Basic therapy, UV light therapy, implementation of skin disinfection and other measures can lead to relief from neurodermatitis. Regarding climatic therapy, it has been shown that a reduced allergen concentration above 1500 m contributes to symptom reduction. Behavioral therapy has been shown to be effective for reducing psychosocial distress.
Treatment of atopic dermatitis includes both drug and non-drug therapies. In the following mini-review, the latter approach will be presented, explicitly refraining from presenting alternative medical offerings.
Individual provocation factors
An identification of individual provoking factors for the development and maintenance of atopic eczema should be aimed at. In addition to allergens, skin-irritating factors such as wearing wool, working in a humid environment (e.g. hairdresser, florist, etc.), contact with dirt particles (e.g. motor vehicle mechanic), climatic (e.g. sultriness), hormonal (e.g. pregnancy, menstruation) and psychological factors (such as stress) may play a role here [1,2]. After identification, attempts must be made to reduce or completely eliminate the influence of the identified factor (e.g., encasing measures for house dust mite allergy sufferers with neurodermatitis).
Basic therapy
Although few studies are available in this regard, the restoration and maintenance of the skin barrier through the repeated application of refatting topicals appears to be of particular importance [3]. The exact mechanism of how lege artis basic therapy can prevent a new episode of atopic eczema is not known. It is believed that by reducing transepidermal water loss and increasing hydration, subclinical skin barrier disruption and early stages of inflammation can be corrected [4]. Within the framework of step therapy, the application of topical therapy adapted to the skin condition with oily ointment bases on dry skin or hydrating oil-in-water emulsions on less dry skin is of great importance. Common contact allergens should not be incorporated into basic therapeutics.
A pilot study and two randomized controlled trials demonstrated that postpartum daily whole-body ointment treatment (e.g., with Cetaphil® Moisturizing Cream, Eucerin® Aquaphor Skin Care Ointment) reduced the cumulative incidence of atopic dermatitis in high-risk infants by 30-50% [4–6].
Skin disinfection
Superantigens from Staphylococcus aureus isolates of lesional atopic dermatitis skin are able to inhibit the activity of regulatory T lymphocytes, which are responsible for the body’s own fight against inflammation. This fact may explain why untreated superinfections induce exacerbations or prolongations of existing atopic dermatitis disease [7].
In addition to antibiotics, other antimicrobial preparations are available in the germ-loaded neurodermatitis patient. Chlorhexidine-containing preparations (e.g. Vita-Hexin® Ointment) have bactericidal properties against Gram-positive and Gram-negative bacteria and are virucidal and fungicidal. Feared adverse effects represent chlorhexidine keratitis [8] and anacusis after affection of the middle ear [9].
Triclosan-containing topicals (such as Lipo Sol Lotion® Widmer) have antibacterial and antifungal properties.
As a lipophilic polychlorinated phenol, triclosan is not without controversy in topical application and is capable of inducing local exacerbation of the skin lesion, especially at higher concentrations [10]. There are also reports of resistance developments to bacteria [11].
Occasionally, the beneficial effect of bathing with Javel water (aqueous sodium hypochlorite solution) or applying a wash lotion containing sodium hypochlorite (e.g., CLn® Body Wash, USA) on atopic eczema has been reported [12]. The antimicrobial efficacy of sodium hypochlorite against bacteria, viruses and spores, which has been known for many decades, is emphasized without the risk of resistance development. The minimum bactericidal concentration of sodium hypochlorite by topical application for Staphylococcus aureus is 0.006%, 0.0015% for Streptococcus pyogenes, and 0.003% for Pseudomonas aeruginosa [13]. In contrast, the Federal Office of Public Health does not consider its use to be harmless and points out the possibility of cutaneous burns or burns [14].
Clothing fabrics coated with silver nitrate or a quaternary ammonium compound exhibit antimicrobial activity. Wearing such underwear may be considered in chronic atopic dermatitis [1]. The addition of silk underwear (such as Derma Silk®) to children and adolescents with atopic eczema failed to provide any additional clinical or economic benefit over guideline-based atopic dermatitis therapy in a randomized, controlled, observer-blinded, parallel-group study [15].
Phototherapy
The rational for the use of UV light treatment in atopic eczema lies in its anti-inflammatory effects on antigen-presenting Langerhans cells, infiltrating T cells, and proinflammatory cytokines (IL12, IL2, interferon alpha, TNF alpha), among others [16–18]. A recently published analysis of randomized controlled trials provided evidence of benefit from UVB narrow-spectrum treatment of atopic dermatitis in adults [19].
In addition to the UVB 311-nm range, irradiation sources for UVA1 and UVB broadband as well as balneo-phototherapy are available. It is adjuvant in acute phases of disease and may be considered in individuals >12 years of age. The use of long-wavelength light (>380 nm) is not recommended in the absence of controlled studies [1,18,19].
