Erectile dysfunction (ED) is a clinical problem encountered in family practice with increasing socioeconomic importance. Comprehensive evaluation is indicated in the presence of ED, as ED symptoms can be an important early marker of previously undiagnosed disease. Thanks to modern endovascular revascularization techniques, even small-caliber erection-related vessels can now be successfully revascularized by catheterization.
Erectile dysfunction (ED) is defined as the repeated inability to establish or maintain an erection that allows vaginal penetration during sexual intercourse. It affects millions of men worldwide, with ED occurring after the age of 40. The Massachusetts Male Aging Study (MMAS) reported an ED prevalence of 52% in men aged 40-70 years [1]. The incidence increases with age. In addition to ED, other common sexual disorders include reduced libido and ejaculation problems.
Sexuality in old age continues to be a big taboo in our society. For many older people, however, sexuality has a high value and is seen as an important source of vitality, well-being and an intact couple relationship. Therefore, disorders of sexual function lead to an impairment of the quality of life as well as the couple relationship that should not be underestimated.
Causes of erectile dysfunction
The causes of ED are often multifactorial. In essence, arterial, cavernous-venous, endocrine, neurogenic, and psychogenic factors play a role. In addition to age, the main causes in many patients with ED are cardiovascular disease. Risk factors include, in particular, coronary artery disease (CAD), peripheral arterial disease, nicotine abuse, arterial hypertension, hyperlipidemia, diabetes mellitus, and a positive family history. In addition, trauma and pelvic surgery, as well as various medications, can lead to or promote ED.
Since the publication of Goldstein et al. 1998, the first large study on sildenafil, it can be claimed without exaggeration that phosphodiesterase 5 inhibitors (PDE 5 inhibitors) have revolutionized the treatment of ED [2]. The success rate of sildenafil in all forms of ED is 50-80%. Therefore, the question often arises why a detailed diagnosis of ED should be made at all, since effective drug therapies with the PDE 5 inhibitors are available (Tab. 1).

Diagnostic workup for erectile dysfunction
For several reasons, a thorough workup should be performed prior to ED therapy. The central point lies in the detection of previously unknown diseases. A classic example is ED as the initial symptom of diabetes mellitus in a previously healthy patient. The prevalence of ED in diabetic patients over 60 years of age is approximately 75%, and the extent of ED increases proportionally with increasing disease severity.
In patients with myocardial infarction, a history of ED can often be elicited (>70%) that preceded the cardiac event by more than a year. This was demonstrated in the pioneering studies by Montorsi et al. impressively demonstrated [3]. ED is present in just over 50% of patients with acute angina and angiographically documented CAD.
Interestingly, the extent of ED correlates significantly with the number of coronary vessels affected. Because the diameter of penile arteries (1-2 mm) is smaller than that of coronary arteries (3-4 mm), the same extent of endothelial dysfunction and atherosclerosis results in a more significant and earlier decrease in blood flow in these vessels, which is why ED usually precedes a cardiac event [4]. ED occurs approximately three years before cardiac ischemic symptoms in almost all patients. For this reason, it is essential to clarify the affected patients in general medicine in order to detect other diseases at an early stage.
Another essential aspect is the question whether an ED is present at all or not. Nowadays, patients often have exaggerated ideas about their sexual performance. In this situation, a clarifying conversation is the decisive step and not the administration of PDE 5 inhibitors.
3-step scheme of ED diagnostics
The necessary steps in ED diagnosis follow a 3-step scheme (non-invasive, semi-invasive and invasive methods of clarification) and are in accordance with the guidelines of the German Urology Society (DGU) and the European Association of Urology (EAU) [5].
In the noninvasive workup of an ED, history and clinical examination are of central importance. These include questions about cardiovascular, neurological, and psychiatric diseases, as well as metabolic disorders. A detailed drug history is important, as the combination of PDE 5 inhibitors with nitrates in particular is a contraindication to their use. Nicotine and alcohol consumption should also be recorded. Hormonal disorders such as partial androgen deficiency in the elderly male (PADAM) may be associated with reduced libido and ED. To better quantify ED, questionnaires such as the International Index of Erectile Dysfunction (IIEF) may be useful.
Physical examination may reveal signs of secondary hypogonadism (hairiness, dry skin, muscle atrophy). Furthermore, the limb should be examined for phimosis or induratio penis plastica. Rectal palpation is mandatory to rule out prostatitis or prostate carcinoma. In addition, there are indications of possible prostate enlargement. Laboratory testing recommended is determination of glucose, lipid status, and total testosterone level.
