For tumors in the head and neck region, the functional and esthetic deficits must be weighed against the prognostic advantage when planning therapy. A variety of restorative options are available as part of surgical therapy, so that both structural integrity and partial function can be reconstructed even in large resection areas. The various forms of fabric flaps (displacement flaps, pedunculated flaps, free flaps) have different advantages and disadvantages. In principle, the resection of the primary tumor and the reconstruction of the defects should be performed by experienced ENT specialists. neck and face surgeons at centers qualified for this purpose.
The area of the head and neck has a high level of complexity from both an anatomical and functional point of view. For example, the larynx not only generates the voice, but the separation between the airway and the foodway also occurs here. Impairment of these functions would lead to aspiration and consequent inability to swallow. The tongue and base of the tongue also perform several functions, including articulation, food transport, and swallowing. The coordination of these partly voluntary, partly involuntary movements requires a highly complex interplay of different cranial nerves running in the surrounding soft tissues.
In the context of the treatment of tumors of the head and neck region, these functional and anatomical peculiarities must be included in the planning of the therapeutic concept. In this context, the functional deficits to be expected after treatment must be weighed against the prognostic advantage. Contrary to a widespread opinion, it must be stated that these deficits can occur after primary surgical therapy as well as after primary and/or adjuvant radio(chemo)therapy. Even with extensive laryngeal carcinoma, the larynx can often be structurally preserved with primary radiochemotherapy. However, postradiogenic fibrosis, which develops in a not insignificant percentage, often results in the larynx and adjacent structures no longer having sufficient mobility, so that functionally both speech and swallowing are no longer possible. In such cases, laryngectomy must be evaluated to restore swallowing function and partial recovery of speech function using a replacement voice.
In the context of surgical therapy, various reconstructive options are available to reconstruct even larger resection areas in terms of structural integrity as well as function. In the following, some frequently used examples will be explained in more detail.
General information about plastic reconstructions
In principle, plastic reconstruction is performed in situations where primary wound closure is no longer possible or would lead to functional or aesthetic limitations. The basic principle is based on the use of tissue flaps, be they local displacement flaps, pedicled flaps or free microvascular anastomosed flaps. The latter have a defined vascular supply consisting of at least one artery and one vein. Pedicled flaps have the advantage of eliminating the need to anastomose the vessels and complications such as vascular thrombosis usually do not occur. In return, other restrictions must be expected depending on the situation.
Cutaneous, myocutaneous, or osteomyocutaneous flaps are differentiated according to the quality and quantity of the tissue. Depending on the location of the tissue defect, the nature of the structure to be reconstructed as well as its function, various surgical options are available in the head and neck region. Due to the complexity of these procedures, resection of the primary tumor and reconstruction of the defects should only be performed by experienced ENT or neck and face surgeons at centers qualified to do so.
Frequently used pedunculated flaps in the head and neck region
Forehead flap: The pedunculated, myocutaneous frontal lobe is mainly used for reconstruction of the nose (predominantly in the tip area). In this procedure, a vertically (median/paramedian) or obliquely oriented skin-muscle area of the forehead supplied by the supraorbital artery is incised and pivoted caudally onto the nasal region to be reconstructed. There the suture is made to the edges of the defect. The bulging vascular pedicle, prominent in the medial corner of the eye, can be transected after autonomization and local revascularization of the nasal skin. Depending on the aesthetic situation, this is reinserted back into the skin of the forehead or resected entirely. If necessary, the flap can be thinned out and further adapted to the anatomy, so that aesthetically and functionally satisfactory results can be achieved in the vast majority of cases.
Temporalis lobe: The temporalis muscle draws its blood supply from the superficial temporal artery and vein and from the maxillary artery. The desired flap portion is prepared up to the zygomatic arch (serves as a hypomochlion), remains pedunculated at this point, and is pivoted into the defect zone from there. This may involve reaching the lateral base of the skull, the orbit, or the oral cavity for reconstruction. A narrow temporalis flap is also used in each case for temporalis reinsplasty of the corner of the mouth and/or lateral corner of the eye performed in the context of complete facial nerve palsy. In the process, a narrow rein of the temporalis muscle swiveled to the corner of the mouth is adapted to the muscles surrounding the mouth in a ring shape under traction. This raises the paretic corner of the mouth in the sense of a static muscle sculpture. This allows a high percentage of functional and esthetic deficits to be compensated.
