Often a combination of different treatment methods achieves the best results. Ablative laser procedures can be used, among other things, for “laser-assisted drug delivery” – active substances can be introduced via the ablation channels created in the scar tissue in a minimally invasive and painless manner. Non-ablative lasers result in remodeling of dermal collagen and elastin and also lead to improvement in the appearance of scars.
Due to the variety of causes, manifestations and therapeutic options, scar correction is a very complex field. Within the broad treatment spectrum, newer procedures are becoming increasingly established. Lorenzo Pelloni, MD, dermatologist at the Ospedale Regionale Bellinzona e Valli and active in his own private practice in Lugano, reported on the use of various laser technologies [1]. In his presentation, the speaker focused on the topic of fractional laser procedures. In fractional photothermolysis, the laser light is applied by means of a special laser head through a (fractionated) laser beam divided into many thousands of individual light columns. This enables a treatment with few side effects but effective at the same time. The goals of scar treatment include reducing functional and aesthetic limitations. While hypertrophic scars are limited to the original size of the wound, scar keloids progressively grow beyond it (box) [3,4].
| Hypertrophic scars vs. keloids At the pathogenetic level, keloid formation is the result of a dysbalance of increased synthesis of collagen and extracellular matrix and decreased degradation of these products. There is research evidence to suggest that the clinical differences between keloids and hypertrophic scars simply reflect differences in the intensity, frequency, and duration of inflammation of the reticular dermis. According to this, they were successive stages of one and the same condition, namely fibroproliferative skin diseases, and keloids could be defined as severely inflamed, and hypertrophic scars as mildly inflamed pathological scars [3,4]. |
Scar evaluation: which scale to use?
In addition to inspection and palpation, there are well-established structured assessment procedures that have been developed to evaluate scar tissue. Dr. Pelloni said he mostly uses the Vancouver Scar Scale (VSS) [1,5]. This scale considers the following criteria to evaluate scars: Vascularization, height or thickness, suppleness and pigmentation. A new score, which was presented in a 2022 publication, is the Keloid Area and Severity Index (KASI) [1,6]. Analogous to the PASI in the field of psoriasis or the EASI for atopic dermatitis, the extent and severity of the scars are calculated on the basis of various criteria. Since a relatively large number of parameters are involved, the whole thing is somewhat more complicated than the VSS, but apps may be offered in the future that take over the calculation of the score, the speaker conceded. Therapeutic goals should be determined individually and should be based on the patient’s symptoms [2].
“Time matters” – Don’t miss the window for laser therapy
The two pillars in the management of keloids and hypertrophic scars are prevention and early treatment, Dr. Pelloni emphasized. Whereas only in the case of postoperative wounds (partial or complete wound healing disorder after primary surgical wound closure) can preventive action be taken by appropriate techniques, but not in the case of burn injuries or post-traumatic wounds (chronic soft tissue wounds as a result of direct penetrating or blunt trauma with associated necrosis of epithelial and non-epithelial extraskeletal structures). For the treatment of traumatic scars and their contractures, laser medical applications are considered first-line therapy – this is stated in the international consensus recommendations published in 2020 [7]. To optimize the risk-benefit ratio, laser treatment should be used as early as possible. 90% of the expert panel advocated starting laser therapy within one month of injury for minor traumatic injuries and 70% within one week of injury. In a 2018 systematic review published in JEADV, significant improvement in scars was seen in 3 of 4 studies when laser treatment was initiated in the inflammation phase, whereas when laser therapy was initiated in the proliferation phase or remodeling phase, this was the case in 6 of 16 and 2 of 5 studies, respectively [13]. Among others, the following laser methods were investigated: PDL, KTP, Er:YAG and fractionalCO2 laser. In 18 of the 25 included studies, 2-4 laser treatments were performed at intervals of 2 to 8 weeks, whereas in seven studies only one laser treatment was performed. Follow-up time ranged from 1 to 12 months, with 18 studies having a follow-up time ≤3 months.