Immunoadsorption/extracorporeal photopheresis
Smaller published case series suggest improvement of severe atopic dermatitis disease under these therapeutic modalities. They are used in selected cases, e.g. when ciclosporin and other immunosuppressants remain without effect, are not tolerated or are contraindicated [1].
Climatherapy
Efficient climatic therapy appears to be useful only in climates with pronounced irritant factors. Effects due to the climate itself must be separated from effects due to therapy in the climate [20]. The first institutions to use climate-therapeutic effects as part of their therapy concept were Heiligendamm/Doberan on the Baltic Sea (1794) and Norderney in the North Sea (1797) [20].
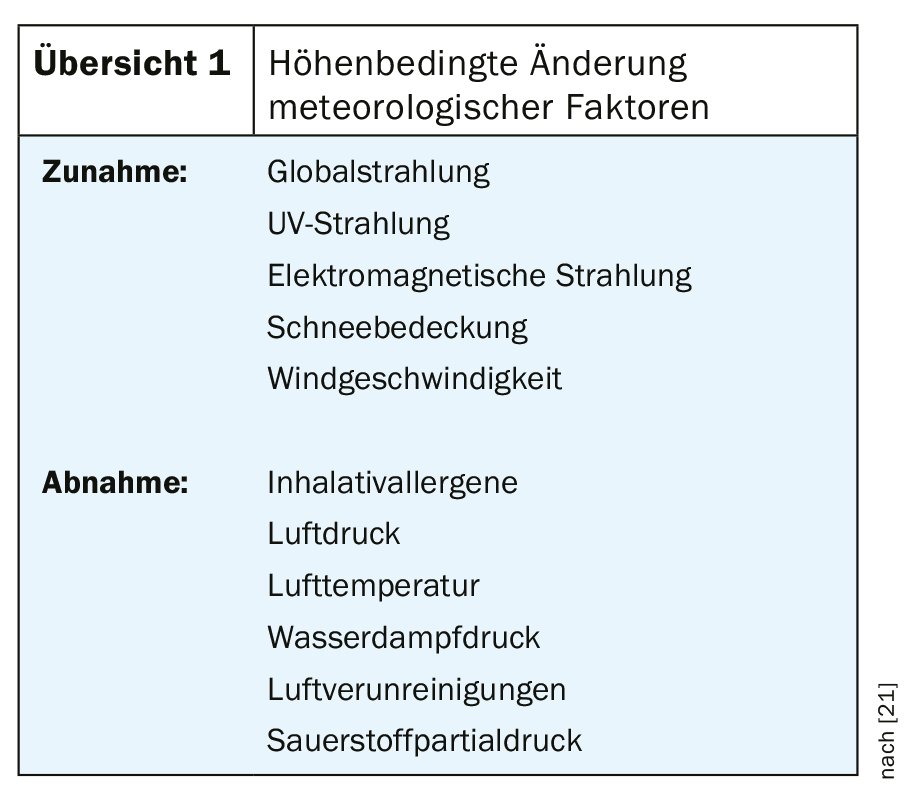
In Davos, which is located at 1600 m above sea level (hanger picture), the physician Luzius Ruedi (1804-1869) founded a first medical institution for the treatment of children in the 19th century. Depending on the altitude, there are changes in significant environmental parameters (Overview 1).
The special radiation climate in the high mountains – with increase of daily sunshine duration above 800 m in autumn and winter, higher global radiation and intensity increase of the wavelength range of 290 and 350 nm, which is significant for dermatotherapy – can be used in the form of heliotherapy almost all year round. Even with cloud-covered skies, a therapeutically usable residual radiation still reaches the exposed skin-suffering patient [20].
A lowered oxygen partial pressure, as it exists in the high mountain climate compared to the lowlands, causes a circulation activation, a deepening of the respiration as well as an improvement of the skin blood circulation, which is used therapeutically.
Reduced humidity at altitude leads to increased evaporation through the skin, a resulting reduction in skin temperature (“evaporative cooling”) and a reduction in itching. Furthermore, the lack of sultriness in the high mountain climate leads to reduced sweat and heat stress on the skin organ.
The protected high mountain valley location of Davos is also held responsible for the fact that a reduced number of infectious pathogens – compared to lower-lying regions – can be detected there [20]. The often considerable distance from the place of residence or work also has positive effects on the psyche and skin.
Above 1500 meters of altitude it can be assumed that the house is free of dust mites. Other potent allergens (e.g. birch and grass pollen, mold spores) are significantly reduced in concentration as well as in the duration of their occurrence or are almost completely absent. Interestingly, Samedan, which is located higher than Davos, shows higher values with respect to the annual pollen sum. This is associated with relatively more unfavorable site conditions of Samedan (such as increased aerogenic pollen supply due to meteorological and geographic features) [21].
