In view of the increasing variety of treatment options, the question of criteria for psoriasis therapy specifically tailored to patient characteristics is coming into focus. A Belgian expert panel has issued recommendations for systemic psoriasis therapy regarding comorbidities and psoriasis subtypes. These were published in this year’s Journal of EADV.
The therapeutic arsenal for the treatment of psoriasis has multiplied within a relatively short time and is now the largest of all inflammatory skin diseases. While this opens up new perspectives for patients, it has made the choice of therapy optimally tailored to individual clinical characteristics very challenging for the treating physician. Patient characteristics such as age, weight, or comorbidities may have an impact on the efficacy of therapy and/or the risk of adverse events. However, considering the immense flood of publications, it is difficult to have an overview of all current clinically relevant study results.
“Belgian Evidence-based Treatment Advice in Psoriasis.”
Against this background, the Royal Belgian Society of Dermatology and Venerology launched the BETA-PSO project (“Belgian Evidence-based Treatment Advice in Psoriasis”), the results of which were recently published in the Journal of the European Academy of Dermatology and Venerology (JEADV) [1]. The primary objective of the work was to establish an evidence base for practice guidelines on the systemic treatment of psoriasis. The evidence-based recommendations were developed using the Quasi-Delphi method. The procedure included the formulation of clinical questions about the treatment of psoriasis and a systematic literature search. Specific recommendations were then generated by a panel of 8 psoriasis experts based on a rating of the data. The results are intended to be a decision support for the clinical practice for the choice of an adequate psoriasis therapy. According to the authors, the study results provide valuable guidance for dermatologists worldwide on contemporary psoriasis treatment.
Included interleukin antagonists
|
Expert consensus according to the quasi-Delphi methodology
During a day-long face-to-face meeting, the expert panel identified a list of 38 questions about real-life situations physicians often face when treating patients with psoriasis in their clinics. Each expert was assigned a unique topic to summarize based on a systematic search of the literature in PubMed. Included were articles published in the past 5 years on randomized controlled trials, case-control studies, observational studies, systematic reviews, meta-analyses, and case reports on systemic psoriasis therapy (conventional, synthetic, and biological). Data was included that provided information on the following aspects:
- Influence of metabolic comorbidities on therapy or vice versa.
- Effects of treatment on specific forms of psoriasis (nail psoriasis, erythrodermic psoriasis, pustular psoriasis)
- Does the patient have a history of treatment with biologics or is he biologics-naïve?
- Influence of age on therapy results and use of certain drugs
- Effects of treatment on mental health
Results at a glance
The following active substances used for the systemic treatment of psoriasis were considered:
- Conventional Antipsoriatics: Acitretin, cyclosporine, dimethyl fumarate, methotrexate.
- synthetic drugs: Apremilast
- Biologics: adalimumab, certolizumab pegol, etanercept, infliximab, ustekinumab, guselkumab, risankizumab, tildrakizumab, brodalumab, ixekizumab, secukinumab
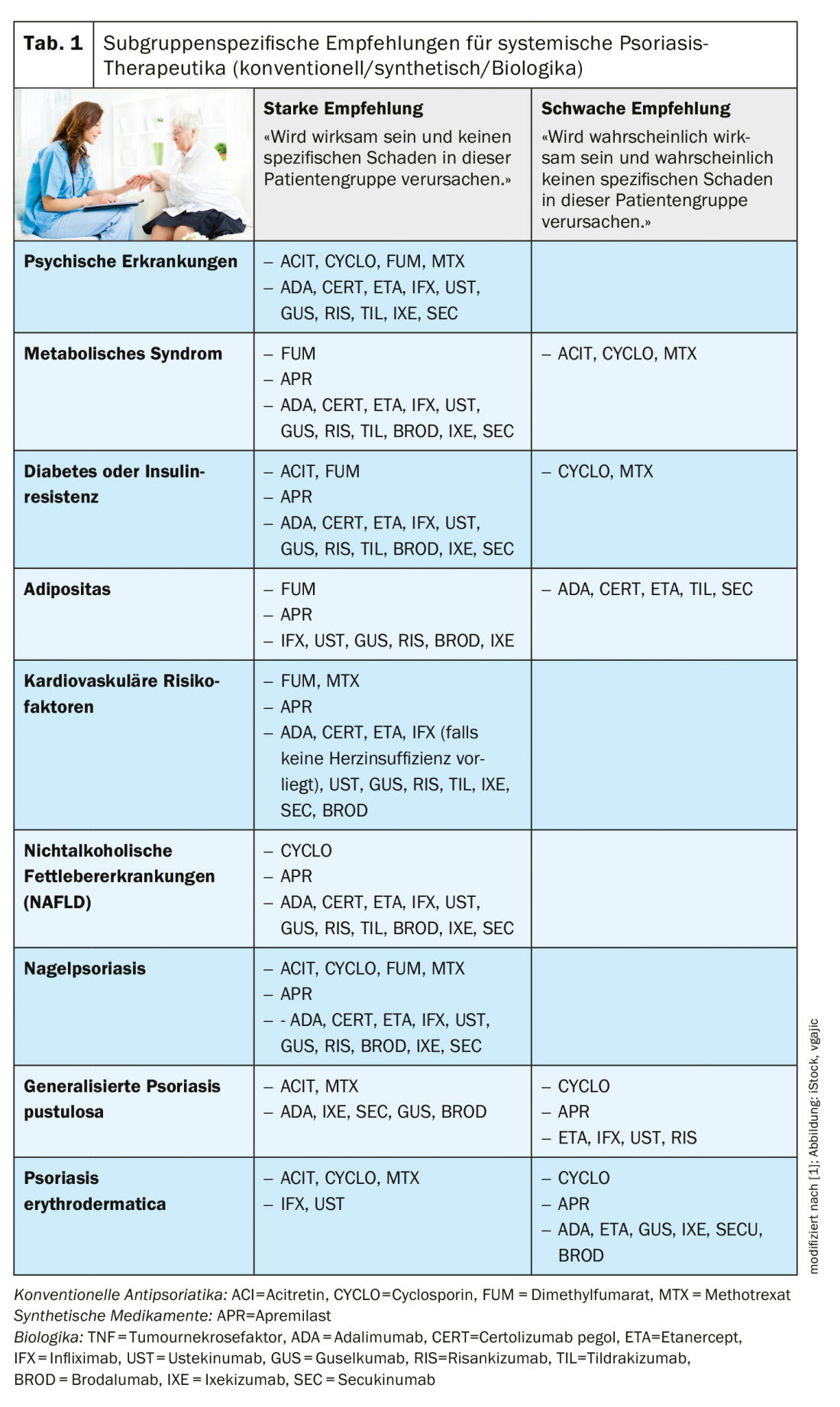
Which agents are recommended for which of the above five groups of patient characteristics is shown in Table 1. The following are some supplementary notes on individual of the criteria:
