Opioids form a pharmacologically heterogeneous group of synthetic, semisynthetic, and natural agents whose common feature is binding to opioid receptors. With regard to the development of analgesic effects, the opioid receptors in the central nervous system are crucial. By activating presynaptic opioid receptors in the posterior horn of the spinal cord, the transmission of pain impulses is inhibited.
The term opioid is taken from the Greek and means “similar to opium”. Opioids form a pharmacologically heterogeneous group of synthetic, semisynthetic, and natural agents whose common feature is binding to opioid receptors. Opioid receptors are found in both the peripheral and central nervous systems. With regard to the development of analgesic effects, the opioid receptors in the central nervous system are crucial. By activating presynaptic opioid receptors in the posterior horn of the spinal cord, the transmission of pain impulses is inhibited. Opioid-induced activation of opioid receptors in certain regions of the brainstem causes additional stimulation of descending inhibitory neural pathways. This inhibits the transmission of pain signals arriving in the posterior horn. In subcortical regions of the limbic system, activation of opioid receptors leads to attenuation of the emotional-affective component of the perception of a pain sensation [1].
The human body itself produces endogenous opioids, which are released as part of stress reactions and lead to the suppression of pain and feelings of hunger. In medical practice, synthetic opioids are generally used. Pharmacodynamic differences between the various opioids can be seen in their different affinities for opioid receptors or for individual receptor subtypes. In clinical practice, precise knowledge of these pharmacodynamic differences helps to estimate the expected effect of a particular opioid.
Epidemiology
The 2017 Swiss Health Survey showed that around 2.5 million people in Switzerland suffer from chronic pain. Approximately 0.6 million of those affected suffer from moderate to severe pain conditions that have limiting effects on activity and quality of life. Women are more likely to report suffering from chronic pain [2].
Although there are various therapeutic approaches to the treatment of pain, opioids are increasingly prescribed in Switzerland as well. The use of opioids is well recognized and usually very useful for the treatment of severe acute pain, e.g., in the perioperative setting. Opioids are also often an indispensable and globally recognized therapeutic option for the treatment of tumor-related pain [3]. Chronic noncancer pain, in contrast, is usually a less good indication for longer-term treatment with opioids. It is unclear whether the use of highly potent opioids results in medium- to long-term improvement in the control of chronic noncancer pain [4].
For this very reason, it is concerning that 85% of all opioids prescribed today are used to treat noncancer pain [5]. Approximately 25% of affected patients receive prescribed opioids for a duration of >90 days. Long-term use over years is often the result.
Taxonomy of pain mechanisms
Adequate and effective pharmacologic pain management can be most reliably achieved when the mechanisms of pain causation are delineated as well as possible. A detailed history and focused clinical examination are fundamental to identifying a pain etiology mechanism. Situationally, in case of specific questions, radiological, laboratory and other additional examinations are helpful. The following pain mechanisms must be identified or ruled out:
Nociceptive pain: this mechanism is responsible for maintaining bodily integrity and is also understood as “normal, usual” pain sensation. Nociceptive pain signals help prevent injury. The pain is stimulus-dependent, usually of short duration, and the stimulated tissue remains intact. With continued nociceptive stimulus, neuronal changes may occur in the posterior horn region of the spinal cord. These changes are usually short-lived and regress. Persistent pain sensitization phenomena are not expected.
Nociceptive-inflammatory pain: acute to subacute pain occurs when tissue damage has already occurred. Triggers are released inflammatory mediators (e.g. interleukins). On the one hand, peripheral pain fiber endings are directly activated, and on the other hand, new, previously inactive pain fibers are recruited and additionally sensitized in the course of this process. Overall, there is a decrease in the electrophysiological excitability threshold. This allows the formation of peripheral sensitization phenomena.
Neuropathic pain: Neuropathic pain also occurs acutely or subacutely. However, the cause of the pain signal here is not the surrounding tissue, but the somatosensory system itself [6]. Damage to nerve cells themselves forms the basis of neuropathic pain. Practically always, peripheral and central sensitization phenomena occur. As a rule, “positive” and/or “negative” sensitization phenomena can be documented. There is often a large discrepancy between the intensity of pain complained of by the patient, the extent of the area affected by pain, and the objective findings that can be determined by the examiner.
