The number of syphilis cases is steadily increasing. Although syphilis is readily curable, it is a serious, markedly multiform infection that can potentially affect all organ systems. However, early diagnosis is not always easy.
In August of this year, the New York Times headlined “Hunting a Killer: Sex, Drugs and the Return of Syphilis.” This article referred to a rapid outbreak of syphilis in Oklahoma City, the cause of which was attributed to a lack of appropriate medication (namely, benzathine penicillin) and rapid spread within networks, on the one hand, and a medical profession unfamiliar with the problem, on the other. In fact, the United States showed a significant increase in cases of early syphilis in 2016 compared with the previous year (15% increase in males, 36% increase in females, and 28% increase in neonates) [1]. Men who have sex with men (MSM) were most commonly affected. In the United Kingdom, the largest incidence since 1949 was reported in 2017 [2]. This trend is also found specifically in Switzerland, where there has been a steady increase for 15 years; 2017 year seems to have the highest incidence since the reintroduction of mandatory reporting [3]. The current incidence of over 25 per 100,000 population for males and 5.3 for females is among the highest in the Western World. In its June 2016 strategy paper, WHO prioritized syphilis control and set a target of 90% reduction by 2030 [4].
Although syphilis is readily curable, provided it is correctly diagnosed and treated, it is a serious, highly multiform infection that can potentially affect all organ systems. In women of childbearing age, the possibility of transmission to the unborn child must also be considered. This lues connata is increasing worldwide and claims more lives than HIV in Africa, for example [5]. Recent data demonstrate that the diagnosis of early syphilis in MSM is associated with a high risk of consecutive HIV seroconversion [6], which requires special attention and makes these patients potential candidates for HIV pre-exposure prophylaxis (PrEP) [6].
However, recognition of the different early manifestations and their differential diagnoses is a prerequisite for rapid diagnosis of the disease. In syphilis, the key to diagnosis is a detailed examination of the entire integument and its appendages, the ano-genital region, the oral mucosa, and the lymph node stations, taking into account any general, neurologic, ophthalmologic, or otologic symptoms [7]. Patients with high-risk behavior must be appropriately evaluated even without clinical symptoms.
Early syphilis
Early syphilis is defined as primary syphilis, secondary syphilis, and early latent syphilis with a latency period of <1 year (definition by the Centers for Disease Control (CDC), Atlanta) and <2 years (definition by WHO) after infection, respectively.
Primary syphilis
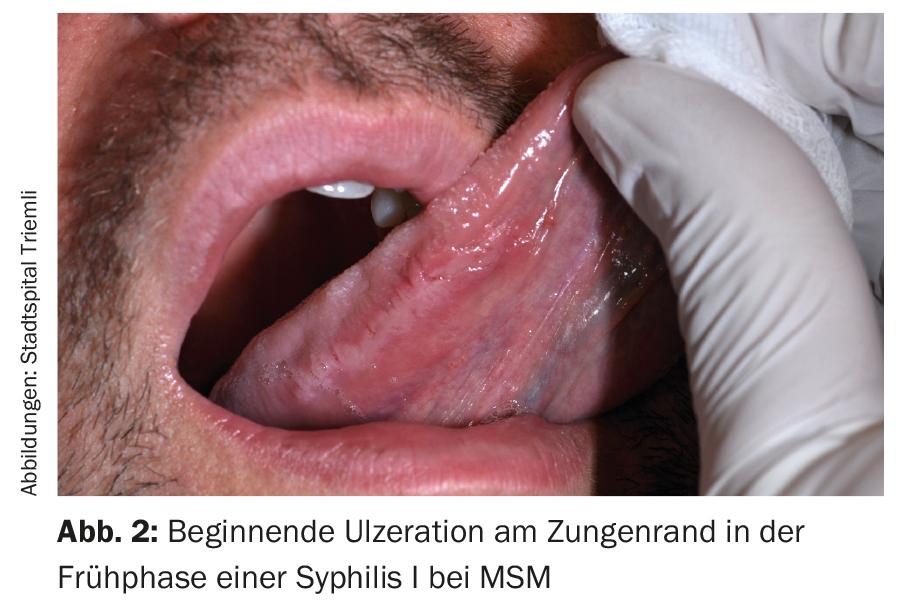
After an average incubation period of three weeks (9-90 days), a dark red spot or papule appears at the site of pathogen entry, which rapidly changes to erosion (Fig.1). The extent and depth of the defect gradually increase until, after one to two weeks, there is typically a painless, sharply demarcated, shallow ulcer with a yellowish base and a dermal, undermined marginal wall [8]. The symptomatology is followed by edematous swelling and bilateral asymptomatic lymph node swelling. Classically, the primary effect is localized in the sulcus coronarius in the male and in the lesser labia in the female. In general, however, it must be noted that stage I often causes diagnostic difficulties due to atypical morphology, atypical symptoms, and atypical localization, which is why only 30 to 40% of patients are diagnosed in the primary stage [9]. This different presentation of the primary effect may be due, on the one hand, to partial immunity caused by prior syphilis, to a concurrent other infection (HIV, herpes simplex virus, hemophilus ducreyi), or, on the other hand, to a change in the pathogenicity of the causative agent.