- Influence of metabolic comorbidities on therapy or vice versa: In psoriasis patients with metabolic syndrome, careful monitoring and follow-up is recommended, including control of weight, blood pressure, triglycerides, HDL cholesterol, and glucose levels. There is an ongoing debate about the effects of different agents on clinical manifestations of the metabolic syndrome. In obese psoriasis patients treated with biologics, the diet/weight control factor should be addressed, as the efficacy of biologic therapy may be affected [2]. If conventional systemic therapeutics are used with a weight-based dosing regimen, caution should be exercised with methotrexate and cyclosporine due to an increased dose-dependent risk of renal or hepatic toxicity. For psoriatics with type 2 diabetes and/or insulin resistance, the authors note that meaningful clinical recommendations are difficult due to a lack of comparative studies. Cyclosporine and methotrexate may be used, but special caution should be exercised when using these agents. In patients at cardiovascular risk, it should be noted that cyclosporine and acitretin are associated with an increased risk of hypertension and dyslipidemia, although there is no contraindication if these potential side effects are adequately managed.
- If the patient has a history of biologic therapy or is biologic-naïve: There are data that patients who have had at least one prior biologic therapy show better drug survival when switching between different classes of biologics as opposed to switching within the same class [3]. However, this is put into perspective when the factors of efficacy, side effects, and comorbidities are included. In this regard, there is evidence that switching within the same class of biologics may also be a good option if it can increase efficacy [4]. According to current data, it is less important for the newer biologics whether a previous therapy attempt with another biologic was unsuccessful [5].
- Effects of treatment on mental health: patients with psoriasis are more affected by depression, anxiety disorders, suicidality, loss of confidence, sleep disturbances, and reduced quality of life, and it is known that these symptoms can be reduced by effective treatment [6]. The expert panel therefore advises to initiate adequate effective treatment as soon as possible. For example, in one large study, biologic therapy was associated with a reduction in antidepressant use [7,8].
Literature:
- Lambert JLW, et al: Practical recommendations for systemic treatment in psoriasis according to age, pregnancy, metabolic syndrome, mental health, psoriasis subtype and treatment history (BETA-PSO: Belgian Evidence-based Treatment Advice in Psoriasis; part 1). JEADV 2020; 34(8): 1654-1665.
- Al-Mutairi N, Nour T: The effect of weight reduction on treatment outcomes in obese patients with psoriasis on biologic therapy: a randomized controlled prospective trial. Expert Opin Biol Ther 2014; 14: 749-756.
- Cozzani E, et al: Serial biologic therapies in psoriasis patients: a 12-year, single-center, retrospective observational study. J Am Acad Dermatol 2019; 82: 37-44.
- Kimmel G, et al: Brodalumab in the treatment of moderate to severe psoriasis in patients when previous anti-interleukin 17A therapies have failed. J Am Acad Dermatol 2019; 81: 857-859.
- Wang TS, Tsai TF: Biologics switch in psoriasis. Immunotherapy 2019; 11: 531-541.
- Gordon KB, et al: Anxiety and depression in patients with moderate-to-severe psoriasis and comparison of change from baseline after treatment with guselkumab vs. adalimumab: results from the phase 3 VOYAGE 2 study. JEADV 2018; 32: 1940-1949.
- Wu CY, et al: Depression and insomnia in patients with psoriasis and psoriatic arthritis taking tumor necrosis factor antagonists. Medicine (Baltimore) 2016; 95: e3816.
- Strober B, et al: Depressive symptoms, depression, and the effect of biologic therapy among patients in Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Am Acad Dermatol 2018; 78: 70-80.
DERMATOLOGY PRACTICE 2020; 30(4): 20-22