History: The 19-year-old female patient with no family or personal history of allergic diseases had episodes of Quincke’s edema in the facial region in the last three months, which were accompanied by nausea, mild dizziness, obstructed nasal breathing and dyspnea.
Therefore, an allergological clarification (Dr. med. H.P. Baumgartner, FMH Dermatology, Zug) was performed, whereby routine inhalation and food allergens were negative. Serological examinations showed an increased IgE level of 374 E/ml and a slightly reduced C1 inhibitor protein of 0.1 and 0.14 g/l (normal value 0.15-0.35) when determined twice. Differential diagnosis was therefore thought to be hereditary angioedema (HAO), so that the general practitioner (M. Giger, M.D., Menzingen) referred the patient to the allergy ward of the Dermatology University Hospital for further investigation.
Further clarifications and course
Re-determination of C1 inhibitor again showed a low value of 0.08 g/ml (Laboratory of Clinical Immunology, USZ), but a normal C4 level of 0.21 g/l (norm 0.14-0.30) was found. Determination of C1 inhibitor function (Dr. P. Späth, Blood Donor Service SRC, Bern) showed a normal value of 129% (norm 60-140%), so that hereditary angioedema could be excluded. Allergic workup confirmed the elevation of serum IgE to 325 E/Ml, but broad prick and intradermal testing with inhalant and food allergens remained unproductive.
The patient was discharged with a suspected diagnosis of allergic Quincke’s edema. Because of the accompanying symptoms (nausea, dizziness, dyspnea), a hematogenously triggered Quincke’s edema (due to ingestion of a certain food) was suspected. In addition to being given an emergency kit consisting of 50 mg prednisone and antihistamine tablets and an epinephrine Medihaler spray, which was still available at the time, the patient was instructed to keep a detailed diary of previously ingested meals in the event of a recurrence.
The patient appeared a few weeks later stating that she had again suffered severe Quincke’s edema of the face after a “Zvieri” consisting of nut croissants and Ovaltine with milk. Since the patient had tolerated milk several times – even in the morning on an empty stomach – without any reaction and had performed a re-exposure with home-baked nut croissant herself, only Ovaltine remained as a suspicious cause for this Quincke’s edema episode.
In search of the allergen in Ovaltine
A scarification test with Ovaltine or Ovo-Sport bar (Fig. 1) was indeed positive, also with another chocolate drink (Hacosan).

In the search for the triggering ingredient in Ovaltine, intradermal tests were subsequently carried out with allergen extracts (unfortunately no longer available today!) from baker’s yeast, brewer’s yeast, peanuts, nuts, cocoa, almonds, malt and chocolate, but these proved negative. I therefore wrote to WANDER LTD, Berne, to ask if they could help me clarify this Ovaltine allergy and send me the various ingredients of the finished product. To my surprise, I then received the following letter from WANDER LTD: “We cannot imagine that any ingredient in OVOMALTINE would cause allergy, especially since this would be the first case in the 79-year history of OVOMALTINE consumption. By the way, it would hardly make sense for us to send you samples of all the raw materials of OVOMALTINE, because a number of them are commercial food ingredients that can be tested by direct consumption.” However, some raw materials of the Ovaltine were enclosed to me and further down in the letter it read further: “We would like to assist you in clarifying your patient’s possible allergy, and will provide you with additional materials if the allergen is not found in the initial selection of raw materials.” Instruction then followed: “Quincke’s edema can also be triggered by drugs. Furthermore, certain hair shampoos are allergenic. Recently, an acquaintance of the undersigned had a severe reddening of the face every time after using Selsun, a shampoo containing selenium disulfide. It is not necessarily the SeS2 that was the allergenic factor. It may just as well have been another ingredient. The hair shampoos used by the patient should therefore be included in the clarification.” And now the “key literature” for the allergist (!): “In the book by Richard Mackarness [BW note: founder of alternative “clinical ecology”]: Allergy to Food and Chemicals. Physical and mental disorders. Paracelsus Verlag, Stuttgart, 1980, 154 pages, SFr. 22.80 rare cases of food allergy are described. Perhaps this information will be useful to you. Sig. WANDER LTD”.
In any case, the dried malt extract from germinated barley supplied produced a very strong positive wheal reaction (Fig. 2) (scratch tests in control subjects were negative), but not the nutritional yeast or the cocoa powder. Malt extract makes up two-thirds of Ovaltine.

After questioning, the patient now stated that she had previously suffered skin swelling and similar reactions after eating other malt extract-containing snack products, such as Maltesers and Mars, but did not recognize the connection herself. She had never drunk beer.
Further allergological examinations
Since no reagents for in vitro diagnostics for specific IgE antibodies against malt extract were commercially available at that time, the patient serum and the malt extract were sent to Prof. S.G.O. Johansson (Karolinska Institutet, Stockholm), discoverer of IgE, to prepare a RAST disc. The subsequent RAST test against malt extract was positive with 1.2 PRU/l (Phadebas-Rast-Unit), corresponding to RAST class 2. Barley flour was also class 2 positive. Thus, it was clear that the first case of Ovaltine allergy was discovered after its introduction 79 years ago [1].
Diagnosis
Acute recurrent Quincke’s edema with shock fragments in IgE-mediated allergy to malt extract from germinated barley in a non-atopic female.
Further course
At a follow-up nine months after diagnosis, the patient stated that after elimination of malt-containing products she had suffered no more episodes of Quincke’s edema – with one exception, when she had again ingested a small bar of Ovo-Sport. She had experienced nausea after only five minutes, followed by Quincke’s edema of the face, which was immediately couped with emergency medication.
