Antiphospholipid syndrome (APS) is an acquired thrombophilia and is associated with a high risk of venous, arterial or microvascular thrombosis. In APS with thrombotic manifestations, lifelong anticoagulation is generally indicated. According to current data, vitamin K antagonists (VKA) or low-molecular-weight heparin should be used for this purpose.
Patients with antiphospholipid syndrome (APS) are particularly prone to deep vein thrombosis of the leg, pelvis or arm, pulmonary embolism and stroke. It can also lead to pregnancy complications (premature abortions and births). APS can occur in isolation (primary APS) or be associated with an underlying disease such as SLE or malignancies (secondary APS). The latter also includes drug-induced APS. In the ACR/EULAR APS classification criteria updated in 2023, the range of clinical features was expanded and a new definition of pregnancy complications was introduced [1,2]. Accordingly, the prerequisites for classification as APS are that the entry criteria are met (at least 1 clinical and 1 laboratory criterion within 3 years) and at least 3 points from the clinical areas and 3 points from the laboratory area are achieved [1,2]. Lupus anticoagulant (LA) is considered the strongest predictor of APS, followed by anticardiolipin antibodies (aCL) and β2-glycoprotein I antibodies (aβ2GPI). To achieve sufficient sensitivity, it is recommended to perform all three antibody (Ak) tests; LA preferably not during the acute thromboembolic event. As antiphospholipid-Ak can occasionally occur only temporarily (e.g. in the context of infections), repeated testing and proof of antibody persistence over at least 12 weeks is recommended [3]. In terms of risk classification, a triple positive antibody profile (LA+, anticardiolipin-Ak+, ß2-glycoprotein I-Ak+) represents a high-risk constellation [9]. The constellation of positive LA with or without anticardiolipin-Ak or ß2-glycoprotein I-Ak (single or double positivity with LA) is also associated with a high risk. A medium risk is associated with negative LA and moderate or high titres of anticardiolipin-Ak and/or ß2-glycoprotein I-Ak (single or double positivity without LA). The constellation of low negative LA with low titres of anticardiolipin-Ak and/orß2-glycoprotein I-Ak (single or double positivity without LA) is classified as low risk [9].
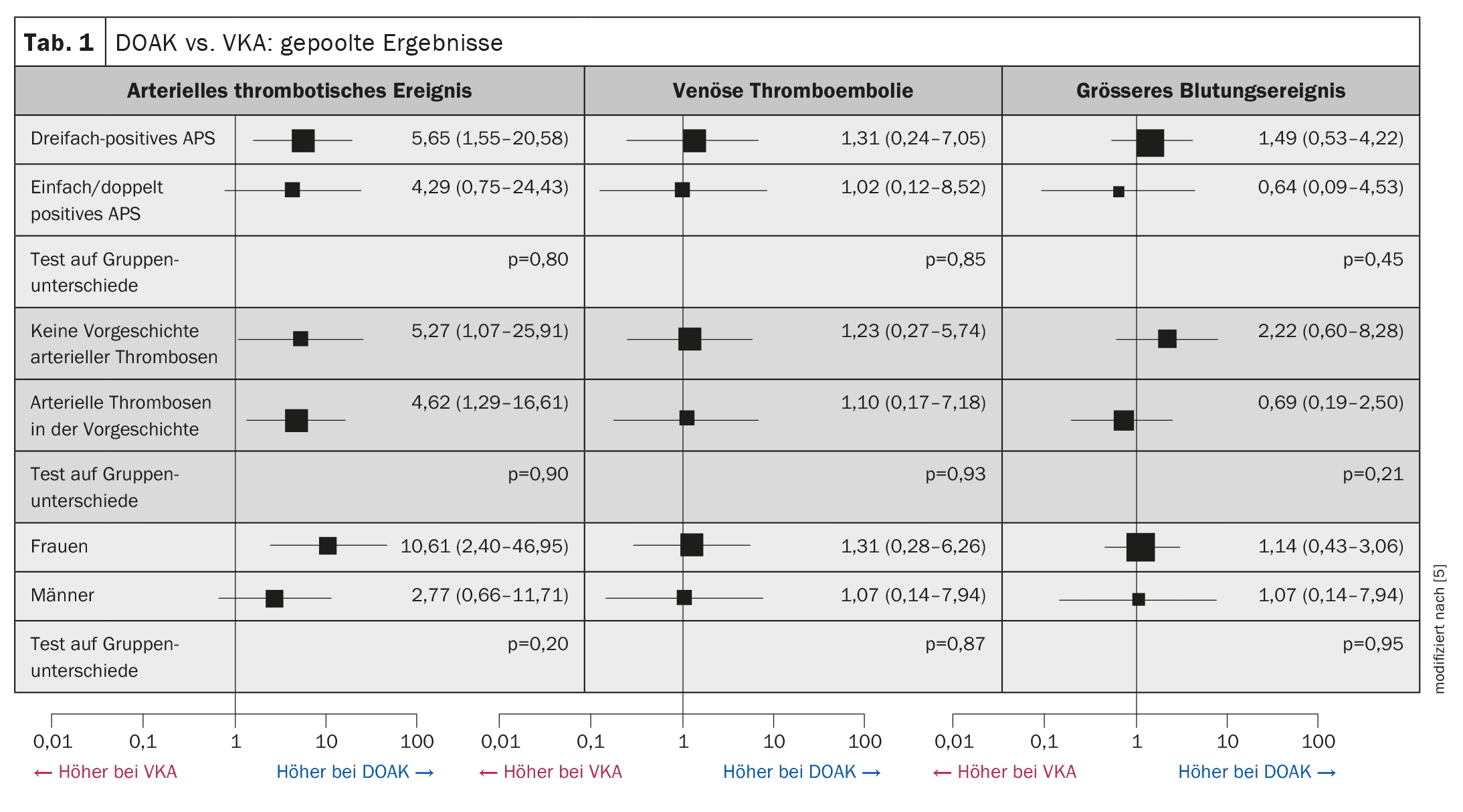
Meta-analysis evaluated current evidence
