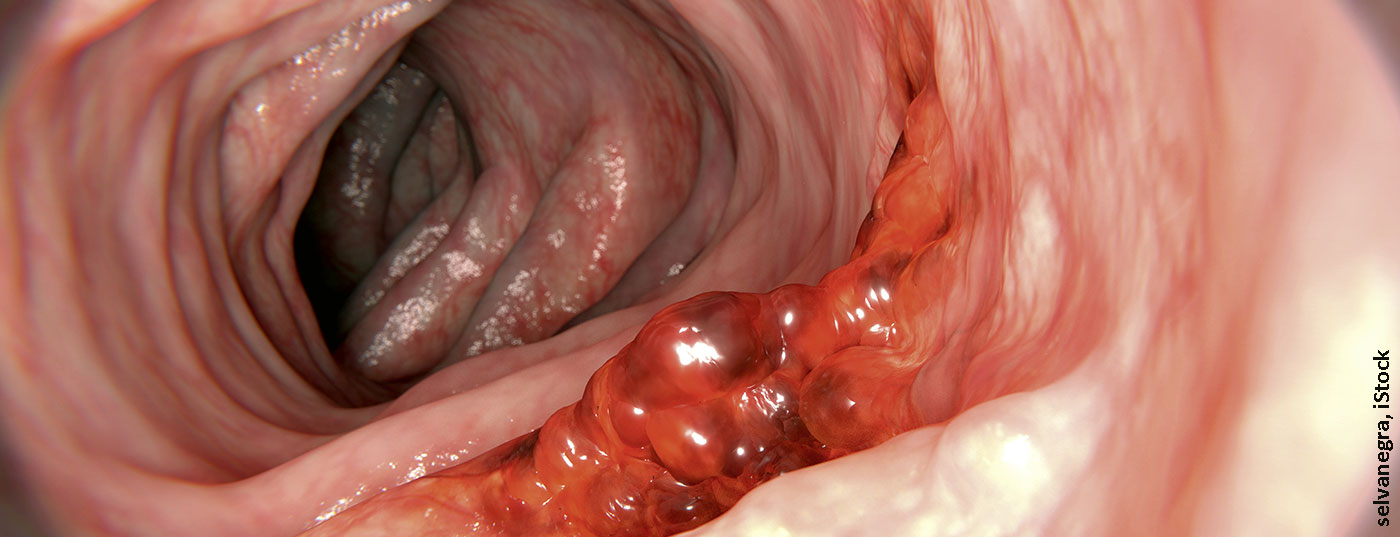
This year’s ASCO brought exciting study results to light. Especially in tumors of the upper and lower gastrointestinal tract, there were developments, some of which had practice-changing potential. In metastatic colon cancer, there were new insights regarding therapy sequence and intensity, and the importance of immunotherapy in tumors with and without microsatellite instability.
Targeted treatment strategies are becoming increasingly important in metastatic colorectal cancer (mCRC). Attention was drawn to the results of the phase III PARADIGM trial comparing panitumumab (PAN) plus mFOLFOX6 or bevacizumab (BEV) plus mFOLFOX6 in patients with chemotherapy-naïve RAS wild-type (WT) mCRC. The primary endpoint was overall survival (OS) in patients with left-sided tumors and in the overall population. Secondary endpoints were progression-free survival (PFS), response rate (RR), and R0 resection rate. 802 patients received either PAN-based or BEV-based treatment in a 1:1 ratio and were followed up for an average of 61 months. PAN was found to significantly improve OS compared to BEV. A significant OS benefit of 3.6 months (37.9 months vs. 34.3 months) was detected in patients with left-sided tumors. For the secondary endpoints, no difference in PFS was observed between the two treatment groups. The rate of response and R0 resection was again higher in the PAN clientele. Accordingly, the combination of PAN with mFOLFOX6 should be established as the new standard for first-line combination therapy in patients with RAS-WT and left-sided mCRC.
In mCRC sufferers with RAS and BRAF wild-type, a chemotherapy doublet (FOLFOX/FOLFIRI) is standard. It was now investigated whether the addition of an anti-EGFR monoclonal antibody (cetuximab or panitumumab) would be useful. For this, 435 patients were treated with either 12 cycles of mFOLFOXIRI plus PAN or 12 cycles of mFOLFOX6 plus PAN, each followed by 5-FU/LV plus PAN until progression. The primary endpoint was defined as the objective response rate (ORR). No significant difference was observed here between the two treatment arms. Disease control rate and tumor shrinkage were also comparable. Accordingly, intensification of chemotherapy does not appear to confer any advantage in treatment management.
Immunotherapy shows sustained survival benefit
Therapy-naïve patients with mCRC tumors and high microsatellite instability (MSI-h) are usually treated with the checkpoint inhibitor pembrolizumab. For pretreated affected individuals, dual immunotherapy with nivolumab (NIVO) plus ipilimumab (IPI) is the standard of care. 5-year follow-up data demonstrate clear benefits for the combination. Patients with dMMR/MSI-h-mCRC were divided into three cohorts until disease progression or the onset of unacceptable toxicity. Be received either NIVO 3 mg/kg Q2W, NIVO 3 mg/kg + IPI 1 mg/kg Q3W (4 doses), followed by NIVO 3 mg/kg Q2W, or first-line NIVO 3 mg/kg Q2W + IPI 1 mg/kg Q6W starting in the second line. The ORR was 39%, 65%, or 71%. The 48-month PFS rates were 36%, 54%, and 51%, and the corresponding 48-month OS rates were 49%, 71%, and 72%.
At 60 months follow-up, PFS rates of 34% and 52% were achieved, respectively. Cohort 3 had not yet reached median follow-up. OS rates were 46% and 68%, respectively. No new safety signals appeared. Therefore, for dual immunotherapy, the solid and persistent PFS and OS benefit was substantiated.
Immunotherapeutic regimens are also being investigated in tumors that do not exhibit microsatellite instability. This is usually a combination of chemotherapy and checkpoint inhibitor. When nivolumab was added to FOLFOXIRI/bevacizumab as first-line therapy in patients with RAS-mutated or BRAF-mutated mCRC regardless of MSS or MSI-h status, promising remission was observed in the MSS group. The ORR was 78.9% and the median duration of response was 7.6 months with an mPFS of 9.8 months. The addition of atezolizumab to the induction treatment regimen of FOLFOXIRI plus bevacizumab versus FOLFOXIRI/bevacizumab alone in mCRC regardless of MSS or MSI-h status was compelling with significantly longer mPFS in the PD-L1 inhibitor arm at 13.1 months vs. 11.5 months. Treatment-refractory MSS-mCRC was treated with avelumab in combination with cetuximab and irinotecan. An initial interim analysis showed that for patients with RAS wild-type, the primary efficacy endpoint of tumor response was met. Encouragingly, 12-month OS was comparable in both RAS wild-type and RAS-mutated tumors, 46.2% vs. 38.5%, respectively.
Congress: ASCO 2022
InFo ONCOLOGY & HEMATOLOGY 2022, 10(4): 26.