Two areas of impairment in old age were presented at Medidays in Zurich: macular degeneration and osteoporosis. The focus was on diagnosis and therapy. For wet macular degeneration especially an early work-up and the use of anti-VEGF drugs are recommended. Regarding osteoporosis therapy, the focus was on the efficacy and feasibility of certain treatment regimens in an elderly population that is multimorbid and taking comedic medications.
Dr. med. Roman Eberhard, Eye Clinic University Hospital Zurich, spoke about the basics, diagnostics and therapy of age-related macular degeneration (AMD): “Based on the Western world, this is the most common cause of blindness in patients over 65 years of age. And even in 45- to 64-year-olds, it follows right behind diabetic retinopathy as the second most common cause. The prevalence is 30% in patients over 75 years of age. It affects 9.3% of white Americans and 7.4% of African Americans.”
Emergence and presentation of suffering
Degeneration of the retinal pigment epithelium (RPE) leads to deposits in Bruch’s membrane, which separates the RPE from the choroid. Drusen form and the photoreceptors atrophy. Known risk factors include age, genetics (e.g., the incidence is lower in dark-skinned people), smoking, circulatory diseases (blood pressure, blood lipids), strong UV light, and the wrong diet. The condition can be classified into a dry and an exudative (moist) form:
Dry form: The dry form accounts for approximately 80% of all AMD cases. It is associated with drusen, pigmentary shift of the RPE, and RPE atrophies. The progression is slow and takes years. This is also one of the most typical characteristics of dry AMD. The transition to the exudative form is possible.
Wet form: The exudative (wet) form accounts for approximately 20% of all AMD. It is associated with choroidal neovascularization (CNV), which may be joined by pigment epithelial detachment, cystoid macular edema, hemorrhages, or end-stage fibrosis. The factor VEGF is significantly involved in this process. In most cases, this form is accompanied by severe vision loss within weeks to months. Therefore, therapy should be sought as soon as possible, which also means that patients with wet AMD should be identified and referred to an ophthalmologist as soon as possible. If left untreated, wet AMD rapidly leads to severe and often irreversible visual loss.
Specifically, AMD presents with symptoms such as metamorphosia (distorted lines), visual acuity loss (difficulty reading), loss of contrast sensitivity, and central relative or absolute scotoma. Diagnosis is based on the distance visual acuity test, presentation of the so-called Amsler net, ophthalmoscopy, fluorescence angiography (pathological vessels show leakage due to the disturbed blood-retinal barrier) and optical coherence tomography (OCT).
Ways of therapy
A minor protective effect in the dry form is provided by vitamins C and E, lutein, omega-3 fatty acids, beta-carotene, zinc and copper oxide. Treatment of the exudative form is primarily with anti-VEGF drugs (e.g. Lucentis®), applied intravitreally via the pars plana. In addition, there is photodynamic therapy with photosensitizer (e.g. Visudyne®), thermal laser photocoagulation or surgical procedures. Since the anti-VEGF drugs, which are very expensive but well effective and low risk, the latter three have become much less important. The anti-angiogenesis therapy with Lucentis
®
or Eylea
®
leads to an inhibition of the growth of proliferating choroidal blood vessels. These drugs should not be injected while the form is still dry.
“AMD is a disease of the retina with unknown cause, which occurs more frequently from the age of 50. The exudative form should be detected in time, self-examination using Amsler reticulation can be done regularly. Anti-VEGF therapy is the most effective here,” Dr. Eberhard summarized.
Drug therapy for osteoporosis in old age
Diana P. Frey, MD, Clinic for Rheumatology, University Hospital Zurich, spoke about the appropriate drug treatment for osteoporosis in old age. “Age is a significant risk factor for osteoporosis, which is why it is predominantly older people who need to be clarified and medically accompanied with regard to this condition. Multimorbidity and comedications are therefore central factors that must be taken into account,” said Dr. Frey, introducing her presentation. In osteoporosis that does not cause symptoms, patient compliance is often poor, especially if the intake regimen is complicated or, at best, if memory is diminished. Therefore, in elderly patients, simple, well-monitored regimens (parenteral agents administered in the office) are preferable to oral therapy. Taking multiple comedic medications may not only complicate the intake pattern of osteoporosis medications, but may also hinder absorption or lead to interactions.
Efficacy in older patient population
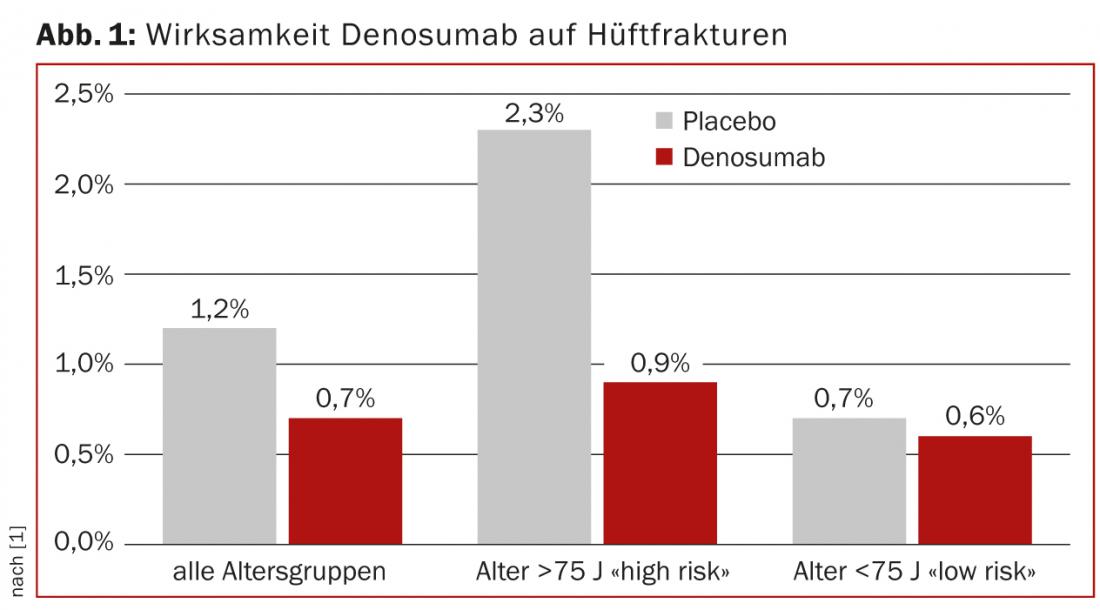
If the study population consisted of women, the majority of participants were postmenopausal, but often only a small number of very elderly patients were studied. For raloxifene, for example, there are no efficacy data in women over 70 years of age, which means that the substance should not be used in this population. Conversely, the effect of osteoporosis drugs tends to be better in principle with a higher fracture risk, which older people usually have with the same bone density, and thus the “number needed to treat” (NNT) is smaller. This has been demonstrated, for example, in the FREEDOM trial of denosumab (Prolia®) in a high-risk subgroup aged >75 years (Fig. 1) [1].