In semi-invasive diagnostics, the corpus cavernosum injection test (SKAT test) is combined with duplex sonography to evaluate the arterial penile vessels. In the SKAT test, prostaglandin E1 (PGE1) is injected into the corpus cavernosum, this leads to increased arterial blood flow after relaxation of the cavernous muscle cells and to erection. For neurogenic or endocrine causes, an initial dose of 5 µg of PGE1 is sufficient; for vascular etiology, a dose of 10-20 µg is recommended. If adequate erections do not occur, the dose may be increased to 40 µg. Color-coded duplex sonography is performed to detect arterial flow in the paired profunda penile arteries in the proximal third of the shaft. Systolic flow velocity should be 30 cm/s according to the European Guidelines (EAU) >. In addition, contrast-enhanced computed tomography can now provide important information on the location of the arterial obstruction and thus be helpful in planning any endovascular intervention.
Invasive diagnostics include dynamic infusion cavernosometry-graphy (DICC) and selective intra-arterial angiography of the penile arteries. Both procedures have a very high informative value as far as the vascular status is concerned.
Erectile dysfunction treatment
For the vast majority of patients, the most attractive treatment option for ED is oral PDE 5 inhibition. Therefore, PDE 5 inhibitors are nowadays recommended as the first choice for ED therapy. They are clinically effective and have a favorable side effect profile. Four different PDE 5 inhibitors are currently approved: sildenafil, tadalafil, vardenafil, and the new more selective PDE 5 inhibitor avanafil (Table 1).
In the absence of therapeutic success with PDE 5 inhibitors, the next step is the use of SKAT injection. SKAT injections are particularly effective for organic and non-endocrine erectile dysfunction. The high effective concentration of the drug induces erection in many patients without systemic side effects. As a further option, Muse® (transurethral PGE1) can also be applied locally.
Testosterone substitution alone for ED therapy is rare (about 3%) – combination with a PDE 5 inhibitor is more common.
Vacuum pumps are effective in many patients because an erection-like state can be achieved that is sufficient for intercourse. Satisfaction rates are reported in the literature to be around 70%, with these figures referring to the couple.
Penile implants (semi-rigid or hydraulic models) are still considered ultima ratio. The insertion of a corpus cavernosum implant into the corpora cavernosa leads to irreversible destruction of the corpus cavernosum tissue and thus represents a definitive therapy.
Catheter Revascularization
If sonographic suspicion of arterial perfusion reduction is present, it may be possible to visualize it by computed tomography. The
