Addressing aspects of patient-centeredness helps improve compliance. Comprehensive and comprehensible patient education and information form the basis for making informed decisions in the sense of “shared decision making” – an important pillar of patient orientation as it is defined today.
The Medical Center for Quality in Medicine (ÄZQ) is committed to quality and knowledge transfer in healthcare. In the compendium “Quality Management and the Patient’s Perspective”, patient orientation is defined as follows: that within the framework of a therapy-compliant care process, all parties involved strive to learn about and meet the expectations and needs of patients [1–3]. However, patient orientation also means uncovering and eliminating deficits through continuous quality management. Important criteria for patient orientation of a medical practice are summarized in the box [4].
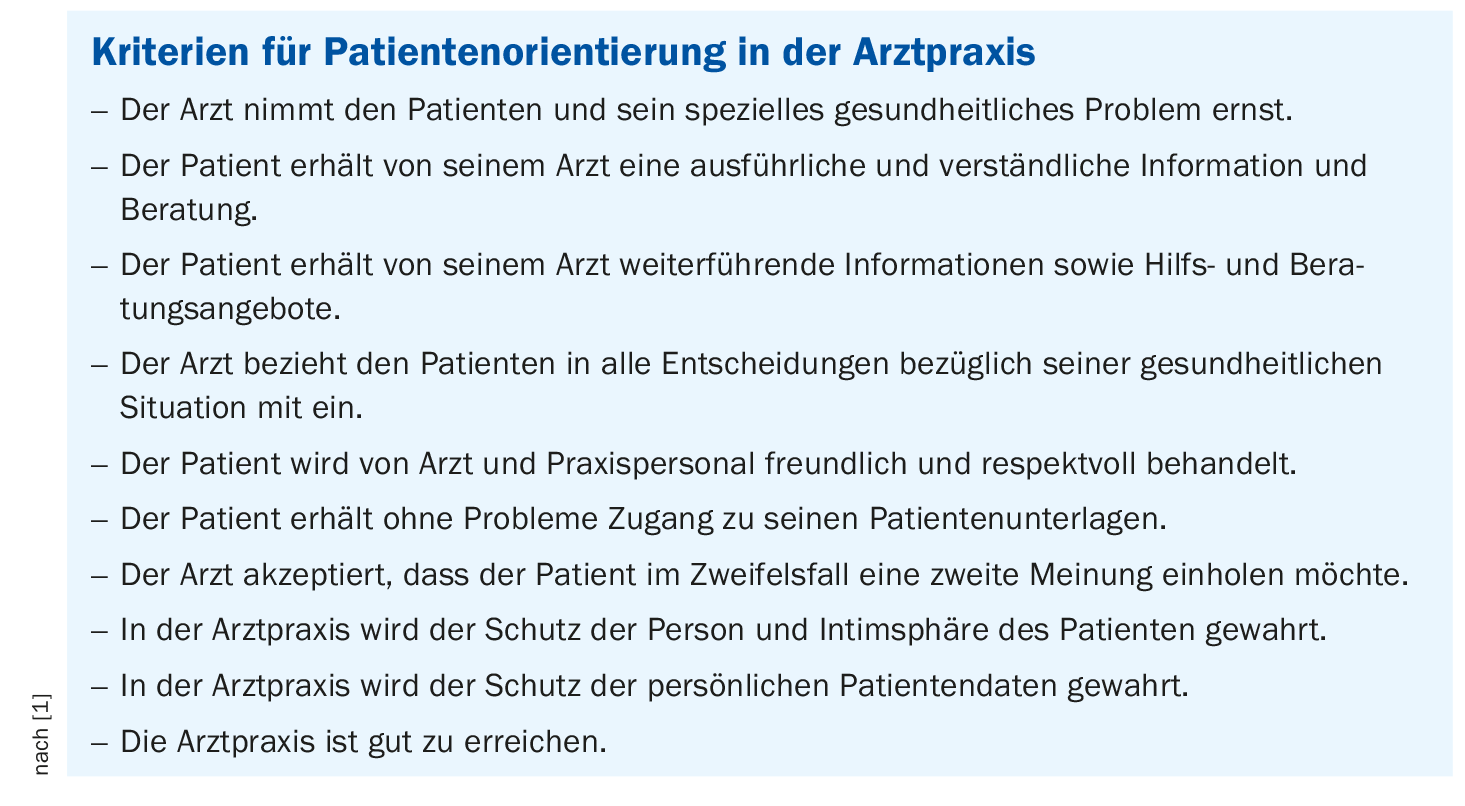
Quality-conscious patients evaluate not only the medical, therapeutic, nursing care received and the outcome of treatment, but also the provision of information, communication with the service providers, the impression of the staff (friendliness, reliability, competence, punctuality, waiting time), interaction with all employees of the practice or clinic, access to and organization in the practice, as well as support offers [5,6].
