The treatment of type 2 diabetes mellitus has undergone a transformation in recent years with the approval of new drug classes. The focus is no longer on pure glycemic control, but on holistic therapy management. This includes, above all, the reduction of cardiovascular risk factors. In this respect, the updated treatment recommendations take into account current developments and study data.
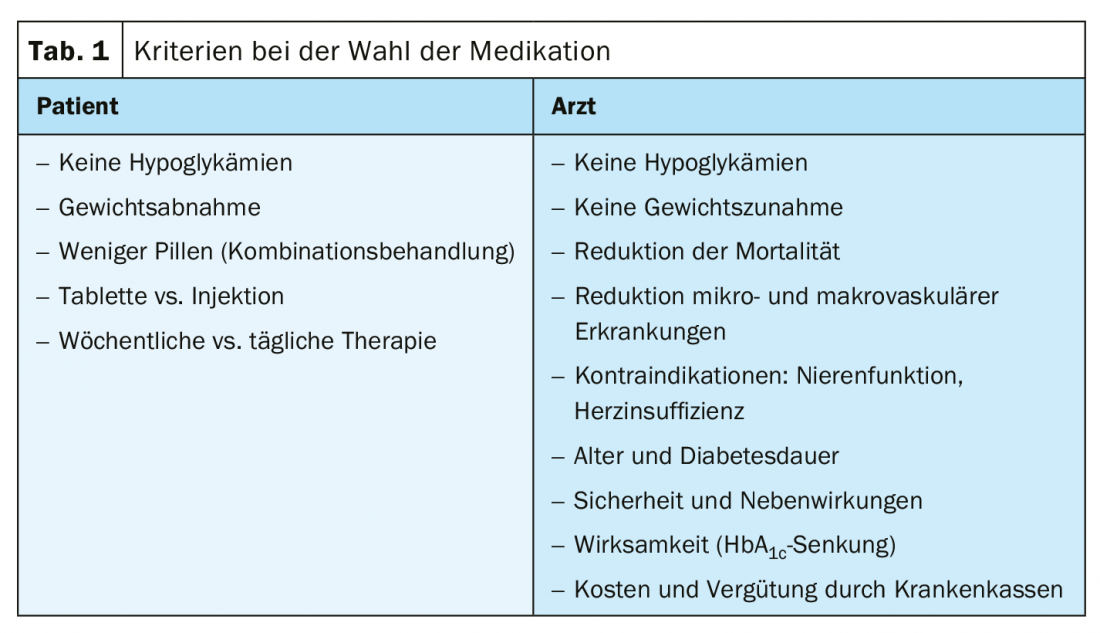
The central theme of previous treatment strategies for type 2 diabetes (T2D) was glycemic control. However, numerous new antidiabetic drugs now enable a holistic therapy concept. This takes cardiovascular risk factors in particular into account, explained Prof. Roger Lehmann, MD, Zurich, during a FomF WebUp. This aspect is even more important since two-thirds of all patients with T2D (63%) die of cardiovascular causes. In addition to hypertension, T2D is primarily associated with coronary artery disease and heart failure. As the expert pointed out, 6.4% of the Swiss suffer from T2D. 25-50% of these have comorbid cardiovascular disease, and 25% of patients have heart failure. 40% of those with T2D and heart failure also develop chronic kidney disease. Therefore, the goal of effective treatment is to address comorbidities in addition to good management of the underlying disease. “Of course, a well-controlled HbA1c level is still essential to avoid microvascular and macrovascular complications,” Lehmann said. Without sulfonylureas and/or insulin, the stated goal should be <7.0%. For patients with significant comorbidities and/or advanced age and insulin requirement, aim for <8.0%. Both the patient’s and the physician’s preferences should play a role in choosing the appropriate preparation (Table 1).
Nearly every T2D patient is at cardiovascular risk
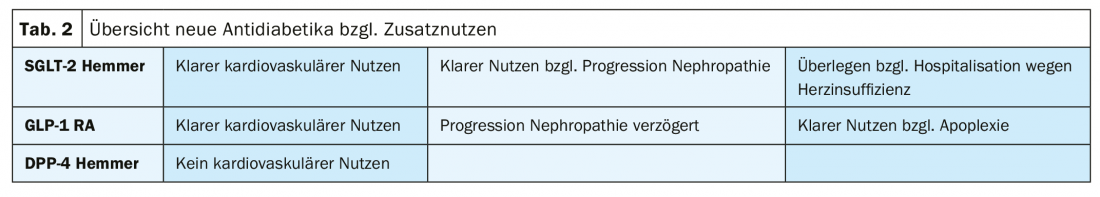
Looking at the cardiovascular risk categories, it is striking that virtually no T2D patient falls under the “moderate risk” aspect. This is because only young patients <50 years of age with diabetes duration <10 years and no risk factors are included. Patients with a disease duration ≥10 years without organ damage and moderate renal insufficiency (eGFR 30-59 ml/min) or another risk factor are already at high risk. A very high cardiovascular risk is brought by patients with diabetes who have established cardiovascular disease or other organ damage, or at least three risk factors. With this in mind, the FDA has required cardiovascular endpoint studies for all new diabetes drugs since 2008. Accordingly, GLP-1 receptor agonists (RA), SGLT-2 inhibitors, and DPP-4 inhibitors were also studied in terms of MACE scores (nonfatal apoplexy, nonfatal myocardial infarction, and cardiovascular death) (Table 2). In particular, GLP-1 RA and SGLT-2 inhibitors cover many pathophysiological defects in T2D, the expert reported. These include lowering blood pressure, blood sugar, and weight, as well as slowing gastric emptying, reducing appetite, and reducing inflammation. An increase in glucose-dependent insulin secretion in the GLP-1 RA and a reduction in oxidative stress, vascular stiffness, and increase in glucose excretion in the SGLT-2 inhibitors are also observed.