Er:YAG orCO2 laser for ablative fractional laser treatment
Ablative fractional lasers can be used to remove tissue in a controlled and safe manner. The principle of fractional photothermolysis can achieve effective neocollagenesis with minimal downtime and good tolerability compared with classical ablative procedures [8]. Alone or in combination with “laser-assisted drug delivery” (LADD) (Fig. 1) , improvement in one or more scar aspects (itching, redness, firmness, pigmentation, or thickness) is usually achieved [2]. The most commonly used fractional lasers are Er:YAG andCO2. Since the energy of the Er:YAG laser is strongly absorbed by water due to its wavelength, there is very little heat distribution in the surrounding tissue, whereas theCO2 laser shows significant heating of the surrounding tissue and leads to coagulation of small blood vessels [9]. The speaker described the case of a patient in whom, after a burn in the arm area, treatment with fractionalCO2 laser resulted in improvement of texture, color and contracture after 3 sessions within 2 months. In addition, the movement restrictions of the arm decreased.
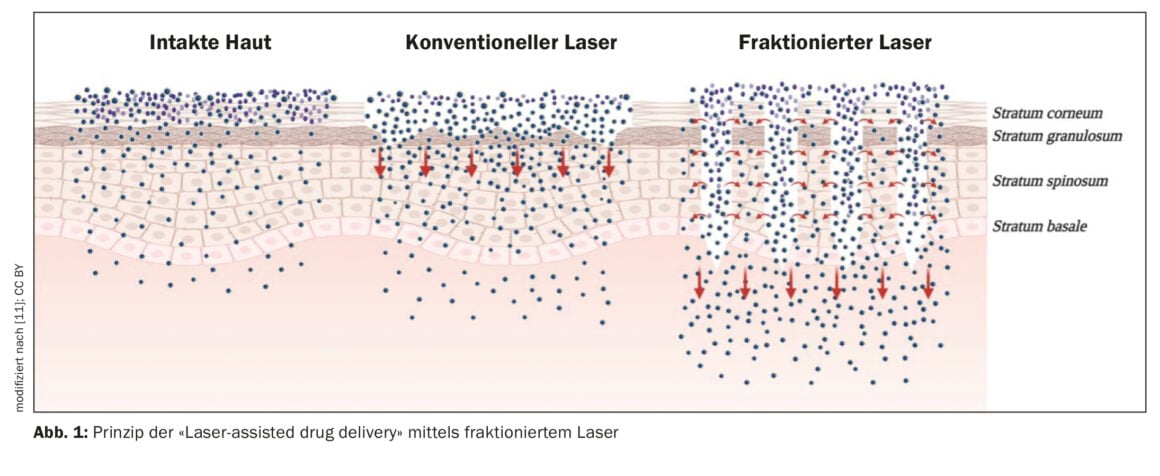
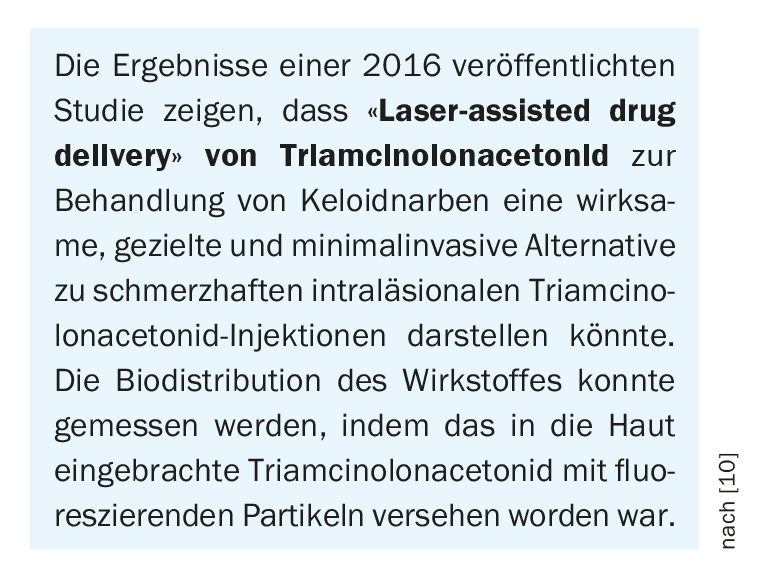
The fact thatCO2 and Er:YAG lasers produce cylindrically shaped microablation zones in the skin allows topical agents to penetrate to the dermis without the need for injection [10]. For example, externally applied triamcinolone acetonide can be introduced.
