With rapid technological advances in radiation oncology, new treatment options are now available to patients with prostate cancer, both in the primary therapy and in the metastatic setting. In particular, body stereotaxy is a promising approach: The therapy, which can be performed on an outpatient basis within one to two weeks, is characterized by high precision and consequently very good local efficacy and by a favorable side effect profile. However, the high complexity of this precision radiotherapy requires the presence of appropriate technologies, an excellently trained and experienced multiprofessional team, and close interdisciplinary collaboration to achieve safe application.
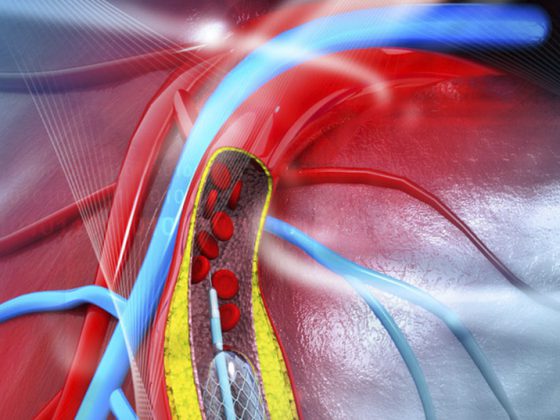
Percutaneous radiotherapy is an established treatment option for localized prostate cancer that is equivalent to surgical procedures. The so-called percutaneous radiation is the most frequently used treatment method and numerous technical advancements have revolutionized radiotherapy of prostate carcinoma in recent years. Intensity-modulated radiation therapy (IMRT) is now an established standard in most centers and allows the radiation dose to be precisely adapted to the tumor. Prior to any radiation treatment, image-guided radiotherapy (IGRT) can be used to determine the exact position of the prostate. Even during the radiation session, electromagnetic transponders, for example, can be used to monitor the movements of the prostate and the targeting accuracy of the treatment. Current concepts try to determine the so-called dominant tumor lesion in the prostate with multiparametric MRI imaging and to irradiate it in a focused manner. Today, these methods allow highly precise targeting of the tumor while sparing the bladder and especially the rectum.
In the meantime, first long-term results are available for the methods of high-precision radiotherapy. These confirm the theoretical superiority of precise irradiation and consistently demonstrate excellent biochemical control with, in particular, reduced rectal side effects [1,2].
Hypofractionated radiotherapy
Traditionally, percutaneous radiotherapy is performed in so-called conventional fractionation. For local control of prostate carcinoma, a radiation dose of 74-80 Gy is necessary: This radiation dose is divided into individual radiation sessions of 2 Gy, so that the entire therapy extends over 37-40 irradiations and a period of eight weeks. This conventional fractionated irradiation has been the gold standard for decades, as it exploits radiobiological differences between tumor cells and normal tissue. However, evidence has been accumulating for several years that prostate cancer is very sensitive to fractionation and overall duration of treatment and, unlike most other tumors, no benefit is obtained from conventional fractionation. On the contrary, hypofractionation, i.e., irradiation with fewer irradiation sessions and simultaneously higher individual doses, could even improve the therapeutic breadth or at least result in no worse outcomes. Patient time and radiooncology resource consumption could be reduced.
Radiobiological findings and technological advancements in radiation therapy have been the basis for numerous randomized trials comparing conventional versus hypofractionated radiation. For the so-called moderate hypofractionation, partly final [3,4], partly preliminary acute toxicity data are available [5,6]. Shortening radiation from seven to eight weeks to four to six and a half weeks does not appear to affect tolerability and may be a safe alternative to conventional fractionation. In terms of biochemical control, equivalence is also emerging, but long-term results of important studies are still pending [7].
Primary body stereotactic irradiation.
Body stereotactic radiation (SBRT) is the extreme form of high precision radiotherapy and hypofractionation. Radiation is administered in only four to five sessions, which are applied within one to two weeks. The requirements for the precision of radiation therapy are even higher. Thus, all studies use methods to compensate for or minimize intrafractional prostate motion, thus achieving millimeter precision of irradiation.
Randomized trials of body stereotaxy are still pending, but a joint analysis of several prospective phase II trials has collected results from a total of 1100 patients [8]. The patients had all been treated with five SBRT sessions, with total doses varying between 35-40 Gy. In the low-risk (n=641; median follow-up 36 months) and intermediate-risk (n=334; median follow-up 30.5 months) patients, 5-year PSA control was promising at 95% and 95%, respectively. 84%. The validity for high-risk patients is limited by the short follow-up period (23 months) and the small number of patients (n=125).
