Low-grade dysplasia is associated with an increased risk of progression in Barrett’s esophagus, but the diagnosis of LGD is limited by considerable interobserver variability. Several studies have shown that the tissue system pathology test TSP-9 is effective in predicting neoplastic progression in patients with BE. A team of researchers from Amsterdam compared the performance of the TSP-9 test in risk stratification with benchmarks from general practitioners and pathology experts.
Barrett’s esophagus (BE) is a premalignant condition characterized by the transformation of the squamous epithelium of the esophagus into metaplastic columnar epithelium. Risk stratification in Barrett’s surveillance is largely based on histologic review of random biopsies by pathologists. Low-grade dysplasia (LGD) is the strongest predictor of progression to high-grade dysplasia (HGD) and if left untreated it can develop into esophageal adenocarcinoma (EAC) with a 5-year survival rate of less than 20%. However, it is not easy to distinguish reactive inflammatory changes (“atypia”) from early neoplastic changes (“dysplasia”), explained Dr. Nicola Frei, Department of Gastroenterology and Hepatology, Amsterdam University Medical Centers (UMC), University of Amsterdam site [1].
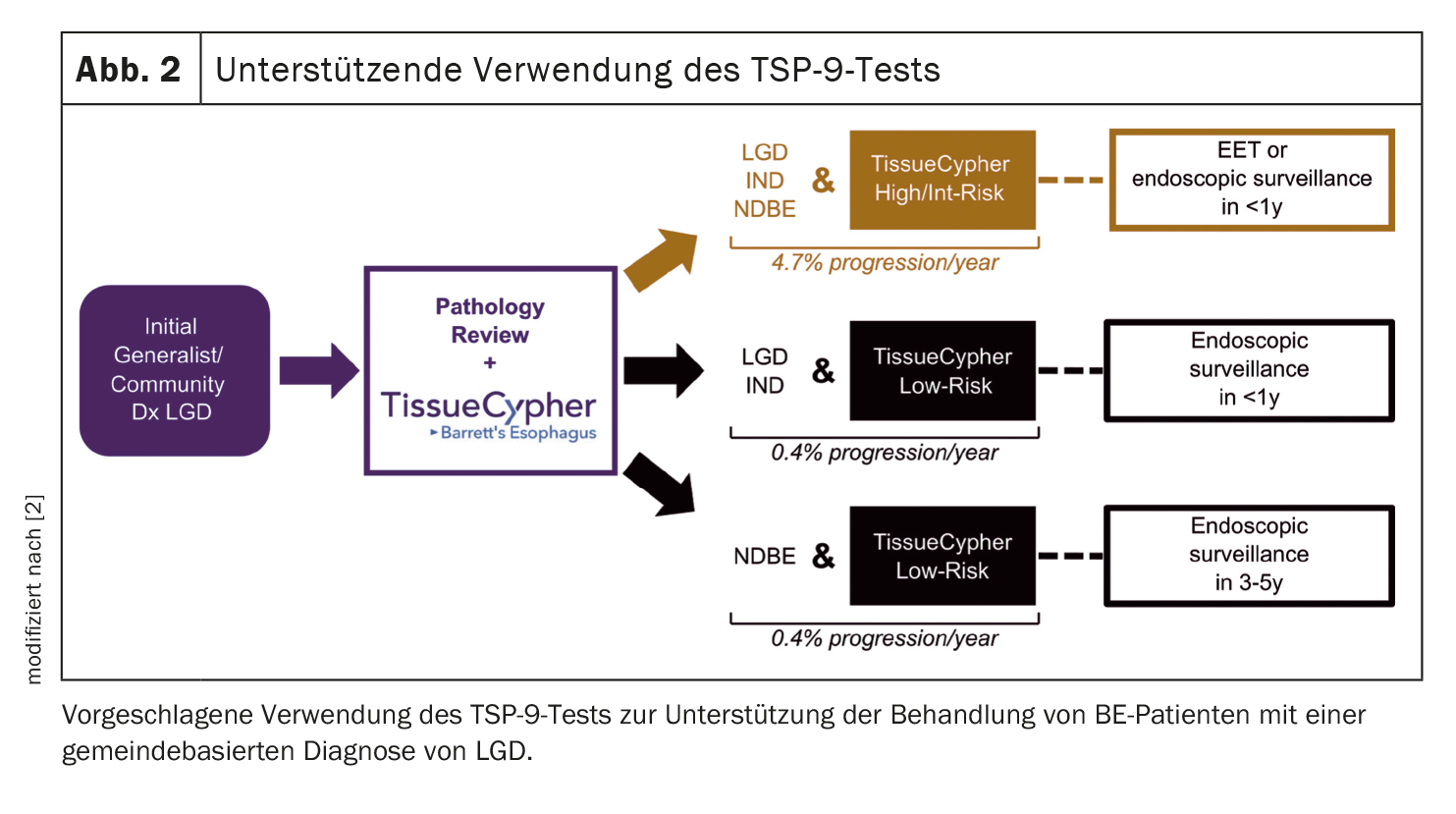
Current practice guidelines recommend that the diagnosis of LGD be verified by a pathologist specializing in GI. If LGD is confirmed, the recommended treatment strategy is endoscopic eradication therapy (EET) to prevent disease progression or endoscopic surveillance every 6 to 12 months to closely monitor the disease, as these patients are at increased risk of neoplastic progression.
