A medical expert panel has developed consensus-based criteria as a decision support tool for triage of patients with suspected or confirmed SARS-CoV-2 infection who have only mild symptoms. This is intended to aid decision-making by the responsible health care personnel and to counteract the threat of overcrowding in inpatient clinical facilities. However, the “HOME-CoV” rule is only appropriate for patients without risk factors for severe COVID-19 progression.
There is a growing concern that the health care system, and especially intensive care units and emergency medicine departments, may be overwhelmed by the magnitude of the COVID-19 pandemic. Unnecessary hospitalization of patients with mild symptoms could contribute to hospital congestion, according to experts. Therefore, triage of outpatient care vs. inpatient care for COVID-19 sufferers is an important consideration. The following summary is based on the article “Outpatient management or hospitalization of patients with proven or suspected SARS-CoV-2 infection: the HOME-CoV rule” published in Internal and Emergency Medicine in September 2020. The first author, Delphine Douillet, MD, is a senior physician in adult emergency medicine at Angers University Hospital (F)*. The described research project has an approval from the “Comité de Protection des Personnes Ouest IV-Nantes” and was funded by the University Hospital Angers.
* Douillet, et al: Intern Emerg Med 2020. https://doi.org/10.1007/s11739-020-02483-0
www.chu-angers.fr
Criteria-driven decision making tool
The goal of the present project was to develop a workable, criteria-guided rule for triage of patients with suspected or confirmed COVID-19 disease. Reliable criteria for deciding outpatient care vs. hospitalization are a key factor in preventing overuse of inpatient clinical facilities. To help healthcare workers do this, a group of clinicians and researchers in France developed the “HOME-CoV” rule. For this purpose, an expert panel of 51 professionals (emergency physicians, geriatricians, infectiologists, medical ethics consultants) conducted a multilevel criteria assessment using the Delphi method**.
** The Delphi method is a systematic multi-stage procedure for obtaining expert consensus.
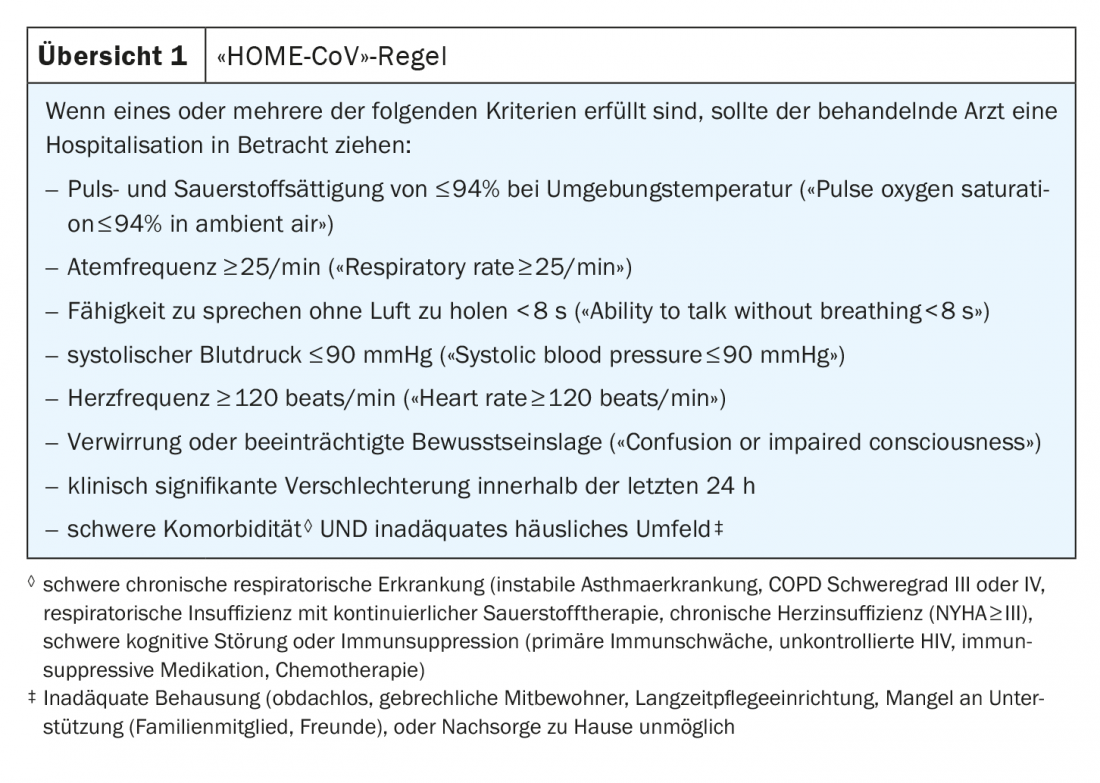
Four rounds of anonymous expert consultation were conducted in April 2020 to evaluate a literature-based list of potential criteria. Each item was rated by the experts according to the following classification with respect to the “HOME-CoV” rule: ‘relevant’, ‘possibly relevant’, ‘not relevant’. Eight criteria were selected, six of which related to the severity of clinical symptoms, one to clinical course (clinically significant worsening within the last 24 hours), and one to a possible association with severe comorbidity and an inadequate home environment. The criteria of the “HOME-CoV” rule are summarized in overview 1 . Hospitalization is considered necessary when a patient meets one or more criteria. This procedure resulted in 94.4% agreement of the experts with the rule thus defined. The authors caution that this rule must be carefully weighed and cannot be applied in all cases (box) .