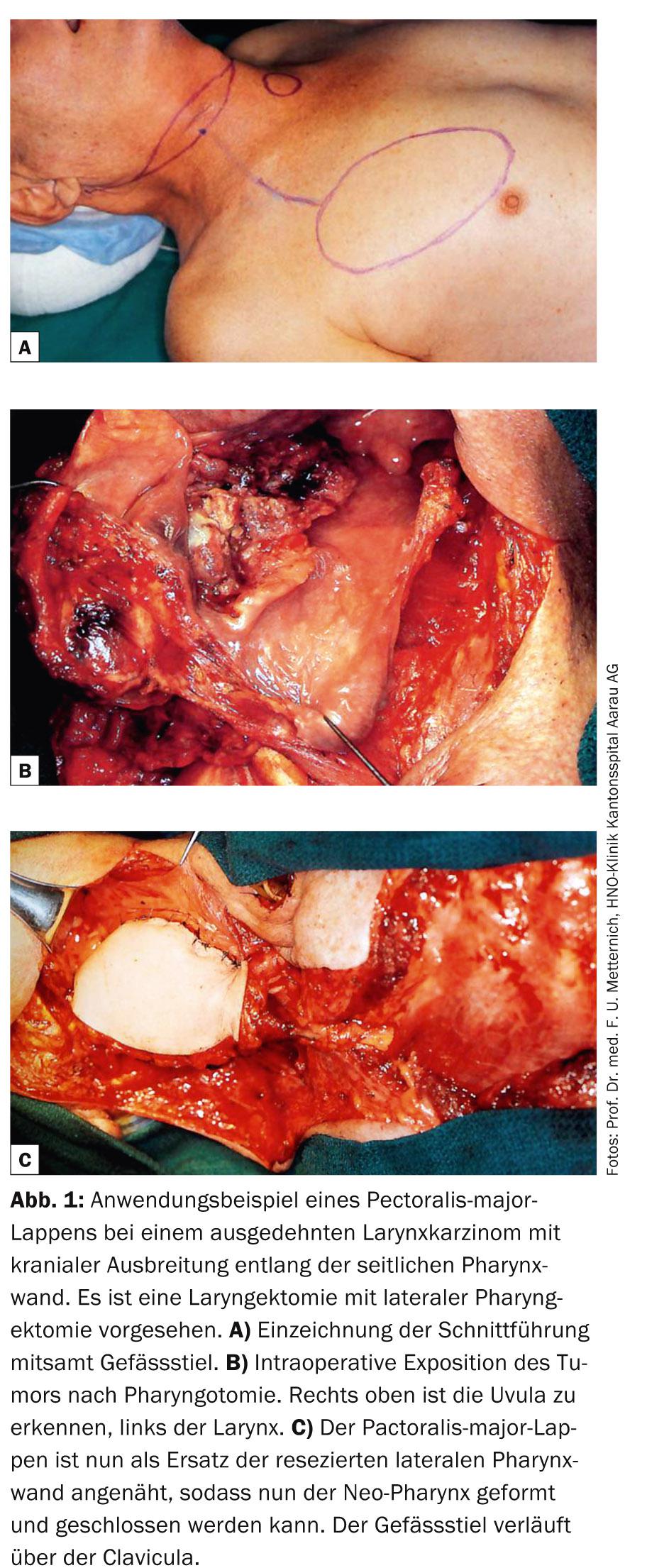
Pectoralis-major flap (Fig. 1): The pectoralis-major flap (PML) can be used as a myofascial or myocutaneous pedicled flap for a variety of defects. The vascular course of the pedicle (thoracoacromial artery and vein) is very constant, and the numerous anastomoses allow the required flap area to be variably adapted to the defect. The pedicle is dissected up to the clavicle, which allows the flap to be pivoted to the oropharynx after subcutaneous tunneling. Due to the thickness of the muscle, the PML is predominantly used where appropriate volume and stability are desired, for example in larger defects of the floor of the mouth, oropharynx and hypopharynx, but also in reconstructions of the soft tissues of the neck. The PML is often used as part of salvage surgery after previous radio(chemo)therapy. After salvage laryngectomy, additional coverage of the reconstructed pharynx with PML can significantly reduce the risk of pharyngo-cutaneous fistula formation.