Neurodermatitis training
A structured interdisciplinary training for children and guardians with chronic and chronic-recurrent atopic dermatitis according to a predefined curriculum has proven successful abroad (e.g. Germany: AGNES) [1]. This assessment is supported by a recent comprehensive review of randomized controlled trials [19]. Still to be clarified is the exact definition of the components that make up a successful training program [19].
Elimination diet
Neurodermatitis diets” have been widely studied in children and adults with the disease [22]. Dietary intervention in patients with atopic dermatitis is warranted only when the recency of food allergy has been established [1,18]. Evidence for general elimination diets resulting in a beneficial effect on atopic eczema has not been generated to date [23]. Nevertheless, at least one in five neurodermatitis sufferers tries to achieve an improvement in their skin condition via elimination diets or “special foods” without involving medical help [24]. Analyzing the dietary habits of adult atopic dermatitis patients, few differences are found with control groups adjusted for sex and age [25]. Among the few differences in dietary habits between atopic dermatitis sufferers and skin-healthy individuals, a slightly increased sugar consumption in male subjects with atopic eczema stood out. Regrettably, a sugar-free diet did not improve atopic dermatitis symptoms [26].
Probiotics
These include living microorganisms, which are supposed to have health-promoting effects for humans. In addition to supporting food digestion, they are also said to be able to influence local and general immunity. Thus, for certain strains of Lactobacillus and Bifidobacteria, there is evidence for a favorable modification of immunological processes [27]. Several meta-analyses from 2008 failed to demonstrate a significant reduction in eczema symptoms with probiotics versus placebo [28,29].
A meta-analysis published in 2014, however, found a significant reduction of the SCORAD value after probiotics intake in atopic dermatitis patients who were older than one year. Here, a mix of different bacteria or Lactobacillus species was superior to Bifidobacterium species [30].
The 2016 guideline does not provide justification for the administration of probiotics for a beneficial effect on the severity and course of atopic eczema [1].
Prebiotics
Prebiotics are found in foods and dietary supplements and contain indigestible components that stimulate the growth of non-pathogenic bacteria [22]. Data on the influence of prebiotics on atopic eczema are scarce. A small randomized trial failed to show that prebiotics alone lead to SCORAD decline [31].
Synbiotics
The administration of probiotics and prebiotics in combination (“synbiotics”) may possibly lead to a favorable influence on atopic eczema [32]. Further studies with larger numbers of cases must follow here to allow a definitive classification of synbiotic administration.
Vitamin D
Supplementation with vitamin D cannot currently be recommended for atopic dermatitis. It is possible that in subpopulations (e.g., lowered blood vitamin D levels, bacterial superinfections), administration may lead to a favorable influence on atopic dermatitis [33]. Further studies must take place here before a valid recommendation can be made.
Essential fatty acids
A reduced delta-6-desaturase activity is found in neurodermatitis, which was the starting point for supplementation studies with essential fatty acids. The majority of these were unable to demonstrate any positive effects for atopic eczema. Therefore, oral administration of borage, evening primrose and fish oil and topical application of fatty acids (such as gamma-linolenic acid) are currently not recommended in atopic dermatitis [33].
Chinese herbal medicine
Due to insufficient data, Chinese herbal medicine cannot currently be recommended for the treatment of atopic eczema [33].
Psychological treatment
Distressing psychological complaints can grow up during a neurodermatitis disease or be causative for the development of the skin lesion. Behavioral therapy approaches, in particular, have shown efficacy in atopic eczema in controlled trials. Both individual psychological trigger factors and secondary psychosocial consequences for the affected person or his or her family environment are important in this context [1].
Take-Home Messages
- The use of basic therapy, UV therapy, skin disinfection and other measures can alleviate existing neurodermatitis.
- Regarding climatic therapy, a reduced allergen concentration above 1500 m may contribute to symptom reduction.
- Behavioral therapy has been shown to be effective for reducing psychosocial distress.
- Without therapeutic benefit in the neurodermatitis therapy remain glucose abstinence, fish oil administration as well as some further measures.
Literature:
- Werfel T, et al: S2k guideline on diagnosis and treatment of atopic dermatitis – short version. J Dtsch Dermatol Ges 2016; 14: 92-106.
- Langan SM, et al: What causes worsening of eczema? A systematic review. Br J Dermatol 2006; 155: 504-514.
- Ng JP, et al: Use of emollients in atopic dermatitis. J Eur Acad Dermatol Venereol 2015; 29: 854-857.
- Simpson EL, Chalmers JR, Hanifin JM, et al: Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol 2014; 134: 818-823.
- Horimukai K, et al: Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol 2014; 134: 824-830.
- Glatz M, et al: Emollient use alters skin barrier and microbes in infants at risk for developing atopic dermatitis. PLOS 2018; 13: e0192443.