Prof. Dr. Hannah Cohen from University College London (UCL) presented a meta-analysis published in 2023, in which the use of DOAC vs. VKA/warfarin in APS was evaluated using randomized controlled trials (RCTs) [4,5]. Four open, randomized controlled trials with 472 patients were included. The statistical analyses showed that APS patients randomized to DOAC had an increased risk of arterial thrombosis compared to VKA, while there were no significant differences in the risk of VTE or major bleeding events (Table 1) [5]. The odds ratio (OR) for arterial thrombotic events, in particular stroke, was 5.43 (95% CI: 1.87-15.75; p<0.001, I2=0%), which corresponds to a significantly increased risk with DOAC compared to VKA. In contrast, the corresponding ORs for a VTE were 1.20 (95% CI: 0.31-4.55; p=0.79, I2=0%) and for a major bleeding event 1.02 (95% CI: 0.42-2.47; p=0.97; I2=0%), which means that these differences were relatively small and did not reach the significance level. The differences in the risk of arterial thrombotic events could neither be explained by corresponding events in the medical history, nor by triple positive antibody detection or phenotypes of antiphospholipid antibodies, the speaker explained and pointed out, that the international specialist societies ISTH (International Society on Thrombosis and Haemostasis), ICAPA (International Congress on Antiphospholipid Antibodies Taskforce) and EULAR (European League Against Rheumatism) recommend avoiding the use of DOACs in APS-associated arterial thrombosis [4,6–8]. The use of DOACs is generally not recommended for triple-positive high-risk patients.
Congress: EHA2024
Literature:
- Barbhaiya M, et al.: ACR/EULAR APS Classification Criteria Collaborators. The 2023 ACR/EULAR Antiphospholipid Syndrome Classification Criteria. Arthritis Rheumatol 2023; 75(10): 1687–1702.
- Barbhaiya M, et al.: ACR/EULAR APS Classification Criteria Collaborators. 2023 ACR/EULAR antiphospholipid syndrome classification criteria. Ann Rheum Dis 2023; 82(10): 1258–1270.
- «Diagnostik und Therapie der Venenthrombose und Lungenembolie», S2k-Leitlinie, Version: 5.5 Stand: 14.02.2023, valid until: 13.02.2028.
- «Challenges in management of thrombotic antiphospholipid syndrome», Prof. Dr. Hannah Cohen, EHA2024, Madrid, 13.6.–16.6.2024.
- Khairani CD, et al.: Direct Oral Anticoagulants vs Vitamin K Antagonists in Patients With Antiphospholipid Syndromes: Meta-Analysis of Randomized Trials. J Am Coll Cardiol 2023; 81(1): 16–30.
- Zuily S, et al.: Use of direct oral anticoagulants in patients with thrombotic antiphospholipid syndrome: Guidance from the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost 2020; 18(9): 2126–2137.
- Cohen H, et al.: 16th International Congress on Antiphospholipid Antibodies Task Force Report on Antiphospholipid Syndrome Treatment Trends. Lupus 2020; 29(12): 1571–1593.
- Tektonidou MG, et al.: EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis 2019; 78(10): 1296–1304.
- Bauersachs R, et al.: Therapie des Antiphospholipid-Syndroms (APS) mit DOAKs. Hamostaseologie 2019; 39(03): 298–300.
HAUSARZT PRAXIS 2024; 19(11): 50-51 (published on 25.11.24, ahead of print)