This year’s annual meeting of the American Association for Thoracic Surgery was held in Minneapolis. Prof Thierry Carrel presents his personal highlights.
Reduced anticoagulation after implantation of a mechanical aortic valve [1].
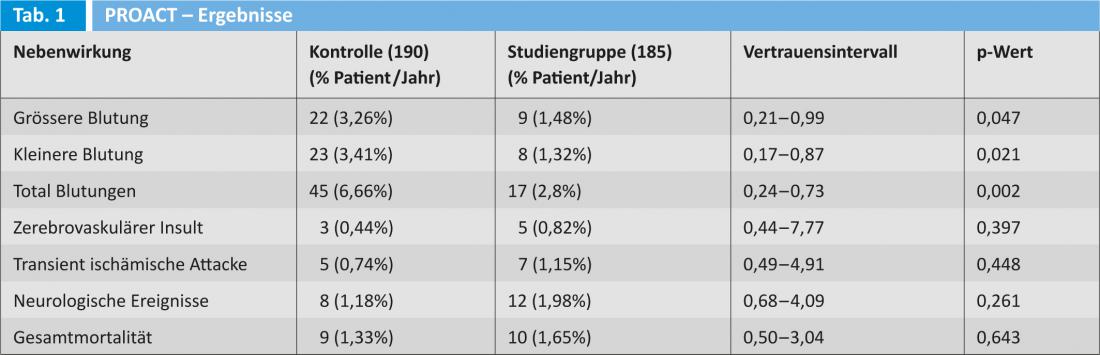
The prospective FDA PROACT trial investigated whether less aggressive peroral anticoagulation was more defensible than that recommended by the American Heart Association or the American College of Cardiology. The study was conducted in patients who received an ON-X aortic valve.
Patients at increased risk for thromboembolic events received warfarin with a target INR of 1.5-2.0 or 2.0-3.0 starting three months postoperatively. All patients received 81 mg aspirin and were allowed to monitor their INR themselves. The results are shown in Table 1.
The authors conclude that the INR in patients undergoing aortic valve replacement with a mechanical prosthesis can be adjusted in the 1.5-2.0 range in combination with low-dose aspirin; this results in a significant reduction in bleeding events without increasing the rate of thromboembolic events.
Single high-dose erythropoietin administration two days before cardiac surgery [2].
Several studies have shown that short-term administration of erythropoietin can significantly reduce the need for foreign blood transfusions. Previous protocols were based on a five-day administration and often resulted in compliance problems for treated patients. The authors therefore investigated the effect of a single bolus dose of 80 000 IU human recombinant erythropoietin (HRE) two days before a planned cardiac surgery. The study was prospectively randomized in 400 patients. The primary endpoint was the need for blood transfusion, and the secondary endpoint was the incidence of adverse events and complications. Hemoglobin levels were determined on the first, second, and fourth days. The HRE group received an average of 0.39 red cell concentrate vs. 1.12 concentrate in control patients (p<0.01). Mean hemoglobin on the fourth postoperative day was 10.2±0.68 g/dL in the HRE group vs. 9.02±0.92 g/dL in the control group (p=0.02). Mortality and complication rates showed no significant difference. The simplified protocol (single dose) appears to be effective and avoided the problems of a more complex application.
Early outcomes after transcatheter “valve-in-valve” implantation in Scandinavia [3].
Transcatheter “valve-in-valve” implantation is increasingly used as an alternative to surgical valve replacement for worn biological prostheses. The authors summarize the experience in Scandinavia between 2008 and 2012.
Forty-nine patients were treated in eleven hospitals; an aortic valve was implanted in 45 patients, a mitral valve and a tricuspid valve in two patients each. The majority of patients were treated by transapical access and the median observation time was eleven months. No mortality was observed and the technical success was 95.6%. The following serious complications occurred:
- cerebrovascular insult (2.2%)
- periprocedural myocardial infarction (4.4%)
- vascular access complication (2.2%).
Hemodynamics showed a mean pressure gradient between 4 and 38 mmHg, (mean 17 mmHg) and a maximum pressure gradient between 7 and 68 mmHg (mean 30 mmHg). This multicenter registry confirmed that the valve-in-valve approach is an acceptable option for high-risk patients and that a substantial number of patients remain with a suboptimal pressure gradient. The long-term consequences of these adverse systolic hemodynamics require further investigation.
Should paroxysmal atrial fibrillation (VHFli) be treated during cardiac surgery? [4]
Several prospective randomized trials have demonstrated the efficacy of intraoperative ablation therapy for permanent AF. The situation is clearly less clear in patients with paroxysmal atrial fibrillation. The hypothesis of this study was that left atrial ablation does not increase perioperative risk and results in a decrease in episodes of AF.
More than 4000 patients were observed, 1044 of whom had preoperative atrial fibrillation. 541 patients suffered from paroxysmal atrial fibrillation (VHFli) and 50% required mitral valve surgery. The following three groups were compared: patients with VHFli who were treated (n=429), patients without treatment (n=112), and finally patients without a history of VHFli (n=3271). Thirty-day mortality was comparable in the three groups. Patients who were treated had a shorter hospital stay, lower incidence and perioperative complications (24% vs. 45%). The rate of cerebrovascular insults was also comparable in all three groups.
Performing left atrial pulmonary vein ablation in patients with atrial fibrillation does not increase perioperative risk and perioperative mortality. Patients who underwent intraoperative ablation showed a higher rate of AF-free interval and better survival compared with untreated patients. This study shows that pulmonary vein ablation may well be a useful intervention in selected patients.
Source: Annual Congress of the “American Association for Thoracic Surgery”, May 4-8, 2013 in Minneapolis/USA
Literature:
- Puskas J, et al: Reduced anticoagulation after mechanical aortic valve replacement: interim results from the PROACT randomized FDA trial. AATS Abstract-Book, p. 87.
- Weltert L, et al: Singlehighdose of erythropoietin twi days before surgery: a simplified short term approach to blood spare. AATS, Abstract-Book, p. 93.
- Ihlberg L, et al: Early clinical outcome of transcatheter valve-in-valve implantation in the Nordic countries. AATS Abstract-Book, p. 97.
- Andrei AC, et al: Should paroxysmal atrial fibrillation be treated during cardiac surgery? AATS Abstract-Book, p. 107.