An important sensitization phenomenon is hyperalgesia. It occurs in both neuropathic and inflammatory pain conditions. Hyperalgesia can be defined as a condition during which a normally mildly painful stimulus is perceived as excessively painful (e.g., pricking with a toothpick). Allodynia is another “positive” sensitization phenomenon and represents an intensification form of hyperalgesia. In a skin area affected by allodynia, a stimulus that is actually painless is perceived as painful (e.g., touch with -brush).
Nociplastic pain: nociceptive/inflammatory pain and neuropathic pain are ultimately mechanistically defined entities. The crucial difference is that in the context of nociceptive pain conditions there is normal function of the somatosensory system, whereas in neuropathic pain conditions this very system is damaged. Many patients with chronic pain cannot be assigned to any of these entities without doubt [7]. In these patients, neither activation of nociceptors nor a lesion of the somatosensory system can be assumed. In such cases, a nociplastic pain problem is present. A large group of patients is affected: Non-specific back pain, non-specific pain in peripheral joints, fibromyalgia, Complex Regional Pain Syndrome (CRPS) type 1.
Overlapping of pain mechanisms/”Mixed Pain”: Very often, an overlapping of the above-mentioned pain mechanisms can be detected/assumed in patients with chronic pain. In “mixed pain”, all of the mechanisms described above are often involved in the development or modulation of the pain signal. Usually, one or the other pain mechanism is in the foreground.
Opioids play an important role in the treatment of nociceptive pain, but can also contribute to good pain control in neuropathic pain. In the case of nociplastic pain conditions, the therapeutic value of opioids is usually nonexistent.
The 4 pillars of analgesia
To achieve the most satisfactory analgesic treatment, recognition of the pain and sensitization mechanisms presented above is central. Regardless of the therapeutic modality, a targeted therapy of pain conditions, or the achievement of “analgesia” is therefore based on the following four pillars: “antinociception”, “anti-inflammation”, “antihyperalgesia” and “antineuropathy” [8].
In the context of pharmacological analgesic therapy, it is therefore crucial to use drugs of one or more substance classes that can cover as far as possible the entire spectrum of diagnosed pain mechanisms.
Recommended measures before starting pain therapy with an opioid
Whether or not a treatment attempt with an opioid analgesic is appropriate requires careful joint consideration between the physician and the patient. Whether weak- or strong-acting opioids should be used is a secondary consideration. The following points should be specifically considered [9]:
- The mechanisms underlying the pain problem must be specifically sought and identified.
- It is recommended that a more detailed psychosocial history and screening for the presence of psychological influences on the pain problem be performed.
- Chronic non-cancer pain should never be treated exclusively with opioids, if possible. Scientific data indicate that opioids are no more effective than other analgesics for the treatment of chronic non-cancer pain.
- Therefore, before pain therapy with opioids is considered, various other therapeutic measures should already have been taken or at least tried (physical, physiotherapeutic, medicinal, interventional, psychological).
- Meaningful and achievable therapy goals should be developed together with the patient. The focus should be on goals such as reducing pain by at least 30%, returning to work, or completing everyday tasks, such as household chores.
- Patients should be advised in detail of the potential hazards that may occur during long-term opioid therapy. In addition to the known side effects such as constipation, dry mouth, nausea, malaise, states of confusion, falls, attention should also be drawn to potentially life-threatening respiratory depression as a result of incorrect/overdosage.
- Patients must be informed that physical dependence usually results from therapy with an opioid.
- During the first 1-2 weeks of therapy, during the adjustment phase, when the dose is increased or when switching to another opioid, driving or operating machinery must be avoided. During this time, side effects that limit responsiveness are common.
When can long-term therapy >120 days with opioids be considered?
