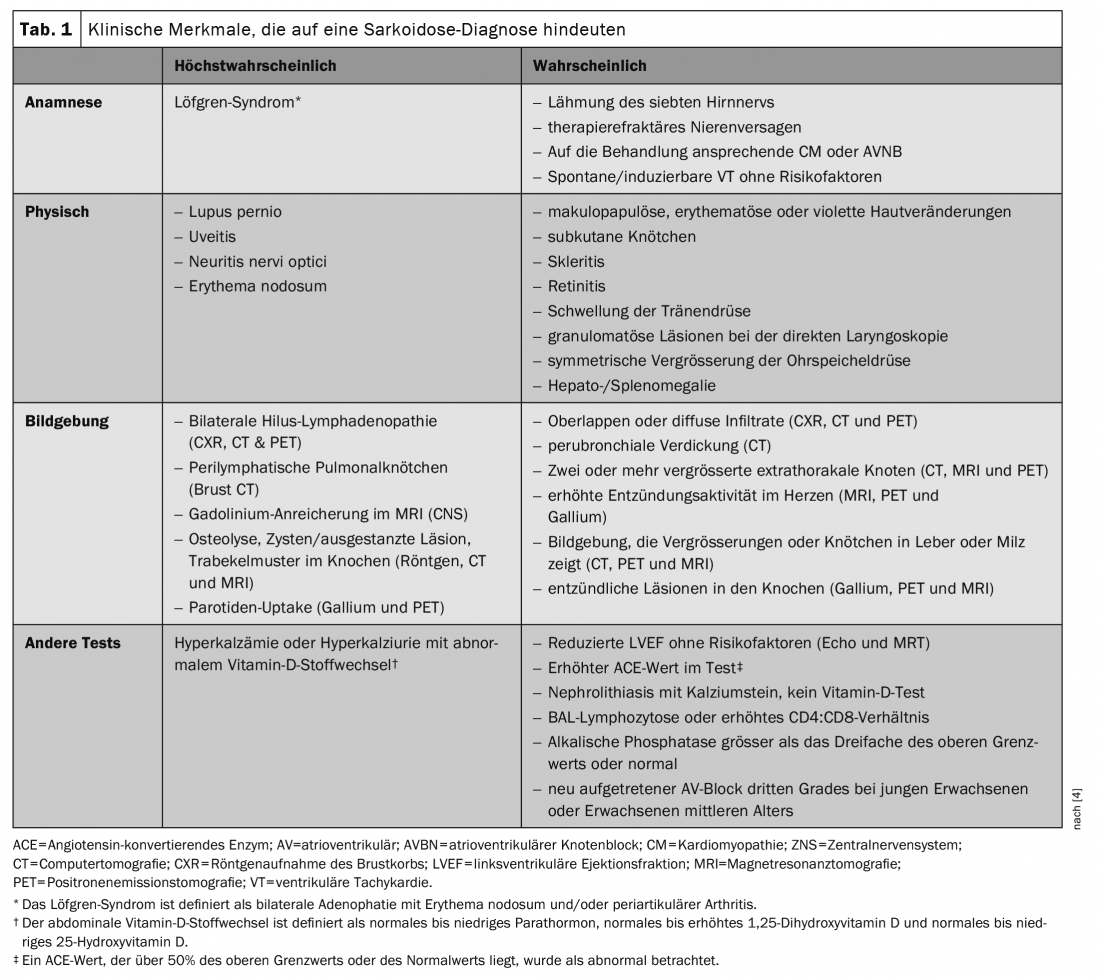
The diagnosis of sarcoidosis is not standardized but is based on three main criteria: A compatible clinical presentation, the finding of non-necrotizing granulomatous inflammation in one or more tissue samples, and the exclusion of alternative causes of granulomatous disease. However, there are no universally accepted measures to determine whether each diagnostic criterion has been met. While many cases of sarcoidosis present a diagnostic dilemma, certain clinical features of sarcoidosis are considered so highly specific to the disease that they are considered diagnostic. These include Löfgren’s syndrome, lupus pernio, and Heerfordt’s syndrome. Other features have been strongly associated with sarcoidosis, such as bilateral adenopathy of the hilar region in patients without B symptoms (fever, night sweats, and weight loss) (Table 1) [4]. In Löfgren’s syndrome, lupus pernio, Heerfordt’s syndrome, and biiliary lymphadenopathy without B symptoms, biopsy detection may not be necessary. In all other cases, sarcoidosis cannot be excluded with certainty, which is why the diagnosis should always be made by biopsy as well.