The tolerability of SBRT is good. However, extremely high irradiation doses of 5× 10 Gy exceed the tolerance of the rectum and must be avoided [9]. An analysis based on the SEER database had recently shown that compared with conventionally fractionated irradiation, stereotactic irradiation did not cause increased rectal side effects [10]. However, an increased rate of urogenital side effects was observed, particularly strictures of the urethra. A final assessment of SBRT is therefore not yet possible. Consequently, this complex form of high-precision radiotherapy should currently only be offered and evaluated by specialized centers.
Body stereotactic irradiation in the oligometastatic situation.
In the metastatic setting, anti-hormonal therapy (AHT) is the first-line treatment of choice. However, in cases of limited asymptomatic metastasis, delayed initiation of AHT with active clinical surveillance is an option [11]. In the case of very low metastatic load, an oligometastasis, it is therefore currently being investigated whether local therapy can delay the start of AHT and prolong progression-free survival. Especially due to the widespread use of choline PET, we currently see patients with solitary lymph node or bone metastasis more frequently and it must be expected that this clinical situation will become even more common when the PSMA tracer becomes available [12].
In this situation, body stereotactic radiation is a highly effective and well-tolerated treatment. The methodology of radiotherapy is currently not sufficiently standardized, especially with regard to the target volume (elective nodal irradiation), the irradiation dose and the combination with subsequent AHT. Nevertheless, a systematic review reported a progression-free survival of 50% at one to three years [13]. Grade 3 toxicities occurred in <1% of patients and grade 2 adverse events in 8.5%.
Randomized trials of local therapy in the metastatic stage are still pending, but due to the favorable side effect profile, this option may be offered to selected patients when systemic therapy is rejected. A high level of radiation oncology expertise in body stereotactic irradiation is a basic requirement due to the variability of metastasis localization and adjacent organs at risk.
Finally, such innovative concepts as well as the decision on primary therapy (e.g., surgery vs. radiotherapy) should be discussed in a specialized interdisciplinary center and there should be an equally interdisciplinary consultation with the patient.
Literature:
- Spratt DE, et al: Long-term survival and toxicity in patients treated with high-dose intensity modulated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2013; 85: 686-692.
- Fonteyne V, et al: Clinical results after high-dose intensity-modulated radiotherapy for high-risk prostate cancer. Advances in Urology 2012; 2012: 368528.
- Arcangeli S, et al: Updated results and patterns of failure in a randomized hypofractionation trial for high-risk prostate cancer. Int J Radiat Oncol Biol Phys 2012; 84: 1172-1178.
- Pollack A, et al: Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol 2013; 31: 3860-3868.
- Fonteyne V, et al: Hypofractionated high-dose radiation therapy for prostate cancer: long-term results of a multi-institutional phase ii trial. Int J Radiat Oncol Biol Phys 2012; 84: e483-e490.
- Aluwini S, et al: Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (hypro): Acute toxicity results from a randomised non-inferiority phase 3 trial. The Lancet Oncology 2015; 16: 274-283.
- Koontz BF, et al: A systematic review of hypofractionation for primary management of prostate cancer. Eur Urol 2015 Oct; 68(4): 683-691.
- King CR, et al: Stereotactic body radiotherapy for localized prostate cancer: pooled analysis from a multi-institutional consortium of prospective phase ii trials. Radiother Oncol 2013; 109: 217-221.
- Kim DW, et al: Predictors of rectal tolerance observed in a dose-escalated phase 1-2 trial of stereotactic body radiation therapy for prostate cancer. Int J Radiat Oncol Biol Phys 2014; 89: 509-517.
- Yu JB, et al: Stereotactic body radiation therapy versus intensity-modulated radiation therapy for prostate cancer. J Clin Oncol 2014; 32(12): 1195-1201.
- Heidenreich A, et al: EAU guidelines on prostate cancer. Part ii: Treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 2014; 65: 467-479.
- Afshar-Oromieh A, et al: The diagnostic value of pet/ct imaging with the (68)ga-labeled psma ligand hbed-cc in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 2015; 42: 197-209.
- Ost P, et al: Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: A systematic review of the literature. Eur Urol 2015; 67: 852-863.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(11-12): 11-13