Multifactorial therapy management
The treatment of a T2D is always multifactorial in nature. Very important above all is the motivation to change lifestyle. In addition, smoking should be stopped and hypertension and lipids should be included in therapy management. The most important characteristics of T2D include possible insulin deficiency, renal function (eGFR), and therapy or prevention of heart failure (Fig. 1) . They are needed as a basis for the appropriate therapy regime. Metformin is still considered a first-line diabetes drug if eGFR >30 ml/min. However, this should be combined early – preferably with a GLP-1 RA or SGLT-2 inhibitor. However, if insulin deficiency is present, basal insulin administration is indicated. Especially with typical symptoms such as weight loss, polyuria, polydipsia as well as a very high Hba1c >10%.

Combination therapies
Prof. Lehman gave a short insight into current study data and at the same time an outlook on possible future therapy options. He looked more closely at the combinations of metformin with GLP-1 RA and SGLT-2 inhibitors or those of the two new agents (Fig. 2) . There were clear advantages in MACE, prevention of severe hypoglycemia, and mortality.
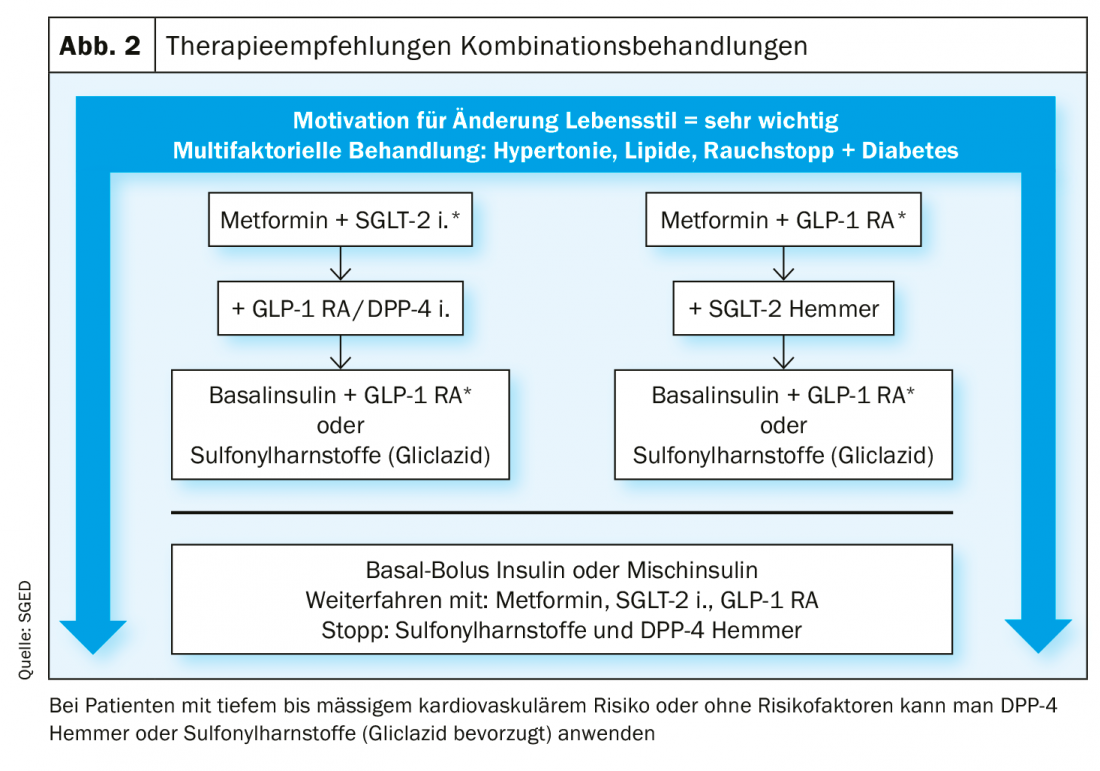
For example, the 5-year follow-up of a Danish cohort demonstrated an 82% reduction in mortality for triple therapy with metformin + SGLT-2 inhibitor + GLP-1 RA. However, the other treatment regimens with the new antidiabetic drugs also scored well. Metformin in combination with an SGLT-2 inhibitor reduced mortality by 70%. When metformin was combined with a GLP-1 RA, the reduction was 59%. If basal insulin was also given, the reduction increased to 62%.
Source: “The new recommendations of the Swiss Society of Endocrinology and Diabetology for the treatment of type 2 diabetes mellitus”, 09.04.2020, FomF WebUp.
Further reading:
- www.sgedssed.ch/fileadmin/user_upload/6_Diabetologie/61_Empfehlungen_Facharzt/2020_Swiss_Recomm_Medis_DE_def.pdf (last accessed 05.05.2020)
- Hasselstrom Jensen M, Kjolby M, Hejlesen O, et al: Risk of Major Adverse Cardiovascular Events, Severe Hypoglycemia, and All-Cause Mortality for Widely Used Antihyperglycemic Dual and Triple Therapies for Type 2 Diabetes Management: A Cohort Study of All Danish Users. Diabetes Care 2020.
HAUSARZT PRAXIS 2020; 15(6): 20-22
CARDIOVASC 2020; 19(2): 24-25