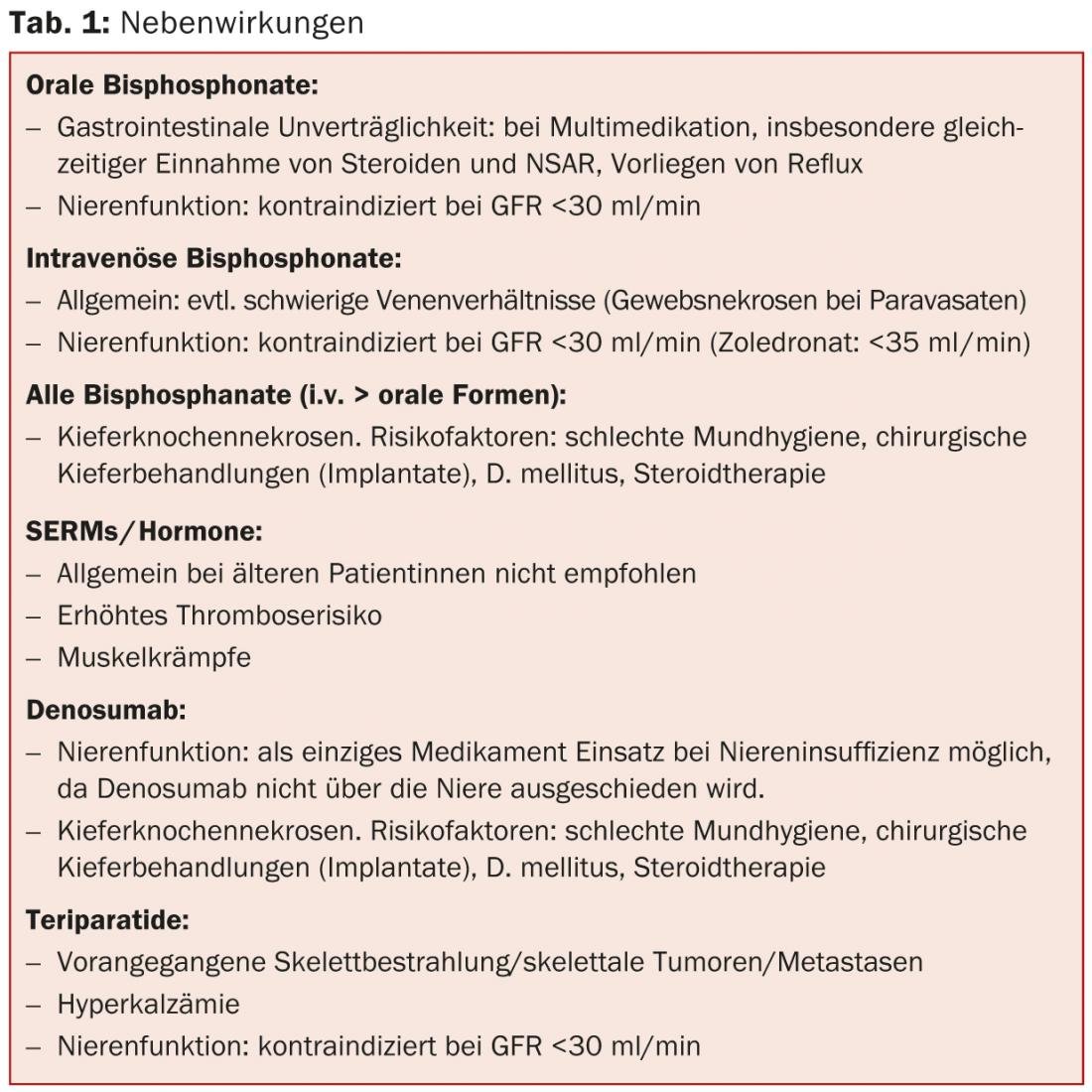
An overview of side effects to consider in the context of pharmacotherapy in the elderly is shown in Table 1.
Source: “Common impairments in old age,” seminar at Medidays, September 2-6, 2013, Zurich.
Literature:
- Boonen S, et al: Treatment with denosumab reduces the incidence of new vertebral and hip fractures in postmenopausal women at high risk. J Clin Endocrinol Metab 2011 Jun; 96(6): 1727-1736. doi: 10.1210/jc.2010-2784. epub 2011 Mar 16.
CONGRESS SPECIAL 2014; (6)1: 31-32











