A blood eosinophilia is defined by a number >500 eosinophils per μl. If a number >1500/μl is measured at least twice within two weeks, one is dealing with hypereosinophilia (HE). Hypereosinophilic syndrome (HES) is when organ damage is added to HE. How to further classify HES and diagnose EGPA, for example, was discussed at the DGIM Congress 2023.
Since 2012, HE and HES have been subdivided into primary forms and reactive forms based on different etiologies, and idiopathic HE and HES in which neither clonal nor reactive underlying disease is identified. Due to the increasing number of markers and targets, an update of this classification was published earlier this year [1]. Among other things, the update specified that a measured count of >1500/µl on at least two occasions at an interval of at least two weeks is required to define HE – in the previous version, the time interval was still four weeks.
As Prof. Peter Valent, MD, University Hospital AKH Vienna, and colleagues write, in addition to the presence of HE in blood and/or tissues and HE-associated organ damage as a third criterion, HES is defined by the exclusion of other underlying disease or pathology as the primary cause of organ damage.
The authors emphasize that HES is neither a definitive diagnosis nor a defined immunologic or hematologic disease. Rather, the contributing etiology must be identified in all patients with HES, if possible. If no underlying disease is identified, the final diagnosis is idiopathic HES (HESI).
The subtypes of HES are myeloproliferative (14%) and lymphoproliferative (14%) disorders, idiopathic (42%), associated (9%), and superimposed (21%) disorders. The group of associated diseases includes eosinophilic granulomatosis with polyangiitis (EGPA), formerly known as Churg-Strauss syndrome.
Anti-neutrophil cytoplasmic antibodies (ANCA) are detected in approximately 40% of patients with EGPA. Given the similarity of the clinical manifestations of EGPA (and other HE-related syndromes) to the classic features of HES, Valent et al. concluded that these syndromes should be classified as HES if the HES criteria are met. If this is not the case, the final diagnosis should be the appropriate syndrome and not HES.
| ACR classification criteria for vasculitis Eosinophilia >10% (optional). Tissue eosinophilia Asthma (>90%) NNH abnormalities (approx. 50%) Volatile pulmonary infiltrates (50-70%). Neuropathy (approx. 75%) |
| according to [3] |
Detection of vasculitis often not possible
“To distinguish between an HES and an EGPA, you have to know that EGPA needs evidence of vasculitis,” explained Dr. Christof Iking-Konert, head of the department of rheumatology at the Stadtspital Triemli in Zurich [2]. He referred in this regard to To the American College of Rheumatology (ACR) classification criteria [3] (box).
EGPA is the rarest form of ANCA-associated vasculitis, with a prevalence of 24/1 million, so the first diagnostic challenge is to think of it first. The second hurdle: The required detection of vasculitis in histology is often difficult because, for example, a biopsy is not feasible in very sick patients. EGPA is mostly suspected, so vasculitis surrogates are used as a guide, Dr. Iking-Konert explained. According to him, if one or more of these factors are present, one can assume a vasculitis correlate:
- Alveolar hemorrhage
- Palpable purpura
- Myocardial infarction due to proven coronariitis
- Hematuria associated with red blood cell count or >10% dysmorphic red blood cells or hematuria and 2+ proteinuria.
- Mononeuritis or mononeuritis multiplex
- MPO ANCA and any type of systemic manifestation.
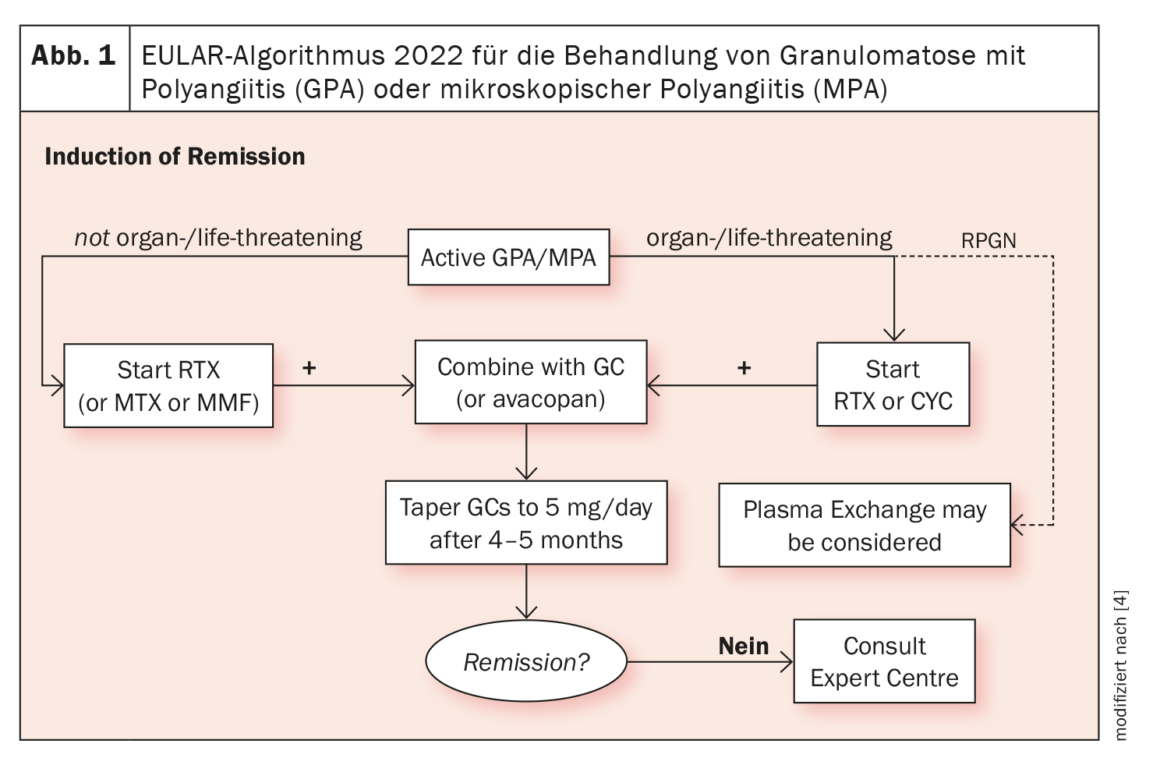
Biologics have been available for the treatment of EGPA for more than a decade. In addition to rituximab, targeted therapies with IL-5 antibodies have become established. Dr. Iking-Konert referred to the EULAR guideline on the management of ANCA-associated vasculitides, which will be updated in 2022: This recommends starting therapy with cyclophosphamide (CYC) or rituximab (RTX) combined with cortisone in the case of organ- or life-threatening EGPA. In non-organ or -life threatening disease, IL-5 blockade is indicated for refractory or severe courses (Fig. 1) [4].
Congress: DGIM Industriesymposium GSK
Literature:
- Valent P, et al.: Allergy 2023; 78: 47–59.
- Industrie Symposium «Und täglich grüsst das Immunsystem: seltene Autoimmunerkrankungen erkennen und behandeln». 129. Kongress der DGIM, 23.04.2023; Veranstalter: GSK.
- Jennette JC, et al.: Arthritis Rheum 1994; 37: 187–192.
- Hellmich B, et al.: Ann Rheum Dis 2023; doi: 10.1136/ard-2022-223764.
| Cover: High magnification micrograph of eosinophilic vasculitis consistent with Churg-Strauss syndrome, abbreviated CSS. H&E stain. Source: Nephron, wikimedia |
InFo RHEUMATOLOGIE 2023; 5(1): 17