There are some changes in the 2023 GOLD recommendations, one of which is the clear emphasis on dual bronchodilation (LABA/LAMA) [1]. For most COPD patients, starting treatment with a LABA/LAMA combination is standard, while the use of a mono-bronchodilator is the exception. Two experts from the GOLD Committee explained the background to the recommendation and the role of the eosinophil count in diagnostics and therapy.
Such exceptions to initial LABA/LAMA administration occur primarily in patients in whom the diagnosis was made by chance and who do not have a high symptom burden, explained Prof. Dr. Claus Vogelmeier, Head of the Department of Pulmonary Medicine at the Philipps University of Marburg (D) and member of the GOLD Committee [2]. Triple therapy with LABA/LAMA/ICS is suitable for patients who have already started a LABA/LAMA combination and develop further events that are considered exacerbations during this treatment. Especially if they have an eosinophil count of over 100 cells per microliter.
However, there may be exceptions to this rule: In a certain group of people who already have a pronounced history of exacerbation and high eosinophil counts >300 cells/μl at the outset, initial triple treatment should be considered. “This is because there are numerous studies that have shown that the higher the eosinophil count in the blood, the more likely it is that the additional administration of inhaled steroids will help to reduce exacerbations,” explained Prof. Vogelmeier.
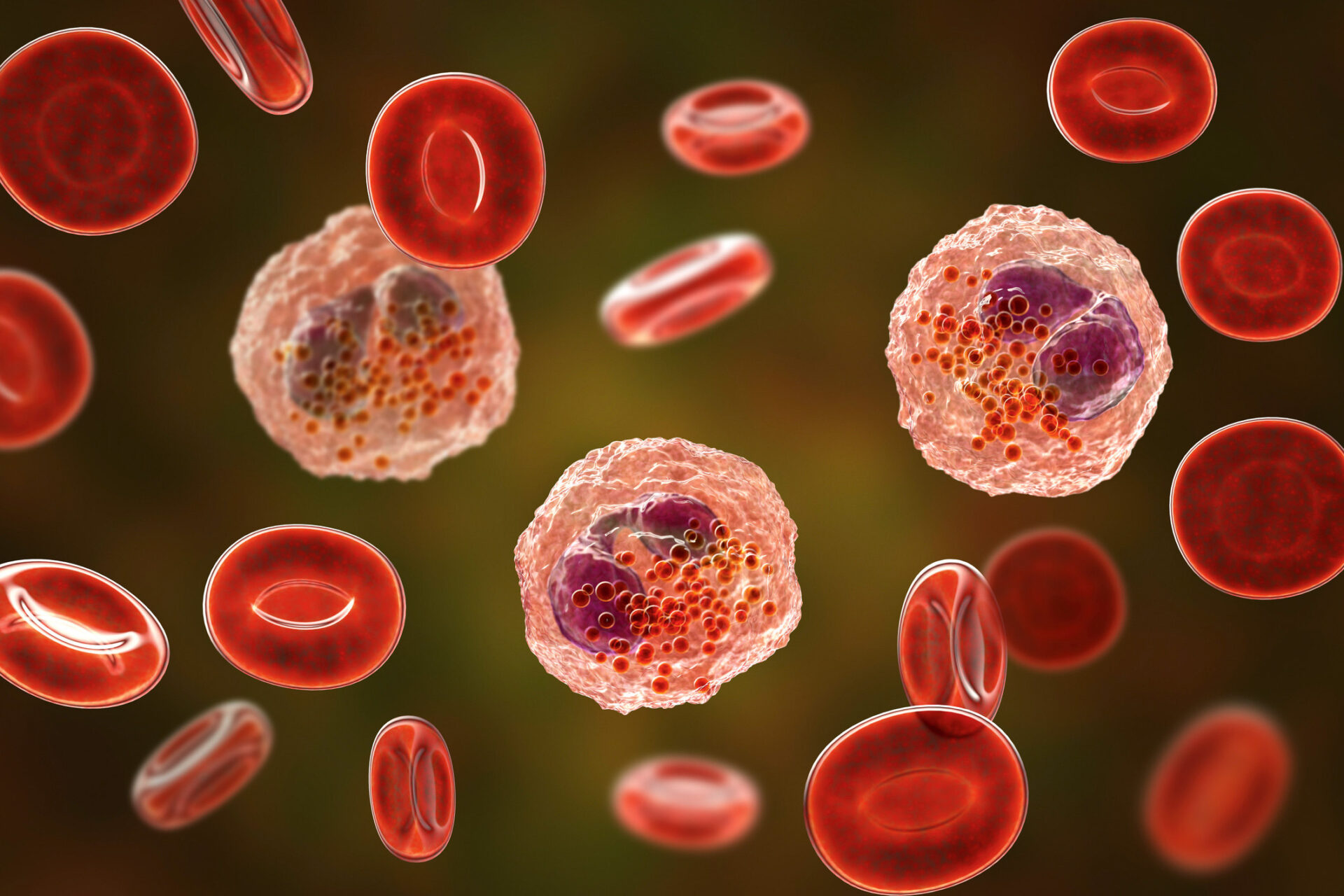
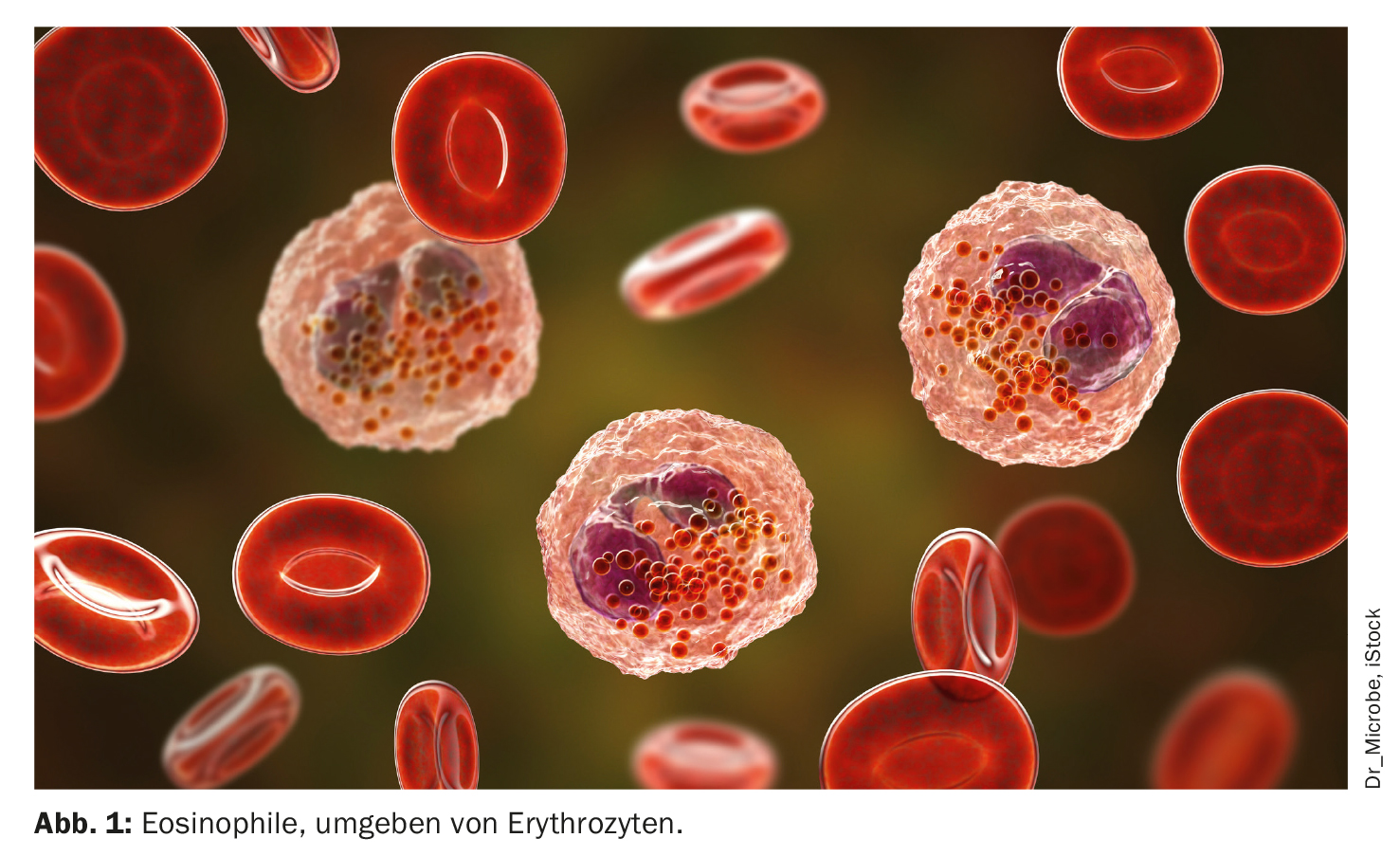
Eosinophils as biomarkers
Triple therapy is therefore better suited to preventing exacerbations than bronchodilators. “With regard to the threshold values, we know At a value of less than 100 (approximate value) there is no benefit for steroids. The further you get above 100, the greater the chance of a benefit. At 300, you are virtually certain that there is a benefit,” agreed Prof. Dr. Dave Singh, Clinical Pharmacology and Respiratory Medicine at the University of Manchester and also a member of the GOLD Committee, with his colleague [3].