Atypical clinical presentations
DiCarlo and Martin [10] demonstrated in 446 men with a genital ulcer that the classic, indurated and painless syphilitic ulcer was present in only 31% of patients and in the majority the clinical picture was indistinguishable from a herpetic ulcer or from a molle ulcer [10]. Not infrequently, multiple painful genital ulcers may be present that are clinically much more reminiscent of genital herpes [11]. Case series decades ago demonstrated that multiple ulcers may occur in about half of patients in the setting of primary syphilis. Deep necrosis, actual phagedaenic ulcers can be found in immunosuppressed patients. Rarely, it may progress to perforation of the prepuce or hypertrophic ulcers. Occasionally – especially in cases of reinfection – a primary effect may be completely absent or nodular lesions may be found, at most only an indurated balanitis [12]. However, this atypical form of primary syphilis should not be confused with the rare syphilitic balanitis Follman, where multiple superficial ulcerations with purulent exudate exist and may precede or follow a primary [13].
About one-third of patients complain of sensitivity to touch, which may extend to marked pain. More frequently affected are the extragenital forms and the longer persistent ulcers, where superinfection with Staphylococcus aureus, for example, is more common. Likewise, assessment of the lymph nodes could not significantly improve clinical diagnosis because, as in other infections, lymph node swelling can be painful in syphilis [10].
Atypical localization
In addition to this nondiscriminatory clinical presentation, the ulcer may go unnoticed because of its location. This particularly affects endoanal and rectal ulcers in homosexual men and vaginal, cervical, or ano-rectal ulcers in women. Because pain is observed in only a minority of rectal primary infections, and at most blood or mucus discharges, these infections often pass unnoticed. An aggravating factor in rectal ulcers is that the lymph node swelling is localized paraaortally rather than inguinally and is therefore not noticed. In England, homosexual syphilis patients exhibited anal primary affect (PA) in 20% in one study (Fig. 1) [14]. Occasionally, only nodular or areal indurations (oedema indurativum) or fissures are found, which makes it necessary to differentiate them from hemorrhoidal disease, anal fissures, and other infections such as a herpes simplex infection [15]. Inspection of the anal canal – preferably with a proctoscope – should be a routine part of the workup for a sexually transmitted infection. Extragenital PA is most commonly found orally (Fig. 2) and anally, but in principle can occur at any mucocutaneous site that has been in contact with an infectious lesion. The incidence of extragenital PA is reported in the literature to be approximately 5-31% [16–19]. Approximately two-thirds of extragenital PAs are found in the head and are caused by unprotected oral sex. 12.5% of homosexual syphilis patients exhibited oral PA [16]. It is important to note that due to the increasing popularity of oral sex in recent decades, not least as a supposedly unproblematic practice, there has been an increase in oral PA. While extragenital ulcers were not uncommon decades ago, we must reacquaint ourselves with this clinic and include syphilis in the differential diagnosis for any indurated ulcer associated with regional lymph node swelling. Differential diagnoses include extragenital sporotrichosis, tularemia, mycobacteriosis, feline scratch disease, leishmaniasis, staphylococcal lymphangitis, and granulomatous diseases and neoplasms.