Studies have shown that LGD is often overdiagnosed in general practices: “73-85% of LGD cases are downgraded to a diagnosis of ‘non-dysplastic’ (ND) or ‘indeterminate dysplasia’ (IND) after review by an experienced GI pathologist,” says Dr. Frei. “These down staged patients do not have an increased risk of neoplastic disease. However, patients with confirmed LGD have an annual risk of 10-13% for progression to HGD/EAC.”
TSP-9 test achieves higher sensitivity
The TSP-9 test (TissueCypher Barrett’s esophagus test) is an objective tissue system pathology test specifically designed to predict the risk of progression from BE to HGD and EAC. A quantitative image analysis is linked to a risk prediction algorithm that integrates 15 quantitative image analysis features to create a risk score from 0 to 10. This then divides the patients into a high, medium and low risk of progression to HGD/EAC within five years. In their current study [2], Frei et al. the results of the test vs. the opinions of general practitioners and experts.
A blinded cohort study was conducted in the screening cohort of a randomized controlled trial of BE patients with community-based LGD. Biopsies from the first endoscopy with LGD were assessed with the TSP-9 test and independently reviewed by 30 pathologists. A total of 154 BE patients (122 of them men) with an average age of 60.9 ± 9.8 years were examined.
“The pathologists are made up of 15 pathologists from all over the world (Netherlands, USA, UK, Germany and Belgium). Each of them has an international track record in the field of Barrett’s esophagus for more than ten years, with a minimum of five to ten mainly dysplastic cases per week,” explained Dr. Frei. “On the other hand, we have 15 private practice or community-based pathologists (evenly distributed across the same countries) who refer dysplastic BE cases to a specialized pathologist.”
The TSP-9 test classified 45 (29.2%) patients as high risk and 109 (70.8%) as low risk for progression to HGD/EAC within five years. The pathologists confirmed LGD/higher in an average of 19% of cases (range 8-41%) and downgraded an average of 13% (range 0-75%) to IND and an average of 68% (range 12-88%) to NDBE. Annual progression rates were 9.2% per year for patients with confirmed LGD/higher, 3% per year for patients downgraded to IND, and 1.7% per year for patients downgraded to NDBE.