Latissimus dorsi flap: The latissimus dorsi flap can be obtained either as a myocutaneous flap or as a pure muscle flap. Due to the achievable skin area and muscle thickness, this flap is used wherever large and deep defects need to be covered, for example in extensive resections in the orbita and paranasal sinuses. Wound healing is very good due to the strong blood supply to the muscle, so it can also be used for infected surgical cavities. The flap can be pedicled or freely microvascularized for defect reconstruction. The vascular supply is via the thoracodorsal artery and vein.
Commonly used microvascular anastomosed flap
Like the PML, the fasciocutaneous forearm radial flap (URL) (Fig. 2) can be used for a wide variety of reconstructions in the head and neck region and is one of the most commonly used grafts. Unlike the PML, the URL is thinner and can be modeled for more complex reconstructions. Nevertheless, the mechanical load capacity is high, so that the flap is also used for movable regions such as the tongue and soft palate. The flap, which varies in size, is removed from the palmar side of the forearm, with the radial artery and accompanying vein serving as the vascular pedicle. Microvascular anastomosis is performed cervically to a branch of the external carotid artery and a cervical vein. The defect on the forearm is covered by split skin or primarily closed by an appropriate incision with tissue mobilization. It is not uncommon for spontaneous resensitization of the graft to occur. This additionally contributes to successful swallowing rehabilitation after tumor resections in the oral cavity and pharynx.

Plastic reconstruction after resection of skin tumors
For the sake of completeness, the reconstruction options after resection of more extensive skin tumors in the head and neck region should also be mentioned. Depending on the extent of the resection area, local displacement flaps or local pedicled flaps can be used in most cases. In cases of not too large concave wound surfaces in the area of the facial soft tissues, spontaneous wound healing, under medical control, leads in many cases to very good cosmetic results. For larger wound cavities involving soft tissues and extradermal structures such as muscles or salivary glands, appropriately larger flaps are used, such as the PML or latissimus dorsi flap.
Take-Home Messages
- In the case of carcinomas of the head and neck, the complex anatomical and functional conditions must be taken into account when planning therapy.
- Functional deficits can occur after both surgical therapy and radiotherapy.
- Various tissue flaps are available for the structural and functional reconstruction of tissue defects after tumor resection.
- Pedicled flaps are less prone to complications, but free microvascularized flaps are sometimes easier to sculpt according to the required shape and function.
- The resection of the primary tumor and the reconstruction of the defects should be performed by experienced ENT- resp. Neck and facial surgeons at centers qualified for this purpose.
Thomas Mantei, MD
Prof. Dr. med. Frank Uwe Metternich
Further reading:
- Bootz F, Keiner S: Pedicled and free flaps for reconstruction of the head and neck region. HNO 2005; 53: 316-324.
- Remmert S: Reconstruction of large defects of the tongue. HNO 2001; 49: 143-157.
- Herberhold S, Bootz F: Reconstruction in the oropharynx. HNO 2013; 61: 580-585.
- Sakuraba M, et al: Recent advances in reconstructive surgery: head and neck reconstruction. Int J Clin Oncol 2013; 18: 561-565.
- Ayshford C, et al: Reconstructive techniques currently used following resection of hypopharyngeal carcinoma. J Laryngol Otol 1999; 113: 145-148.
- Welkoborsky H, et al: Reconstruction of large pharyngeal defects with microvascular free flaps and myocutaneous pedicled flaps. Curr Opin Otolranygol Head Neck Surg 2013; 21: 318-327.
- Rigby M, Taylor S: Soft tissue reconstrucion of the oral cavity: a review of current options. Curr Opin Otolranygol Head Neck Surg 2013; 21: 311-317.
InFo ONCOLOGY & HEMATOLOGY 2014; 2(10): 12-15.