Participatory decision-making requires education
There are an increasing number of patients who want to be informed about diagnostic and therapeutic measures and self-help options, understand the respective implications, and ultimately have a say in the decision-making process. This corresponds to the core message of the concept of shared decision making: Physician and patient make a jointly responsible decision on the basis of shared information, they enter into a “therapeutic alliance” [7].
Patients often understand only 50% of the information they receive from their physician [8]. Even with a thorough verbal educational discussion, there is no guarantee that patients have understood and can recall the content conveyed. Many patients cannot correctly recall the content of the conversation after leaving the doctor’s office. For this reason, patients should be able to take with them – in condensed form – “in black and white” everything they learn about the disease and possible treatment options, as well as further care and support, during the information session [4]. The convincing thing is: the patient carries something home with him that was created especially for him. Quality should take precedence over quantity. Information tailored to the individual patient has a more professional and personal effect than a copied diet plan or a standard information brochure. Individual consultation prescriptions, patient passports or patient books that integrate individual information – also from different physicians – have proven successful [9].
Literature:
- Medical Center for Quality in Medicine (ÄZQ): Quality Management and the Patients’ View, www.aezq.de/aezq/kompendium_q-m-a/3-qualitaetsmanagement-und-die-sicht-derpatienten/#3, (last accessed Dec. 06, 2022).
- Bleses H: Patient orientation as a quality characteristic. 2005, Dissertation for the degree of Doctor rerum curae (Dr. rer. cur.). Med. Fak. of the Charité, Berlin.
- Dierks ML, Schwartz FW: Patients, insured, citizens – the users of health care. In: Schwartz FW, Badura B, Busse R, Leidl R, Raspe H, Siegrist J, Walter U, The Public Health Book, 2008: 314-321. Urban and Fischer, Munich.
- Medical Center for Quality in Medicine (ÄZQ): How can you recognize a good medical practice? Checklist for patients. ÄZQ 2007, Berlin.
- Bitzer EM, Dierks ML: How to address patient expectations and satisfaction in quality management? – Survey methods and experiences from ambulatory care. In: The Federal Ministry of Health, Quality Management in Medical Practice 1999, 125-184. Nomos, Baden-Baden.
- Wölker T: Qualitätsmanagement in der Arztpraxis – So managen Sie Qualität. Ärzte-Zeitung-Verl.-Ges., 2002: Neu-Isenburg.
- Harder M: Participatory decision making (Shared Decision Making) – an approach demanded by patients, physicians and health policy is gaining acceptance. Z Arztl Fortbild Qualitatssich 2004; 98: 89-92.
- Schillinger D, et al: Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003; 163: 83-90.
- Szecsenyi J, Klingenberg A, Pelz J, Magdeburg K: Evaluation of a patient book by patients – results from the Ried Medical Quality Community. Z Arztl Fortbild Qualitatssich 2001; 95: 407-412.
HAUSARZT PRAXIS 2022; 17(12): 44