|
“HOME-CoV” rule not suitable for all patients For patients with certain comorbidities or in certain clinical situations, the “HOME-CoV” rule cannot be used, the study authors said. Caution is advised in particular with regard to patients with obesity, diabetes and hypertension, as there is still a small evidence base in this regard. However, the “HOME-CoV” rule could be considered as a guide to develop criteria for triage tailored to a particular context. |
Counteracting congestion in inpatient facilities
Without reliable criteria for triage of COVID-19 patients, the likelihood of hospitalization of cases that could have been managed in the outpatient setting tends to be increased. Being guided by whether there is any concern that a rapid deterioration could develop or that timely hospitalization could not be assured is too woolly and could lead to an underestimation of the possibility of caring for patients in the outpatient setting, contributing to overuse of inpatient healthcare facilities, the authors argue. They support this thesis on the one hand with an analysis showing that of 1099 hospitalized COVID-19 patients in China, 6.1% required mechanical ventilation and 41.3% oxygen therapy, indicating that a large proportion of hospitalized patients could also have been cared for on an outpatient basis***. Secondly, it refers to the analysis of a large Chinese cohort of 72′ 314 COVID-19 patients, of whom 81% were classified as mild (no pneumonia or mild pneumonia) and a relatively small proportion of 14% as severe.****
*** Guan W-J, et al: N Engl J Med 2020, https://doi.org/10.1056/NEJMoa2002032
**** Wu Z, McGoogan JM: JAMA 2020, https://doi.org/10.1001/jama.2020.2648
For patients with pneumonia or sepsis, he said, there are many scores to identify low-risk patients such as PSI, CRB 65, CURB65, SOFA, and qSOFA. However, these are not fast-track procedures, as biological parameters or imaging studies are required.
The Delphi method is a proven procedure to define a set of criteria based on expert consensus and is particularly recommended in situations where there is an insufficient evidence base of scientific data. For example, this is how the SEPSIS-3 consensus was developed for outpatient management of parenteral antimicrobial therapy and for a regimen for de-escalation of beta-lactam antibiotics. The Delphi process was conducted via the Internet, which was possible within less than two weeks.
Source: Douillet D, et al: Outpatient management or hospitalization of patients with proven or suspected SARS-CoV-2 infection: the HOME-CoV rule. Intern Emerg Med (2020). https://doi.org/10.1007/s11739-020-02483-0
FAMILY PRACTICE 2020; 15(11): 44-45