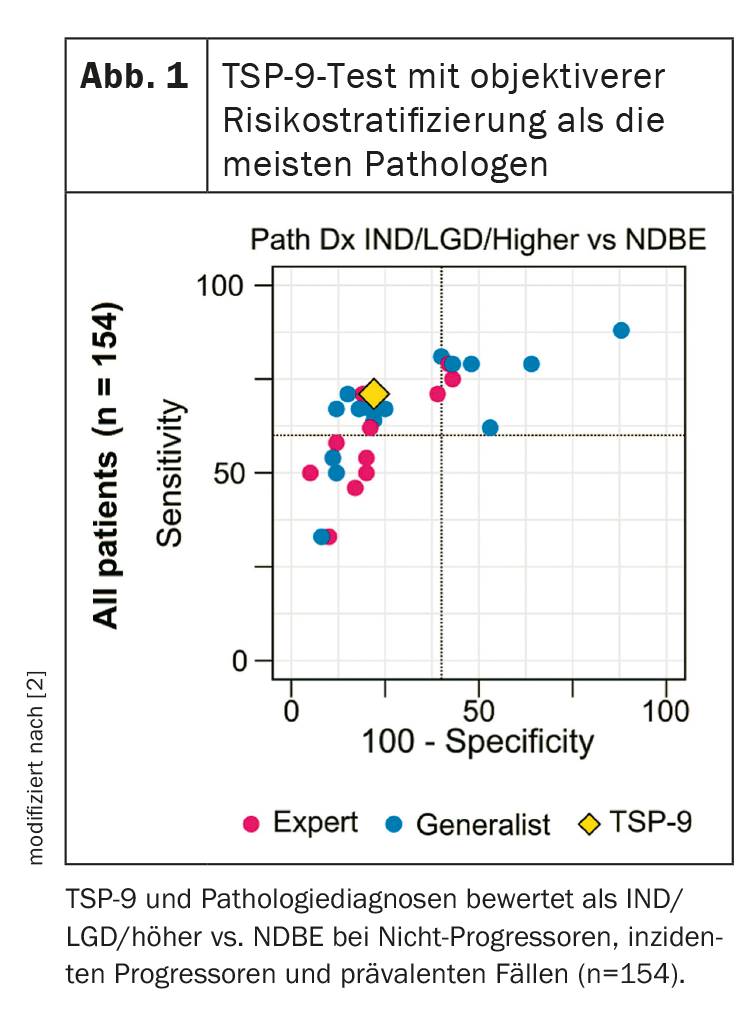
24 patients developed HGD/EAC within five years (median 1.7 years) and 130 did not develop HGD/EAC within 5 years (median 7.8 years). The TSP-9 test showed a higher sensitivity in detecting patients who developed progression within five years (70.8% vs. 63.2% on average; p=0.01186). A wide range of sensitivity (33-88%) was also observed among the 30 pathologists.
Pathologists’ judgments with great variability
The accuracy of expert and general practitioner diagnoses showed significant interobserver variability. The predictive accuracy of the general practitioners’ diagnoses varied widely, and although the experts’ diagnoses showed slightly less variability, the overall predictive accuracy was not significantly higher than that of the general practitioners (Fig. 1).
The TSP-9 test led to an objective risk stratification of LGD patients with an overall higher sensitivity in detecting progressors than benchmarks from general practitioners and experienced pathologists, Dr. Frei summarized the results.
Current guidelines recommend that the diagnosis of BE with LGD should be confirmed by an expert pathologist to better risk stratify patients and make appropriate management decisions. However, the term “expert pathologist” is not precisely defined, the speaker said, and confirmation of LGD is a challenge, which limits compliance with the expert examination in practice. Based on the results of their study, the authors propose a guideline on how the TSP-9 test can be used to improve the management of patients with BE diagnosed with LGD (Fig. 2) .
The TSP-9 test enables objective risk stratification in patients with BE with community-based LGD and, on average, outperforms even experienced pathologists in identifying patients who progress to HGD/EAC. The test is also not subject to the fluctuations of the observers and can therefore offer an objective solution for the subjective and variable pathology classification, Dr. Frei concluded. TSP-9 is therefore a more logical tool for risk stratification of LGD as it is fully automated, objective and highly reproducible, outperforming most pathologists.
Congress: SGG Annual Congress 2023
Sources:
- Frei NF: Lecture “A Tissue Systems Pathology Test Outperforms Pathology Review in Risk Stratifying Patients with Low-Grade Dysplasia”; Annual Congress of the Swiss Society of Gastroenterology (SGG), Interlaken, 14.09.2023.
- Khoshiwal AM, Frei NF, Pouw RE, et al: Gastroenterology 2023; 165: 1168-1179; doi: 10.1053/j.gastro.2023.07.029.
GASTROENTEROLOGIE PRAXIS 2023; 2(1): 19-20 (published on 27.11.23, ahead of print)
Cover picture: Barrett’s esophagus (left part of image). ©Nephron, wikimedia