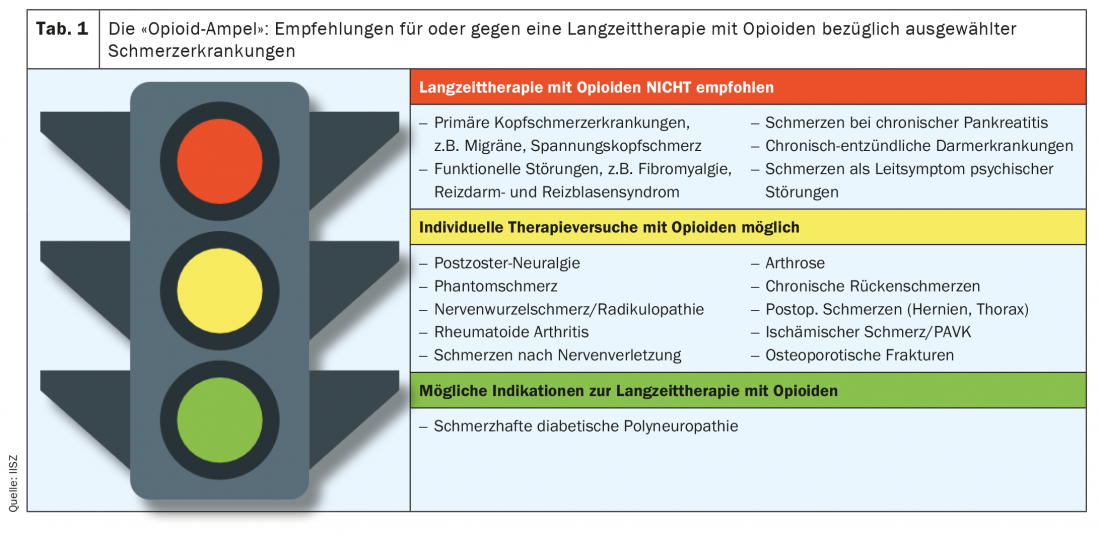
The principle applies that opioids should only be used for long-term therapy (>120 days) of a chronic pain condition if the patient concerned has experienced a significant reduction in pain and/or improvement in his general condition during a 4 to 12-week trial therapy. In addition, nationally and internationally applicable guidelines should be included in the considerations surrounding an indication. For example, the guideline on “Long-term use of opioids for chronic non-tumor-related pain (LONTS)” [9] of the German Pain Society represents a recommendable resource. Currently, long-term therapy with an opioid is recommended only in the presence of painful diabetic polyneuropathy. In contrast, long-term therapy with opioids is even specifically discouraged in the case of various other chronic pain conditions (see also Table 1).
In case of doubt: the i.v. opioid test as a signpost
If there is uncertainty about whether pain therapy with opioids should be continued for longer than 12 weeks, an intravenous (i.v.) opioid test performed in an outpatient setting can be helpful [10] (Fig. 2). Such tests are offered in Switzerland by various pain medicine centers. By protocolized i.v. administration of an ultra-short-acting opioid, it is usually possible to determine whether or not a pain condition can be effectively treated by an opioid.
Short-acting vs. long-acting opioid preparations
For the treatment of chronic pain, preparations with retarded galenics or long duration of action should be used if possible. The intake should follow a fixed schedule. Experience shows that better pain control and better therapy adherence can be achieved in this way. Furthermore, this procedure can reduce the risk of complications.
Short-acting and ultra-short-acting opioids should be used only in exceptional circumstances in the treatment of non-tumor-related chronic pain. They are also not recommended as an on-demand medication. Clinical experience shows that short-acting opioids can rapidly lead to psychological dependence as well. Unfortunately, this often results in misuse.
Outcomes of long-term opioid therapy
The scientific evidence currently available to assess the effectiveness of opoid therapy >120 days with respect to nontumor-related chronic pain is insufficient. This automatically implies uncertain prospects for success [11].
