In the age of personalized medicine, molecular diagnostics is also becoming increasingly important in dermatology. In a cross-sectional study published in the JDDG, their use in the areas of oncological, inflammatory and infectious dermatological diseases was investigated and it was identified which hurdles exist from the point of view of dermatologists in private practice with regard to the implementation of corresponding offers in practice.
The results of the online study were published in the Journal of the German Dermatological Society 2022 [1]. For the survey, an online questionnaire was sent to 2754 dermatologists via the e-mail distribution list of the Berufsverband der Deutschen Dermatologen e.V. in the period October-December 2020. A total of 192 practicing dermatologists completed the questionnaire, representing a response rate of 7% [1]. Of these, five were excluded from the analysis because they had not answered more than 50% of the questions. The remaining 187 participants had a mean age of 52.3±8.9 years, and 50.3% were female. The vast majority were specialists (96.8%, n=181) who had an average of 23.3±9.0 years of professional experience. About half of the participants (51.3%, n=96) were in solo practice and about 30% worked with one (n=59) or two dermatologists (n=58).
74 of the respondents (39.6%) reported using molecular diagnostics in their dermatology practice [1]. Users and non-users did not differ significantly in age or work experience. Users performed an average of 90.5±155.3 molecular diagnostic services per quarter, with most (40.0%, n=28) performing fewer than 50 tests. About 44.3% (n=31) said they did the testing either themselves or with an outside vendor. The most common microbiological-infectious service was fungal diagnosis (86.5%, n=64), followed by STD diagnosis (44.6%, n=33). The 70 dermatologists who provide these services in their practice reported performing an average of 226.4 ±296.4 services per quarter, with 45.7% (n=32) implementing them themselves. 79.7% of the 74 dermatologists stated that they do not offer any tests in the field of oncological diagnostics. Lymphoma diagnostics are used by 17.6% (n=13) of the respondents and melanoma diagnostics by 16.2% (n=12). Of those who reported performing oncology diagnostic procedures, 86.7% (n=13) used the assistance of outside providers. Regarding inflammatory/autoimmune diagnostic procedures, more than 80% (n=61) of the participants indicated that they would not use appropriate molecular diagnostic methods in their practice. The most common diagnostic procedures were genetic analyses such as HLA typing (6.8%, n=5) and PCR (6.8%, n=5).
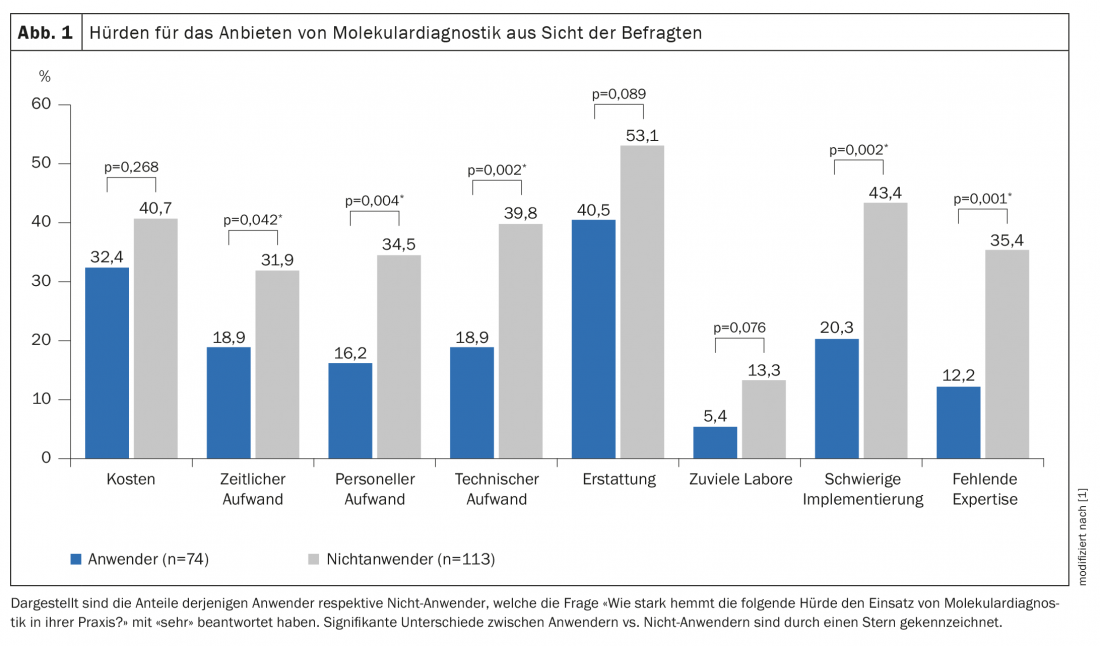
As in figure 1 can be seen, users and non-users differ significantly with regard to the aspects perceived as hurdles concerning offering molecular diagnostic procedures: time effort (18.9 vs. 31.9%), personnel effort (16.2 vs. 34.5%), technical effort (18.9 vs. 39.8%), difficult implementation (20.3 vs. 43.4%), lack of expertise (12.2 vs. 35.4%). Reimbursement, on the other hand, is perceived as a major problem by both groups (40.5 vs. 53.1%).
Literature:
- Tizek L, et al: Molecular diagnostics in dermatology: an online survey to investigate use, barriers and requirements in Germany. JDDG 2022; 20(3): 287-296.
- Stadler R, Has C, Bruckner-Tuderman L: Dermatologic diagnostics: search for the molecular “fingerprint”. Dtsch Arztebl 2018; 115 (20-21): 26; DOI: 10.3238/PersDerma.2018.05.21.05.
- Tietz H: Genetic engineering revolutionizes diagnostics. Der Deutsche Dermatologe 2020; 68: 688-697.
DERMATOLOGIE PRAXIS 2022; 32(2): 44-45