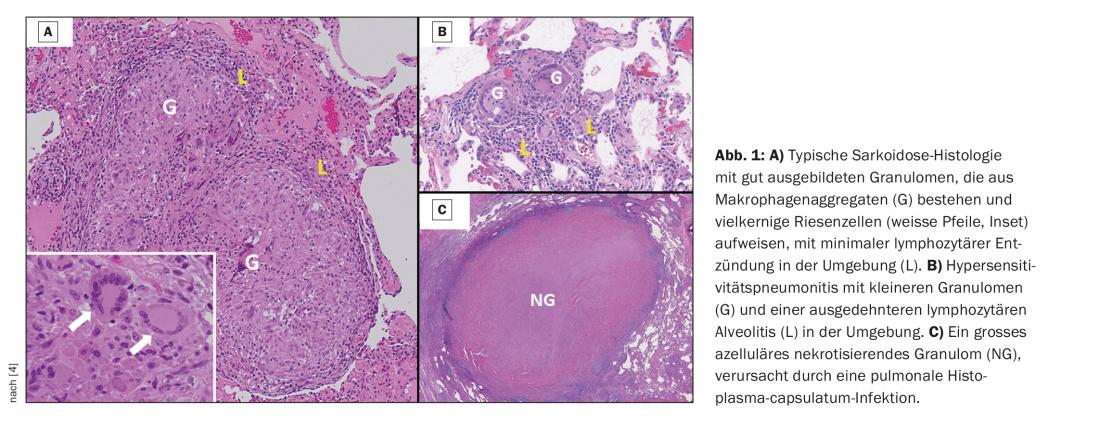
Because the clinical manifestations of sarcoidosis are often nonspecific, histologic evaluation of tissue granulomas is often required to establish the diagnosis. Histologic features typical of sarcoidosis granuloma include the presence of well-formed, concentrically arranged layers of immune cells, with the central core of macrophage aggregates and multinucleated giant cells being most prominent. An outer layer of loosely organized lymphocytes, usually T cells, is often observed with some intervening dendritic cells. In some cases, the granulomas are surrounded by isolated collections of B lymphocytes. Sarcoidosis granulomas are nonnecrotic in most cases; however, variants of sarcoidosis, particularly the nodular pulmonary sarcoidosis phenotype, may occur with a mixture of necrotic and nonnecrotic granulomas. Figure 1 shows histopathologic features useful for distinguishing sarcoidosis from other causes, although histopathologic features alone cannot distinguish sarcoidosis from other granulomatous diseases.
Screening for extrapulmonary diseases
In patients with sarcoidosis, a baseline eye examination is recommended to screen for ocular sarcoidosis. Patients who do not have renal symptoms or established renal sarcoidosis should have a baseline serum creatinine test to screen for renal sarcoidosis. In patients with sarcoidosis who do not have hepatic symptoms or established hepatic sarcoidosis, a serum alkaline phosphatase test is recommended to screen for hepatic sarcoidosis. For patients who have neither hepatic symptoms nor proven hepatic sarcoidosis, no recommendation is made for or against a baseline serum transaminase test. A baseline serum calcium test to screen for abnormal calcium metabolism, however, should be performed. If an assessment of vitamin D metabolism is deemed necessary in a patient with sarcoidosis, for example, to determine whether vitamin D supplementation is indicated, it is recommended that both 25- and 1,25-OH vitamin D levels be measured before vitamin D supplementation. In addition, a complete blood count should be obtained to detect hematologic abnormalities. Performing a baseline ECG to screen for possible cardiac involvement is also recommended. In contrast, routine transthoracic echocardiography (TTE) or 24-hour ambulatory ECG monitoring (Holter) is not recommended to screen for possible cardiac involvement [4].
