It is well known that low LDL cholesterol reduces the risk of cardiovascular disease. But in practice, this is often easier said than done. Are PCSK9 inhibitors the solution?
Lowering LDL-C levels is an integral part of risk reduction in patients with myocardial infarction. However, very few achieve the target values of 2.5 mmol/l or 1.8 mmol/l in high-risk patients, which are preferred by the European guideline [1]. In this context, statins have clearly demonstrated their efficacy in the treatment of dyslipidemia. However, the incidence of myalgias, which affect up to 10-25% of patients taking statins, has been underestimated [2]. Therefore, the administration of PCSK-9 inhibitors was investigated as an additional option – with success.
The proprotein convertase subtilisin/kexin type 9 (PCSK9) binds to LDL receptors and marks them for degradation in lysosomes. Thus, the density of receptors on the cell surface is reduced and circulating LDL cholesterol in the blood increases. In contrast, if PCSK9 is inhibited, the LDL receptors on the surface of hepatocytes can be recycled multiple times, allowing them to bind more circulating LDLC and lowering levels. This benefits the overall lipid profile.
High-risk patients benefit
Subanalysis [3] of a large-scale randomized, double-blind, placebo-controlled trial [4] showed that additional administration of the PCSK-9 inhibitor evolocumab consistently reduced LDL-C levels by 59-61% in all three groups. The time of the last infarction, the number of infarctions, or the presence of coronary multivessel disease were irrelevant. From this, the experts concluded that therapy with PCSK-9 inhibitors is indicated primarily in patients in secondary prevention who have additional high-risk characteristics.
The deeper the better
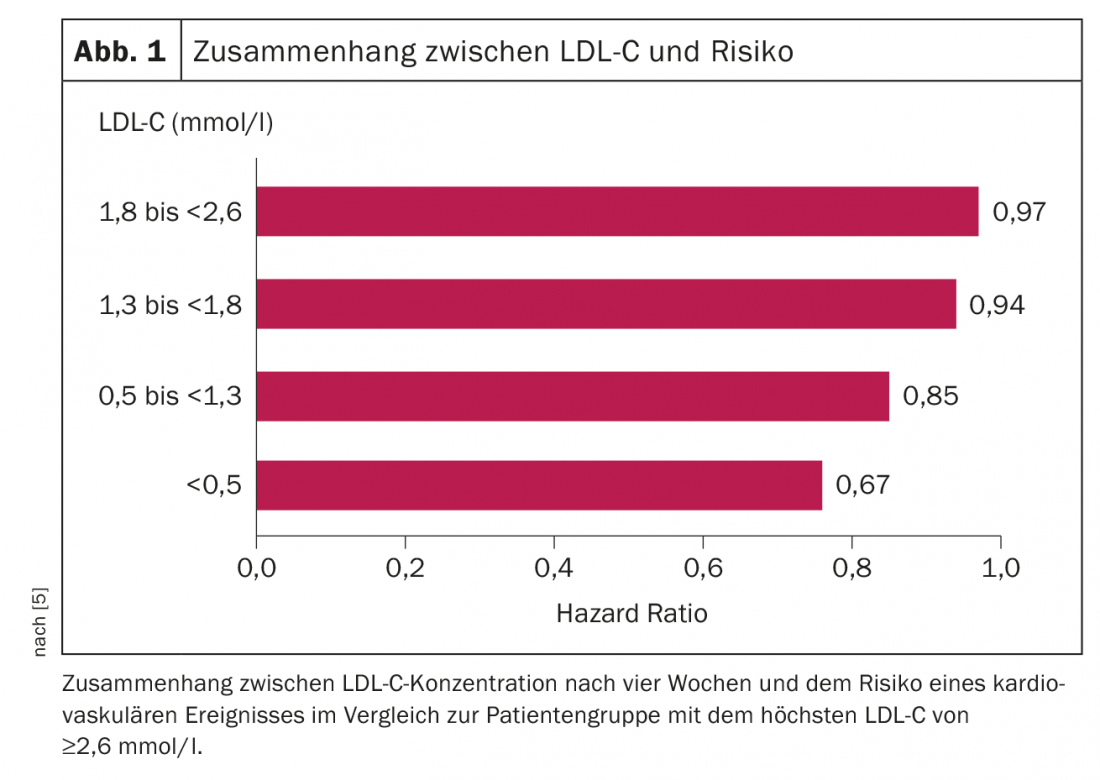
The good response of the patients to the additional lipid-lowering therapy raised a question that had not been asked before: where is the lower LDL-C limit? This is because 10% of the subjects had LDL-C levels of <0.5 mmol/l after four weeks of treatment (median 0.36 mmol/l). Is there any additional clinical benefit to be expected at these levels? Indeed, it was shown that with reduction of LDL cholesterol, the risk of cardiovascular events, such as cardiovascular death, myocardial infarction, stroke, coronary revascularization or hospitalization due to unstable angina pectoris, also decreased (Fig. 1) . The results suggest that even patients already below target levels benefit from further LDL-C reduction. An increase in adverse effects was not observed. Even values <0.5 mmol/l are to be considered safe in the view of the authors on the basis of the results [5], as Prof. Urs Fischer of the University Hospital Bern explained in a lecture.
Source: Swiss Brain Stroke Society Annual Meeting, January 15-16, 2019, Zurich.
Literature:
- www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Dyslipidaemias-Management-of (last access: 01/22/2019)
- Thompson PD, et al: Statin-associated side effects. J Am Coll Cardiol. 2016; 67: 2395-2410.
- Sabatine MS, et al: Clinical Benefit of Evolocumab by Severity and Extend of Coronary Artery Disease: An Analysis from FOURIER. Circulation 2018; 138: 756-766.
- Sabatine MS et al: Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med 2017; 376:1713-1722.
- Giugliano RP et al: Cognitive Function in a Randomized Trial of Evolocumab. N Engl J Med 2017; 377: 633-643.
CARDIOVASC 2019; 18(1): 36











