With optical coherence tomography and confocal laser scanning microscopy, state-of-the-art high-tech methods are available for the non-invasive diagnosis of non-melanocytic skin cancer and melanoma. Both methods are painless for patients and another advantage is that the data and findings are delivered in real time. Laser-based technologies that can be used in dermatology are constantly being developed further, one example being “linefield confocal” optical coherence tomography.
The earlier skin cancer is detected, the better the chances of cure. In diagnostics, non-invasive methods are increasingly used in addition to clinical inspection and dermoscopy. This significantly reduces the amount of examination required for the diagnosis of suspicious skin lesions. Modern noninvasive techniques that allow overall assessment of lesions using optical cross-sectional imaging include confocal laser microscopy and optical coherence tomography.
Confocal laser scanning microscopy: in vivo and ex vivo methods
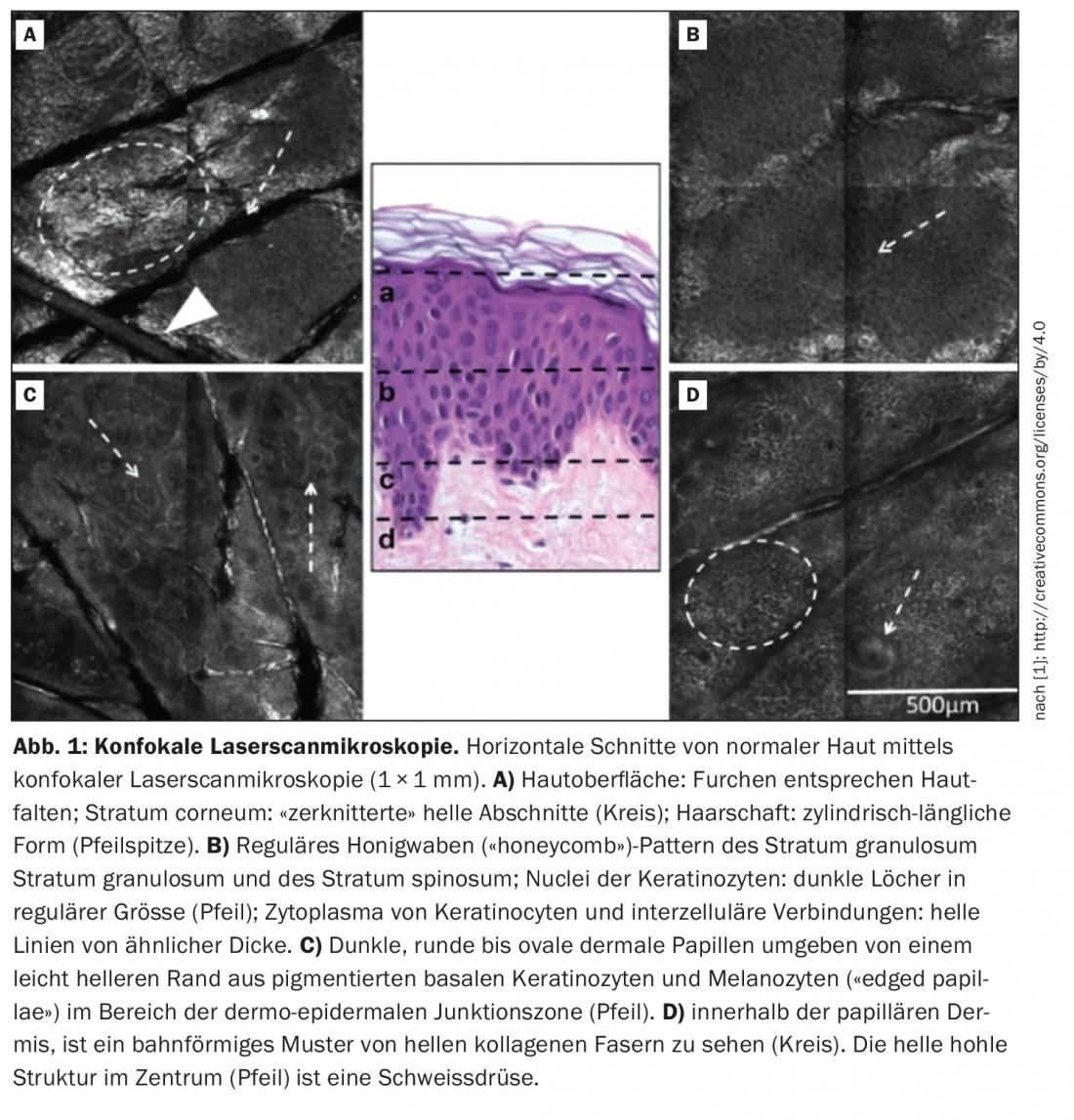
Confocal laser scanning microscopy (Fig. 1) can be used to reliably and painlessly examine skin cells below the skin surface for malignant changes [1]. This gives patients the fastest, most reliable diagnosis currently available for skin cancer and its precursors. In the English literature, confocal laser scanning microscopy is referred to as “reflectance confocal microscopy”. Regarding the diagnosis of basal cell carcinoma, confocal laser microscopy was shown to have a sensitivity of 100% and a specificity of 88.5% in a multicenter study [2]. The 2020 updated guidelines on malignant melanoma refer to a recent meta-analysis on confocal laser microscopy in the evaluation of malignant skin tumors [3,4]. In 8 of the 21 studies, only melanomas were investigated. A total number of 1400 lesions could be evaluated. In these studies, sensitivity was 92.7% [95% CI: 90-95] and specificity was 78.3% [95% CI: 76-81] [3]. Confocal laser microscopy uses devices with one or more lasers as the light source, which can be used for both in vivo and ex vivo examination of the skin [2]. PD Dr. med. Daniela Hartmann, LMU Munich, reported on the indication spectrum of ex vivo confocal laser scanning microscopy for bedside histology on the occasion of the skin cancer congress of the Arbeitsgemeinschaft Dermatologische Onkologie (ADO) [5]. While in vivo laser scanning microscopy can be used to take optical noninvasive biopsies of skin lesions, the ex vivo method is an ultrafast direct-intraoperative fluorescence