Consistent research into multiple sclerosis and translation of findings into clinical practice has led to major advances in both understanding of the disease and therapy management in recent years. Exciting new drugs are in trials, and already established ones are being used more extensively and earlier than before with success.
Multiple sclerosis (MS) has many faces – making it a major challenge for everyone involved. Worldwide, about 2 million people suffer from MS, in Switzerland there are about 10,000. What causes the immune system to turn against its own body is not yet clearly understood. However, it is a fact that sclerosis develops during acute inflammatory activity. These lesions may slowly evolve during increasingly chronic inflammation to form leptomeningeal follicle-like aggregates. Here the danger exists, because outwardly inconspicuous, the progression of the disease often continues in secret. 60% of patients had progressive disability before escalation therapy was initiated, according to one study [1]. This speaks for the early use of highly active therapies, emphasized Prof. Ralf Gold, MD, Bochum (D). The risk of progressive clinical disease activity can thus be reduced by 74% [2].
Thrust-free does not necessarily mean progression-free
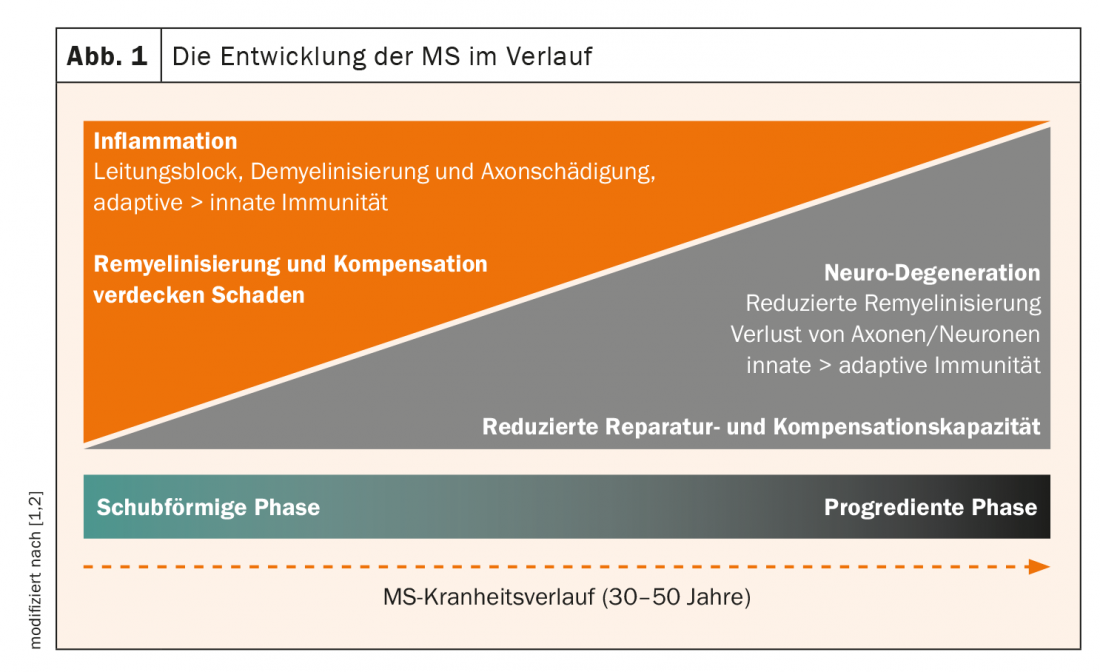
In the meantime, the course of the disease could be detected as a continuum, moving from the relapsing phase to the progressive form (Fig. 1) . The damage initially masked by remyelination and compensation comes to fruition over time through reduced repair and compensatory capacity. Vulnerability to comorbidities also increases over time. It has also been shown that axonal damage is greatest in early stages of disease [3]. The subject of recent investigations has been the role of B cells in disease progression. AK-independent B-cell function has been shown to play an important role in the pathogenesis of MS [4–6]. This is where antibodies attack. Primary progressive multiple sclerosis, previously considered untreatable, can now be treated with a CD20 antibody. The risk of disability progression was reduced by 25% in the pivotal study of ocrelizumab [7]. In addition, Bruton’s tyrosine kinase (BTK) plays an important role in cellular immune processes. This is to be addressed in the future with BTK inhibitors – studies are ongoing.
Fast onset of action for effective results
In relapsing-remitting MS, cladribine, an agent with antineoplastic and immunomodulatory activity, has been available for a good year. Oral therapy is characterized above all by a rapid onset of action, as the expert pointed out. An improvement in the thrust rate was already measurable after four weeks [8]. Overall, the time to first relapse was extended from 4.6 months on placebo to more than 13 months [9]. In addition, a significant effect on disability progression has been demonstrated [10]. These results were confirmed by recent evaluations: Already in the first examination section after one month MRI data showed a significant reduction of combined lesions – with increasing therapy effect over time [11].
Source: DGN 2020
Literature:
- Harding K, et al: JAMA Neurology 2019; DOI: 10.1001/jamaneurol.2018.4905.
- Freedman MS, et al: Mult Scler J Exp Transl Clin 2017; 3: 2055217317732802.
- Pfeifenbring, et al: Ann Neurol 2015; 77: 655-667.
- Bar-Or, et al: Ann Neurol 2010; 67: 452-461.
- Fraussen J, et al: Autoimmune Rev 2016; 15: 896-899.
- Jelcic I, et al: Cell 2018; 175: 85-100.
- Montalban X, et al: N Engl J Med 2017; 376(3): 209-220.
- Vemersch, et al.: ECTRIMS 2009 [P617]
- Comi G, et al: ECTRIMS 2009 [P469]
- Giovannoni G, et al: NEMJ 2010; 362: 416-426.
- De Stefano N, et al: ACTRIMS/ECTRIMS 2020. [P0382]
InFo NEUROLOGY & PSYCHIATRY 2020; 18(6): 22 (published 11/28/20, ahead of print).