In an interview with DERMATOLOGIE PRAXIS, PD Dr. Dr. med. Ahmad Jalili, specialist in dermatology and venereology at the Dermatology & Skin Care Clinic and president of DermaNet Switzerland, talks about the topic of modern systemic therapy approaches for atopic dermatitis. In doing so, he provides a practical insight into the current standards and empirical values in diagnostics and treatment. In addition to the subcutaneously applied biologic dupilumab, the oral JAK inhibitor baricitinib was recently approved.
Thank you very much for taking the time to answer our questions. Atopic dermatitis is one of the most common chronic recurrent skin diseases. What are the criteria used in practice to classify moderate to severe symptomatology?
Dr. Jalili:
In practice, we often use the IGA* scores, this is also due to lack of time. This allows us to classify atopic dermatitis with a score from 0 (appearance-free) to 4 (severe disease). It is predominantly a visual process that saves a lot of time. We can use it to assess atopic dermatitis so very quickly. On the other hand, we also use SCORAD** or EASI#. I favor the SCORAD because it allows us to assess not only the clinical presentation of the patient, but also the itch. In summary, the IGA is definitely ranked #1, followed by SCORAD and EASI. We often use a visual analog scale (VAS) to determine itch.
* IGA = Investigator Global Assessment
** SCORAD = SCORing Atopic Dermatitis
# EASI = Eczema Area and Severity Index
What clinical manifestations are most distressing for this patient population?
Definitely the itching, as well as sleep disturbances and when the eczematous lesions are in visible localizations, for example, in the area of the face or the back of the hand.
What are currently realistic treatment goals in patients with moderate to severe atopic dermatitis?
With conventional systemic therapies such as ciclosporin or methotrexate (MTX), we can be satisfied with an EASI50, sometimes a little more, meaning a 50 percent improvement in clinical symptoms. Regarding Dupilumab – currently the only biologic for the treatment of moderate to severe atopic dermatitis – we can expect an EASI75 to EASI90. This means that we can achieve higher targets with the new therapy options.
Recently, baricitinib (Olumiant®) was approved by Swissmedic as the first JAK inhibitor for this indication. In studies, this drug proved to be very effective, especially with regard to itch relief. Has this been confirmed in practice?
Definitely, I can confirm this. Some patients of ours who we treat with baricitinib report that the itching is completely gone within 2 to 3 hours at most. It is a great advantage of baricitinib, respectively this group of drugs, that a very fast itch relief is induced.
Are there patient groups that are particularly suitable for treatment with baricitinib?
Moderate to severe dermatitis and especially patients who do not want to have injections, thus prefer oral medication. In addition, patients who suffer severely from itching symptoms.

What are the main decision criteria for using this JAK inhibitor?
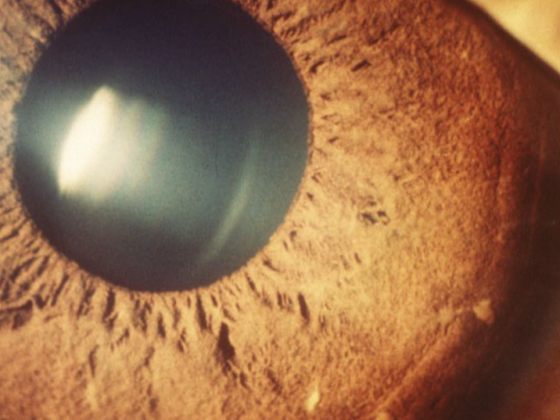
One is the presence of pruritus, the other is that in a group of patients treated with dupilumab, conjunctivitis manifests as a side effect. However, we also know that atopic dermatitis per se have a higher incidence of conjunctivitis. This means that individuals who are known to have a tendency to develop conjunctivitis independent of therapy are better suited for treatment with a JAK inhibitor than with the biologic dupilumab.
What are the main differences with other currently approved systemic therapies?
This is an interesting question. Baricitinib can be used to inhibit two JAK molecules: JAK1 and JAK2. Thus, it is not so much a broad-spectrum JAK inhibitor as a selective one. Definitely, we see less immunosuppression compared to conventional systemic therapies like ciclosporin or methotrexate. It must be said that in Europe the only approved conventional systemic drug is cyclosporine. But methotrexate is often used off-label.
Adherence is an important factor in the treatment of atopic dermatitis. What is your experience regarding patient adherence to baricitinib therapy?
That’s a good question. In general, baricitinib has a short half-life. With a break with this drug, the symptoms, especially itching, return very quickly. We know that itching is a major problem in patients with atopic dermatitis. Therefore, I think patients remain adherent in the long term, knowing that as soon as they pause therapy or miss taking their pills once or twice, the itching returns quickly. This is a motivation for patients to perform this therapy regularly.
How is the measurement of response and tolerability in practice?
We usually do clinical and laboratory (blood count, renal, liver, and CRP) checks every 3 months, as recommended for JAK inhibitors. Personally, I think that makes sense, especially since baricitinib is largely excreted through the kidney.
Treatment response/progression measurement: we most often use IGA to see if we have achieved our goal of twofold improvement in IGA score and completely to almost completely healed skin. When it comes to cost approval or further cost coverage by the health insurance, we also have to argue and document with SCORAD and EASI.
There are several guidelines for the treatment of atopic dermatitis. Which do you currently consider to be particularly relevant for everyday clinical practice?
Unfortunately, there is currently no guideline specifically designed for Switzerland. But we are currently in the process of drafting a consensus recommendation or, if necessary, a guideline with a group of experts. This would greatly facilitate daily work, especially in the office-based sector. As a template is definitely the European guideline [1,2]$ makes sense.
$ In the s2k guideline (AWMF registry number: 013-027) respectively the update on system therapy, JAK inhibitor therapy with baricitinib is not mentioned because the approval of Olumiant® is recent.
Interview: Mirjam Peter
Literature:
- Werfel T, et al: S2k Guideline on Diagnosis and Treatment of Atopic Dermatitis – Short Version. J Dtsch Dermatol Ges 2016; 14(1): 92-106.
- Werfel T, et al: Update “System therapy in atopic dermatitis” to the S2k guideline atopic dermatitis. 2020.
DERMATOLOGY PRACTICE 2021; 31(4): 18-19