- Gould HJ, et al: The allergic march from Staphylococcus aureus superantigens to immunoglobulin E. Chem Immunol Allergy 2007; 93: 106-136.
- Steinsapir KD, Woodward JA: Chlorhexidine keratitis: safety of chlorhexidine as a facial antiseptic. Dermatol Surg 2017; 43: 1-6.
- Lai P, et al: Chlorhexidine ototoxicity in ear surgery, part 1: review of the literature. J Otolarygol Head Neck Surg 2011; 40: 437-440.
- Wohlrab J, et al: Antiseptic efficacy of a low-dosed topical triclosan/chlorhexidine combination therapy in atopic dermatitis. Skin Pharmacol Physiol 2007; 20: 71-76.
- Yazdankhah SP, et al: Triclosan and antimicrobial resistance in bacteria: an overview. Microb Drug Resist 2006; 12: 83-90.
- Ryan C, et al: Novel sodium hypochlorite cleanser shows clinical response and excellent acceptability in the treatment of atopic dermatitis. Ped Dermatol 2013; 30: 308-315.
- Coetzee E, et al: The use of topical, un-buffered sodium hypochlorite in the management of burn wound infection. Burns 2012; 38: 529-533.
- Anonymous: Federal Office of Public Health FOPH > Healthy Living > Environment and Health > Chemicals > Chemicals from A – Z > Javel water (06.01.2020).
- Thomas KS, et al: Silk garments plus standard care compared with standard care for treating eczema in children: a randomised, controlled, observer-blind, pragmatic trial (CLOTHES Trial). PLoS Med 2017 14: e1002280.
- Majoie IM, et al: Narrowband ultraviolet B and medium-dose ultraviolet A1 are equally effective in the treatment of moderate to severe atopic dermatitis. J Am Acad Dermatol 2009; 60: 77-84.
- Gambichler T: Management of atopic dermatitis using photo(chemo)therapy. Arch Dermatol Res 2009; 301: 197-203.
- Wollenberg A, et al: Consensus-based European guidelines for treatmemt of atopic eczema (atopic dermatitis) in adults and children: Part I. J Eur Acad Derm Venerol 2018; 32: 657-682.
- Nankervis H, et al: What is the evidence base for atopic eczema treatments? A summary of published randomized controlled trials. Br J Dermatol 2017; 176: 910-927.
- Engst R, Vocks E: High mountain climate therapy for dermatoses and allergies – mechanisms of action, results and immunological parameters. Rehabilitation 2000; 39: 215-222.
- Gehrig R, Peeters AG: Pollen distribution at elevations above 1000 m in Switzerland. Aerobiologica 2000; 16: 69-74.
- Finch J, et al: Atopic dermatitis and nutrition. Clin Dermatol 2010; 28: 605-614.
- Bath-Hextall F, et al: Dietary exclusions for improving established atopic eczema in adults and children: systematic review. Allergy 2009; 64: 258-264.
- Jensen P: Use of alternative medicine by patients with atopic dermatitis and psoriasis. Acta Derm Venereol 1990; 70: 421-424.
- Solvoll E, et al: Dietary habits among patients with atopic dermatitis. Eur J Clin Nutr 2000; 54: 93-97.
- Thestrup-Pedersen K: Treatment principles of atopic dermatitis. J Eur Acad Dermatol Venereol 2002; 16: 1-9.
- Prescott SL, Björksten B: Probiotics for the prevention of or treatment of allergic diseases. J Allergy Clin Immunol 2007; 120: 255-262.
- Lee J, et al: Meta-analysis of clinical trials of probiotics for prevention and treatment of pediatric atopic dermatitis. J Allergy Clin Immunol 2008; 121: 116-121.
- Michail SK, et al: Efficacy of probiotics in the treatment of pediatric atopic dermatitis: a meta-analysis of randomized controlled trials. Ann Allergy Asthma Immunol 2008; 101: 508-516.
- Kim SO, et al: Effects of probiotics for the treatment of atopic dermatitis: a meta-analysis of randomized controlled trials. Ann Asthma Allergy Immunol 2014; 113: 217-226.
- Shibata R, et al: Clinical effects of ketose, a prebiotic oligosaccaride on the treatment of atopic dermatitis in infants. Clin Exp Allergy 2009; 39: 1397-1403.
- Chang YS, et al: Synbiotics for prevention and treatment of atopic dermatitis: a meta-analysis of randomized controlled trials. JAMA Pediatr 2016; 170: 236-242.
- Schlichte MJ, et al: Diet and eczema: a review of dietary supplements for the treatment of atopic dermatitis. Dermatol Pract Concept 2016; 6: 23-29.
DERMATOLOGY PRACTICE 2020; 30(1): 10-13