“Laser-assisted drug delivery” for the treatment of hypertrophic scars.
The technique of “laser-assisted drug delivery” has been used by the speaker, among others, on a 70-year-old woman who had hypertrophic scars in her arms due to a burn from hot water. After treatment with fractional Er:YAG laser (without anesthesia), triamcinolone solution (40 mg/ml) was applied to the corresponding areas. He said it is important to do this within 20-30 minutes of laser application for optimal effectiveness. This procedure is not painful, the speaker explained. After that, a plastic patch could be applied for 8-12 h for occlusion and then the patient could be asked to apply a silicone gel twice a day until the next session. After 2 sessions with Er:YAG laser plus triamcinolone solution, the patient was very satisfied with the result, especially the redness had decreased significantly.

Scar reduction with non-ablative fractional laser
Non-ablative laser procedures allow heat to reach deep tissue layers without affecting the integrity of the epidermal barrier. In addition to remodeling of epidermal and dermal components, photothermolysis of the microvasculature in the dermis takes place. Collagen and hyaluronic acid metabolism is stimulated at the molecular level and the formation of elastic fibers is induced [12]. Migration of normal melanocytes at the edges of thermally coagulated tissue results in normalization of pigmentation [1,12]. The speaker illustrated that a significant improvement can be achieved, particularly with regard to skin redness, pigmentation and texture of the scar, using patients with burns and surgical scars.
Last, but not least: Pulsed dye laser
Finally, the speaker also discussed the use of pulsed dye laser ( PDL). The mechanism of action of dye lasers on the skin is based on selective photothermolysis, i.e. an adaptation of the pulse duration, energy density and wavelength to the respective target [12]. This creates microvascular damage, resulting in local hypoxia and catalyzing biochemical changes in the scar, among other effects [1]. The lecturer described the case of a patient with post-traumatic scars in the area of nose and forehead, in whom especially a significant improvement of erythematous aspects was achieved after treatment with PDL (6 sessions).
Congress: SGML23 Laser & Procedures
Literature:
- “Laser Management of Hypertrophic and Keloid Scars,” Lorenzo Pelloni, MD, SGML23 Lasers & Procedures, Jan. 23, 2023.
- Nast A, et al: S2k guideline therapy of pathological scars (hypertrophic scars and keloids) – update 2020 JDDG 2021; 19(2): 312-327.
- Huang C, et al: Int Wound J 2014; 11: 517-522.
- Ogawa R: Int J Mol Sci 2017; 18(3): 606.
- Sullivan T, et al: J Burn Care Rehabil 1990; 11(3): 256-260.
- Limmer EE, et al: Br J Dermatol 2022; 187(5): 799-800.
- Laser Treatment of Traumatic Scars and Contractures: 2020 International Consensus Recommendations.
- 8 Steckmeier S, et al: Current Dermatology 2017; 43(10): 418-426.
- Poetschke J, Gauglitz GG: JDDG 2016; 14(5): 467-478.
- Singhal M, et al: Mol Pharm 2016; 13(2): 500-511.
- Portugal I, et al: Pharmaceuticals (Basel) 2021; 14(8): 772.
www.mdpi.com/1424-8247/14/8/772/htm,(last accessed Jan. 25, 2023) - “Laser therapy of the skin,” S2k guideline, AWMF registry no: 013-095, 2022.
- Karmisholt KE, et al: JEADV 2018; 32(7): 1099-1110.
DERMATOLOGIE PRAXIS 2023; 33(2): 50-51 (published 4/20-23, ahead of print).