examination of freshly excised tissue, PD Dr. Hartmann explained. Depending on the device, one has at least two laser wavelengths available, as well as different fluorescent dyes. The optical vertical sections as known from histology are produced within 2-3 minutes. An important innovation for everyday practice is digital HE staining(box). There are now numerous studies on the use of ex vivo confocal laser scanning microscopy in Mohs surgery. In particular, for basal cell carcinomas, it was confirmed that laser scanning microscopy is firstly much faster and that thanks to the fluorescence of the cell nuclei of the basal cell carcinoma, the tumor parts are easier to find.
|
Confocal laser scanning microscopy (ex-vivo) with digital HE staining The newly introduced digital color processing of images mimics conventional hematoxylin-eosin (HE) staining almost perfectly and is very well suited to diagnose basal cell carcinomas and their cut margins even under routine conditions [9]. Thus, this method represents a tissue-saving alternative to cryostat rapid sectioning. It is expected that further developments such as slides with magnetic fixations to optimize contact pressure will further improve the accuracy of the findings. |
Optical Coherence Tomography
Optical coherence tomography (OCT) is an imaging technique that uses lasers to scan all layers of the human skin. The basis of optical coherence tomography is white light interferometry. This involves comparing the transit time of a signal within the tissue sample to a reference signal of known optical path length. The examination method allows a penetration depth of up to one millimeter and a resolution of 15 µm. In addition to the early detection of skin tumors and the avoidance of unnecessary biopsies, according to Sandra Schuh, MD, University Hospital Augsburg, Germany, support in therapy selection (surgery vs. topical treatment) and therapy monitoring are among the main applications of optical coherence tomography in routine diagnostics [5]. Regarding the detection of basal cell carcinoma, the use of OCT increases the accuracy compared to clinical and dermoscopic diagnosis as shown in a study with 164 patients and 235 lesions: the specificity could be increased from 29% to 75% by using OCT [6]. According to the current guideline, optical coherence tomography is suitable for thickness measurement of basal cell carcinomas up to a thickness of about 1 mm and allows a preoperative estimation of the extent of a basal cell carcinoma by visualizing the lateral borders [7].