| Significance of eosinophils and their values One problem in the treatment of COPD patients in everyday clinical practice is that the number of eosinophils in their blood can vary greatly (Fig. 1). Prof. Singh gave tips on the interpretation of the values and the therapeutic procedure and recommended a simple strategy. Some COPD patients have type 2 inflammation, which fluctuates from day to day. However, inflammation in humans will never be static. The expectation that the number of eosinophils in the blood will always be between 200 and 220, for example, will therefore not be fulfilled. Prof. Singh’s concept is: “Once you find signs of type 2 inflammation, that tells you that this patient has a tendency towards it. All the thresholds we give in GOLD are approximations. The estimated thresholds of 100 and 300 are not strict. If the patient has 320/μl today and 250/μl a week later, you don’t have to ask yourself what to do now. You treat a patient by looking at the pattern and trying to understand if that person has type 2 inflammation. So if the patient has 320/μl or 250/μl, they have type 2 inflammation. A practical approach might be to just use the highest value you’ve ever seen.” This is also how the expert proceeds in his practice, without performing repeat tests. Stable values should always be used to decide whether inhaled steroids should be used. In the case of exacerbations, measurement is not recommended, partly because oral steroids completely wipe out the eosinophil count in the blood and the measured value will be very low. However, there is also a group of patients without type 2 inflammation who have low eosinophil counts in their blood and whose values always remain very low: “They are almost always below 150 and their variability is low. This variability can actually say something: low variability and low values = no type 2 inflammation. High variability with occasionally high values – these are type 2 patients who will benefit from the inhaled steroid.” |
The reason for this relationship between blood eosinophil count and prediction of inhaled steroid benefit, according to Prof. Singh, is that people with higher eosinophil counts are more likely to have type 2 inflammation, and type 2 inflammation in COPD is different from that in asthma. The eosinophil count in the blood is therefore used to detect type 2 inflammation in the lungs and to say that an inhaled steroid – depending on the eosinophil count – is likely to be of benefit.
And what about eosinophils as a predictor of the risk of exacerbations? The more eosinophils are present, the more likely it is that the patient will suffer an exacerbation. The review articles on this topic contained very confusing statements, Prof. Singh pointed out. “The simple message is: I wouldn’t use it as a marker for exacerbation risk in clinical practice. There are better indicators, namely the history of exacerbations.” The clinical history should always be included in the assessment first and foremost: “The strongest predictor of the risk of future exacerbations is what has happened in recent years.”
ICS monotherapy without value
ICS mono, on the other hand, plays no role in the treatment of COPD. In the current GOLD recommendations, the use of a LABA/ICS combination is also no longer recommended, because if there is an indication for an ICS, a triple is superior to a LABA/ICS combination in terms of efficacy. With regard to the preventive use of LABA/LAMA, several studies have shown that they not only improve symptoms, lung function and quality of life, but can also reduce exacerbations. “There are therefore many good arguments for starting with LABA/LAMA combinations, not only for symptom control, but also to prevent events,” explained Prof. Vogelmeier.
Although there is evidence of some efficacy for LABA/ICS as initial therapy in COPD, numerous studies have shown that the triple combination is the better option in terms of several endpoints.
What to do if exacerbation continues under the triple
If a patient still has symptoms during triple therapy, there are no further options for escalation. One can only consider changing either the drug combination and/or the device, and of course non-pharmacological measures should also be considered. The expert also reminded the patient to think about differential diagnoses that could be relevant to the patient’s symptoms.
However, there are other options with regard to exacerbations: “We have roflumilast, a selective phosphodiesterase 4 inhibitor (PDE4i), which is not often used due to gastrointestinal side effects. We also have azithromycin, which can have effects on the QT time and hearing, among other things. So if the patient develops further exacerbations during triple treatment, they need to be evaluated very carefully in order to consider further steps.” Inhaled PDE4 inhibitors are in development – they have the potential to have the same efficacy but fewer side effects. However, this is still at an early stage of development.
Prof. Vogelmeier referred to a study that was presented at the ATS Congress in Washington DC in May 2023: According to the study, some patients who have persistent exacerbations and high eosinophils could be eligible for treatment with the anti-IL-4/13 antibody dupilumab, as this could have a positive effect on the exacerbation rate in addition to the triple or over and above the triple treatment. Dupilumab would therefore be the first biologic to show a clear effect in a subgroup of COPD patients.
Biologics for mucus congestion?
It has been shown that there is a strong correlation between mucus plugs in the airways and the risk of mortality. Similar findings have already been made in the treatment of asthma, where it has been shown that mucus congestion can be eliminated through the use of biologics. Comparable studies should now be carried out for COPD. A particularly interesting aspect identified by Prof. Vogelmeier was that more than half of the people in whom this mucus congestion was detected in the CT scans showed no symptoms of current bronchitis. It is therefore not enough to rely on the clinical presentation.
Sources:
- Global Initiative for Chronic Obstructive Lung Disease (GOLD): Global Strategy for Prevention, Diagnosis and Management of COPD: 2023 Report.
https://goldcopd.org/2023-gold-report-2. - Vogelmeier C: Pharmacological management of COPD. ERS Vision Live – New concepts in COPD; 5.7.2023.
- Singh D: Role of eosinophils as biomarkers in COPD. ERS Vision Live – New concepts in COPD; 5.7.2023.
InFo PNEUMOLOGY & ALLERGOLOGY 2023: 5(4): 26-27