Diagnostic evaluation of suspected extrapulmonary disease.
If cardiac involvement is suspected, cardiac magnetic resonance imaging (MRI) rather than positron emission tomography (PET) or TTE is recommended to provide both diagnostic and prognostic information. For patients with suspected cardiac involvement who are treated in a setting where cardiac MRI is not available, it is recommended that a dedicated PET be performed in lieu of TTE to provide both diagnostic and prognostic information. Patients suspected of having pulmonary hypertension (PH) should have an initial evaluation by TTE. If PH is merely suspected or suggested by a transthoracic echocardiogram, a right heart catheterization should be performed to definitively confirm or rule out PH. If PH is suspected but not indicated by a transthoracic echocardiogram, the need for right heart catheterization should be decided on a case-by-case basis [4].
Treatment dependent on manifestations
The main reasons for treating sarcoidosis are to reduce the risk of morbidity and mortality and to improve the quality of life. The indication for treatment varies depending on which manifestation is causing the symptoms: lung, heart, brain, skin, or other. Manifestations of cardiac sarcoidosis include atrioventricular conduction delay, His-Purkinje system conduction block, ventricular and supraventricular tachyarrhythmias, and cardiomyopathy. Therefore, in patients with evidence of functional cardiac abnormalities, including heart block, arrhythmias, or cardiomyopathy, the use of glucocorticoids is recommended.
The clinical manifestations of symptomatic neurosarcoidosis often result in significant impairment of the sarcoidosis patient’s quality of life and include facial paralysis, optic neuritis, aseptic meningitis, severe sequelae of granulomatous mass lesions of the central nervous system, hydrocephalus, and encephalopathy/psychosis. Therefore, for patients with clinically significant neurosarcoidosis, treatment with glucocorticoids is recommended. In patients with neurosarcoidosis who have been treated with glucocorticoids and in whom the disease persists, it is recommended that methotrexate be added. If the disease persists, infliximab should be administered.
Before sarcoidosis-associated fatigue (SAF) can be diagnosed, other causes of fatigue must be ruled out. These include diabetes mellitus, thyroid dysfunction, neuroendocrine disorders, mental disorders (especially depression), obstructive sleep apnea, small-fiber neuropathy, vitamin D deficiency (especially low 1,25-dihydroxycholecalciferol levels), heart failure, and neurologic disease. In patients with sarcoidosis who suffer from troublesome fatigue, a pulmonary rehabilitation program and/or inspiratory muscle strength training for 6-12 weeks is recommended to improve fatigue. If fatigue is not related to disease activity and testing of a pulmonary exercise or rehabilitation program has been completed, the use of D-methylphenidate or armodafinil for 8 weeks is recommended to test the effect on fatigue and tolerability [5].
Congress: German Rheumatology Congress 2021
Literature:
- Dr. Peter Korsten, Current recommendations for the diagnosis and therapy of sarcoidosis, lecture German Rheumatology Congress 2021, Sept. 17, 2021.
- Al-Kofahi K, et al: Management of extrapulmonary sarcoidosis: challenges and solutions. Ther Clin Risk Manag 2016, doi: 10.2147/TCRM.S74476.
- Korsten P, et al: Sarcoidosis and autoimmune diseases: differences, similarities and overlaps. CURR OPIN PULM MED 2018, doi: 10.1097/MCP.0000000000000500.
- Crouser E, et al: Diagnosis and Detection of Sarcoidosis. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med 2020, doi: 10.1164/rccm.202002-0251ST.
- Baughman R, et al: ERS clinical practice guidelines on treatment of sarcoidosis. Eur Respir J 2021, doi: 10.1183/13993003.04079-2020.
InFo PAIN & GERIATry