|
Linefield confocal OCT: new, non-invasive procedure Line-field confocal optical coherence tomography is an innovative method that allows cellular resolution and penetration depth down to the deep dermis, so that not only the morphology but also the depth of invasion of numerous tumors can be determined by it [10]. Using this laser-based technology, 3-D images of the skin are possible in real time. For the diagnosis of BCC, linefield confocal OCT is a great device, said Cristel Ruini, MD, LMU Munich [5]. The first larger study describing morphologic criteria related to diagnosis and subtype classification of BCC was published in 2020 in JEADV by Suppa et al. Published [11]. |
Several studies are also available on OCT for the evaluation of melanocytic lesions, describing potential differentiation criteria. In a multicenter prospective study on an HD-OCT system, a total of 93 lesions (27 of which were melanomas) were examined [8]. A sensitivity of 74.1% [95% CI: 54-89] and a specificity of 92.4% [95% CI: 83-98] were achieved [3].
Congress: German Skin Cancer Congress 2021
Literature:
- Ahlgrimm-SiessV, et al: Confocal Microscopy in Skin Cancer. Curr Derm Rep 2018; 7: 105-118.
- S1 Guideline: Confocal laser microscopy in dermatology, 2017, AWMF Registry Number: 013/076, www.awmf.org/uploads/tx_szleitlinien/013-076l_S1_Konfokale_Lasermikroskopie_der_Haut_2017-08.pdf, (last accessed 11/23/2021).
- S3 guideline on diagnosis, therapy, and follow-up of melanoma, 2020, AWMF registry number: 032/024O, www.awmf.org/uploads/tx_szleitlinien/032-024OLl_S3_Melanom-Diagnostik-Therapie-Nachsorge_2020-08.pdf (last accessed Nov. 23, 2021).
- Xiong YD, et al: A meta-analysis of reflectance confocal microscopy for the diagnosis of malignant skin tumours. J Eur Acad Dermatol Venereol 2016; 30(8): 1295-1302.
- “Imaging and physical diagnosis of skin cancer – from the new world”, WS4, 31st German Skin Cancer Congress, Sept 07, 2021.
- Ulrich M, et al: The sensitivity and specificity of optical coherence tomography for the assisted diagnosis of nonpigmented basal cell carcinoma: an observational study. Br J Dermatol 2015; 173(2): 428-435.
- S2k guideline: basal cell carcinoma of the skin, AWMF registry number: 032-021, www.awmf.org/uploads/tx_szleitlinien/032-021l_S2k_Basalzellkarzinom-der-Haut_2018-09_01.pdf, (last accessed 11/23/2021).
- Gambichler T, et al: A multicentre pilot study investigating high-definition optical coherence tomography in the differentiation of cutaneous melanoma and melanocytic naevi. J Eur Acad Dermatol Venereol 2015; 29(3): 537-541.
- Grupp M, et al: Sectional margin control of basal cell carcinomas by ex vivo confocal laser scanning microscopy with digital color processing – application in routine diagnostics. J Dtsch Dermatol Ges 2021; 19(5): 685-693.
- Ruini C, Sattler E: Confocal line-field OCT: the eggshell? Current Dermatology 2020; 46(04): 148-151.
- Suppa M, et al: Line-field confocal optical coherence tomography of basal cell carcinoma: a descriptive study. J Eur Acad Dermatol Venereol 2021; 35(5): 1099-1110.
DERMATOLOGIE PRAXIS 2021; 31(6): 32-33 (published 12/3/21, ahead of print).