In the context of chronic use of opioids, it is not uncommon for the opioid medication used to decrease in effectiveness. There are several differential diagnoses that may explain this development. Even in the case of non-tumor related chronic pain, disease progression can occur, leading to an increase in pain problems. However, chronic opioid treatment often leads to the development of tolerance with a consequent reduction in the analgesic effect of the opioid used. The cause is thought to be a migration of opioid receptors from the cell surface to the interior of the cell, so that they are no longer available for the analgesic effect. Another phenomenon that may occur in association with an increase in pain during ongoing therapy with opioids is opioid-induced hyperalgesia. The discussed mechanisms of development of opioid-induced hyperalgesia are complex and range from down-regulation of opioid receptors to possible central sensitization and synaptic long-term potentiation.
Adverse effects with long-term use
Long-term use of opioids may result in the following adverse effects:
- Loss of sexual desire
- Impotence
- Female cycle disorders
- Increased all-cause mortality
- Passivity/listlessness
- Memory disorders
- Increased risk of falling
When should long-term opioid therapy be stopped?
Long-term therapy with an opioid should be reevaluated periodically. If it is unclear whether therapy with an opioid is providing pain relief, work toward discontinuation of that therapy. It is recommended that therapy with an opioid be gradually discontinued if:
- During the discontinuation phase (4 to 12 weeks), the individually defined therapy goals were not achieved and/or significant side effects occurred.
- In the course of treatment, a loss of efficacy of the opioid used must be detected and this cannot be further prevented by a moderate adjustment of the dose or a change to another opioid.
- Evidence of misuse occurs during treatment (independent dose increases, prescription by multiple physicians).
Conclusion
Opioids represent one of the most important classes of substances for the treatment of severe pain. They are never used as a first-line option and should always be accompanied by non-drug interventions. Long-term therapy is only given to therapy responders, and the effect must be evaluated regularly by defining and monitoring therapy goals. Non-functioning therapy with opioids must be terminated in a timely manner.
Take-Home Messagess
- Before starting pharmacological pain therapy in general and treatment with opioids in particular, the underlying pain mechanism must be narrowed down.
- Opioids are often the treatment of choice for severe acute and tumor-related pain.
- In contrast, long-term therapy of non-tumor-related chronic pain should be exceptional and combined with non-drug measures whenever possible.
- Long-term opioid therapy must be guided by measurable goals. If these goals are not met, opioid treatment should be suspended.
- In the course of long-term therapy with opioids, a physical dependence always develops, which is sometimes accompanied by a psychological component, in the sense of an addiction.
Literature:
- Ossipov MH, Dussor GO, Porreca F: Central modulation of pain. J Clin Invest 2010; 120: 3779-3787.
- Swiss Health Interview Survey 2017, Health and Gender, Swiss Federal Statistical Office, FSO number 213-1718. 2020.
- Wertli MM, Steurer J: In Process Citation. Practice 2015; 104(11): 541-542.
- Breivik H, Stubhaug A: Burden of disease is often aggravated by opioid treatment of chronic pain patients: Etiology and prevention. PAIN 2014; 155(12): 2441-2443.
- Wertli M, Held U, Signorell A, et al: Analysis of the development of pain and sleep medication prescribing practices between 2013 and 2018 in Switzerland. University Hospital Bern 2020.
- Jensen T, Baron R, et al: A new definition of neuropathic pain. Pain 2011; 152: 2204-2205.
- Trouvin AP, Perrot S: New concepts of pain. Best Practice & Research Clinical Rheumatology 2019; 33(3).
- Maurer K: Practicable step therapy for the family physician. The Informed Physician 2017.
- Long-term use of opioids for chronic nontumor-related pain (LONTS), 2nd update 2020; AWMF guideline registry no. 145/003.
- Gustorff B: Intravenous opioid testing in patients with chronic non-cancer pain. Eur J Pain 2005; 9(2): 123-125.
- Chou R, Turner JA, et al: The Effectiveness and Risks of Long-Term Opioid Therapy for Chronic Pain: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop. Ann Int Med 2015; doi: 10.7326/M14-2559.
InFo PAIN & GERIATry 2021; 3(1): 10-14.