Secondary syphilis
Hematogenous seeding of the pathogen begins the second stage of infection. Skin manifestations are varied [20]:
- Macular (small/large spots)
- Papular (corymbiform, psoriasiform, lichenoid, annular, pigmented, papulo-pustular, condylomata lata).
- Pustular
- Follicular (grouped, pigmented)
- Scarred (after lues maligna)
The spectrum of organ involvement in secondary syphilis fans out as follows [20]:
- Skin and mucous membrane (see above), lymph nodes
- Eye (uveitis, conjunctivitis, scleritis, episcleritis, keratitis, iritis, vitritis, retinitis, vasculitis, optic neuritis, pupillary abnormalities).
- CNS (meningitis, meningoencephalitis, stroke, neuropathy)
- Lung (pneumonitis, pleural effusion)
- Musculoskeletal system (arthralgias, arthritis, periostitis, bursitis)
- Kidney (glomerulonephritis, nephrotic syndrome)
- Gastrointestinal tract (gastritis, ulcer, hepatitis, hepatomegaly, splenomegaly, proctitis).
- Ear (hearing loss, etc.)
Diagnostics
A clinical diagnosis in stage I is in most cases not reliable due to the large clinical variability [21] and seroreactions may still be false negative in the first three weeks, so pathogen identification should always be attempted. This is most commonly done with darkfield examination, which achieves a sensitivity of 79-97% with a specificity of 77-100% for skilled examiners [22,23]. False negative results are usually the result of using topical antibiotics or taking even small amounts of systemic antibiotics. Dark field examination is the only method that allows immediate diagnosis with immediately following therapy. This also enables the fastest possible partner treatment and interruption of further spread [24]. Alternatively, polymerase chain reaction (PCR)-based assays have become established for the detection of treponemal DNA [25]. Specificity is reported to be 95-97%, while sensitivity ranges from 91-95% [26]. In addition to a specific serological screening test (TPPA – Treponema pallidum particle agglutination test or an enzyme immunoassay), it may be worthwhile in the early phase to also determine IgM antibodies [27].
Diagnosis of all other stages and detection of response to therapy are performed serologically [28].
Conclusions
Despite elaborate and sometimes expensive prevention efforts, the trend of increasing syphilis continues unabated. However, containment of the further spread can only be achieved by the fastest possible diagnosis with the initiation of immediate, adequate therapy for the affected persons and their sexual partners. However, this requires awareness of the multifaceted symptomatology, knowledge of the typical and atypical clinical presentations and courses, and laboratory diagnostics. Likewise, patients at risk should be identified and also tested repeatedly. As a result of the reduction in condom use, particularly in the context of PrEP, a decrease in new infections of syphilis and other STIs can hardly be expected in the future.
It would also be desirable to do more research on the interaction of syphilis and HIV, a better “test of cure”, intensified measures to educate the population about the ways of infection, and hopefully, at some point, a vaccination.
Take-Home Messages
- The spread of syphilis continues to increase.
- The multiform manifestations of syphilis – not only in the secondary stage – need to be made better known.
- Any infiltrative ulceration associated with regional lymph node swelling should also be suggestive of syphilis.
- Only rapid recognition of the primary effect and correct diagnosis by pathogen detection allow rapid therapy and partner clarification in the early phase to contain the further risk of transmission.
- In addition to the varied skin symptoms of secondary syphilis, all organ systems may also be affected. Especially the possible eye and ear involvement should also be considered.
Bibliography with the author
DERMATOLOGIE PRAXIS 2017; 27(6): 4-8