Internal iliac artery cannot always be seen well by duplex sonography, so cross-sectional imaging may be helpful in patients with duplex sonographic evidence of reduced perfusion and cardiovascular risk factors. Provided there is arterial macroobstruction and no microangiopathy, endovascular catheter revascularization can be discussed (Fig. 1).
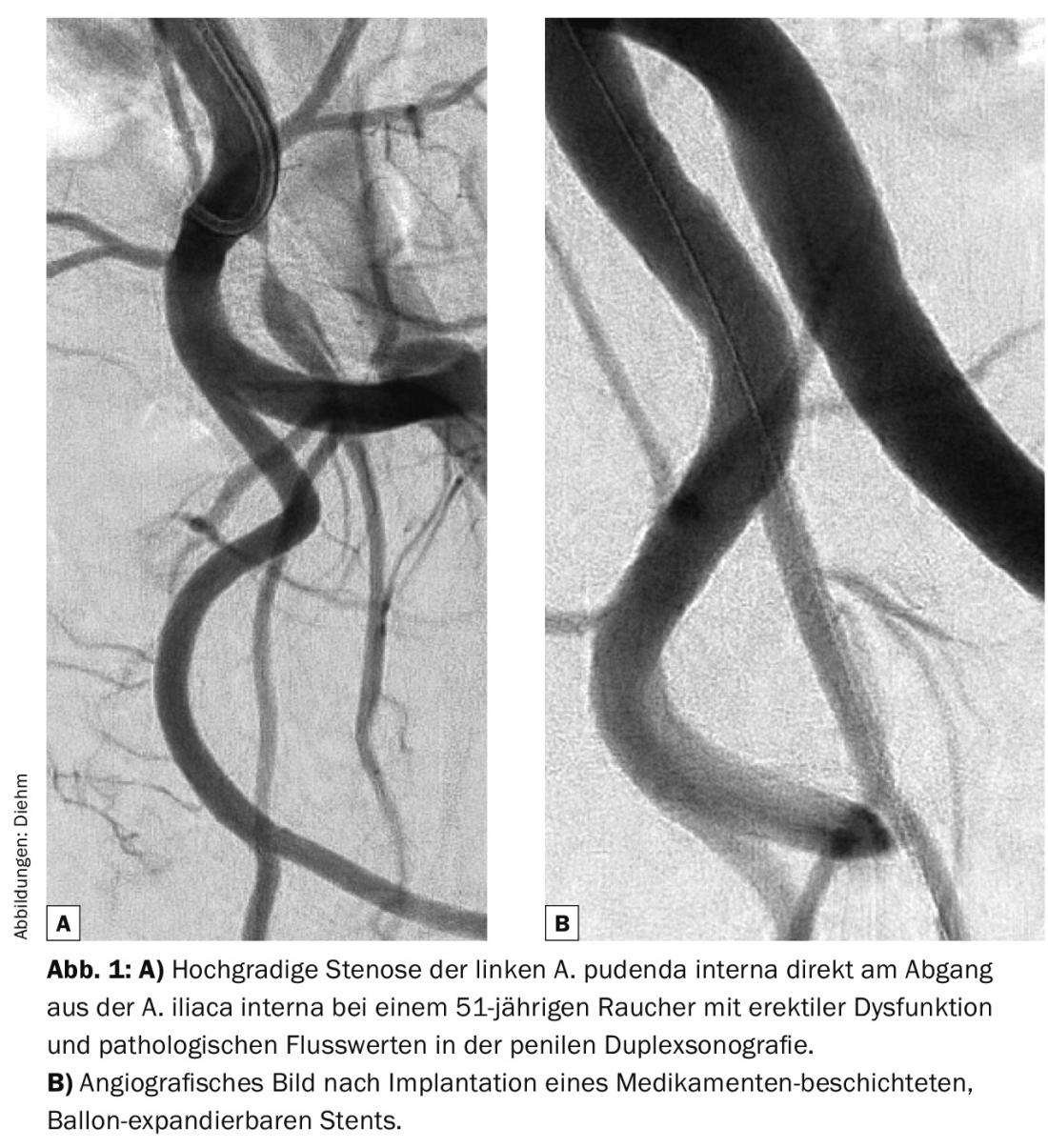
Obstructions of the proximal iliac arteries (Aa. iliacae communes, Aa. iliacae externae) can be successfully treated by catheterization for many years. In contrast, revascularization of the internal pudendal artery has been made possible mainly by miniaturization of catheter material in recent years. Accordingly, the current data situation is still relatively thin.
Rogers and colleagues treated 30 men aged about 60 years with a suboptimal response to PDE 5 inhibitors and angiographically verified stenosis of one or both arteries in the ZEN trial. pudendae internae by implantation of drug-eluting coronary stents [6]. A total of 383 patients required screening and 89 angiography. About one-third of the patients were not suitable for dilatation because of a lack of macroobstruction, and another third were not suitable because of excessive obstruction. The technical success of the intervention was 100%. After stent implantation, nearly 60% of dilated patients had improvement in function and penile blood flow. However, after six months, the angiographically verified residual stenosis rate was 34%. This pilot study shows encouraging results of endovascular therapy in patients with ED due to atherosclerosis.
Conclusion
In summary, ED represents an important marker symptom that is still often underestimated in its importance for the diagnosis of previously unrecognized diseases.
Not infrequently, arterial obstruction is present as a cause of decreased penile tumescence. Modern catheter-based procedures nowadays also allow arterial revascularization of small caliber penile vessels.
Literature:
- Johannes CB, et al: Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts male aging study. J Urol 2000 Feb; 163(2): 460-463.
- Goldstein I, et al: Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med 1998 May 14; 338(20): 1397-1404.
- Montorsi F, et al: Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. Eur Urol 2003 Sep; 44(3): 360-364; discussion 364-365.
- Gandaglia G, et al: A systematic review of the association between erectile dysfunction and cardiovascular disease. Eur Urol 2014 May; 65(5): 968-978.
- Hatzimouratidis K, et al, European Association of Urology: Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol 2010 May; 57(5): 804-814.
- Rogers JH, et al: Zotarolimus-eluting peripheral stents for the treatment of erectile dysfunction in subjects with suboptimal response to phosphodiesterase-5 inhibitors. J Am Coll Cardiol 2012 Dec 25; 60(25): 2618-2627.
Further reading:
- Diehm N, Baumann F: Erectile dysfunction – Technical advances enable endovascular therapy. Cardiovasc 2013; 2: 22-25.
CARDIOVASC 2016; 15(3): 32-35