Comment
About two-thirds of cases of acute or acute-recurrent Quincke’s edema (without or with urticaria) can be causally clarified. Rarely ingested foods, medications, insect bites, and also parasites play a role here [2–4]. Pathogenetically, in addition to IgE-mediated allergy of the immediate type, pseudoallergic or intolerance reactions to antiphlogistics (ASA and NSAIDs), ACE inhibitors, and (more rarely) to additives must also be considered [2]. Recognition of hereditary or acquired angioedema due to C1 inhibitor deficiency is important because of its potentially lethal course [5,6]. When HAO is clinically suspected, immunologic measurement of complement system proteins, C1 inhibitor, and C4 factor, which is always decreased, even in the interval, is suitable for laboratory diagnosis; C4 may not be determinable in an acute attack. In the routine determination of the C1 inhibitor in external laboratories, the value can often be somewhat reduced for technical reasons, as in the present case, so that HAO is only likely to be present with a simultaneous strong reduction in the C4 complement factor. Functional determination of C1 inhibitor activity in a specialized laboratory can definitively confirm or exclude the diagnosis of HAO [5,6]. Allergic Quincke’s edema, unlike HAO, is always accompanied by itching, redness, and more often other symptoms of an allergic reaction (rhinitis, asthma, urticaria) and an increase in serum IgE levels. If the first allergological clarification is unproductive, it is often possible – as described above – to track down the triggering allergen on the basis of diary records and targeted allergological tests. Hair shampoos, on the other hand, do not trigger Quincke’s edema, but contract eczema due to late-type allergy with redness, vesicles, and collateral swelling [2].
In 1984, we succeeded for the first time (in the allergological literature accessible at that time, including standard textbooks, allergic reactions after consumption of foods containing malt were not documented) in describing an Ovaltine allergy due to sensitization to malt extract from germinated barley and, in collaboration with Prof. Gunnar Johansson, in establishing the specific IgE determination in the RAST test (f90) [1]. It should be mentioned in this case that the intradermal test with a commercial malt allergen – in contrast to the strongly positive scarification test with the native malt extract – was “false negative”. The patient with acquired malt allergy without atopic predisposition is a type C of the classification of food allergies [7]. This type C is more common than previously thought [8].
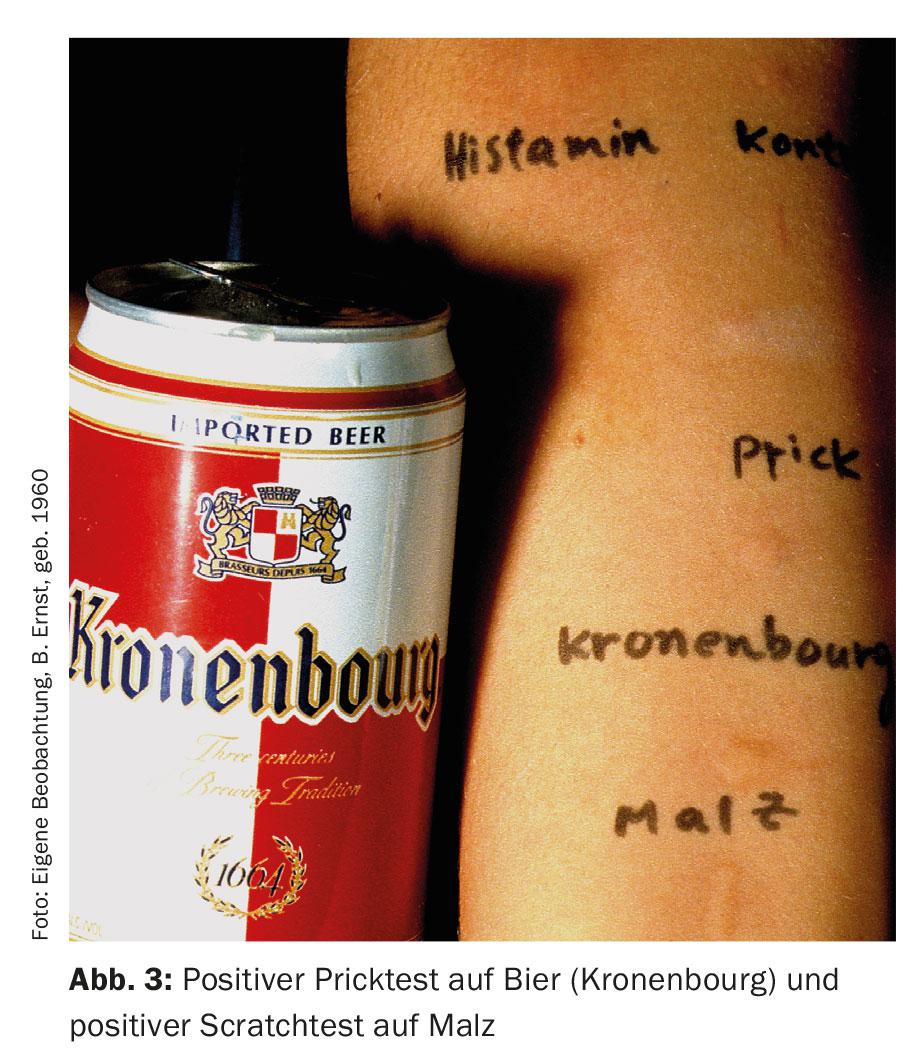
As a result, allergies to barley malt have been demonstrated several times. They occurred both in individuals who produced and processed malt (inhalant allergy) and as ingestive allergy mainly in beer drinkers [9–14] (Fig. 3).
Malt is grain that has been germinated and then dried (kilned) at higher temperatures. From an allergological point of view, brewing malt must be distinguished from baking malt. Brewing malt is made from barley, baking malt from wheat. The production of malt from rye, oats, corn and rice is much rarer. The malt used to brew beer is obtained from barley grains. The malting process produces malt sugar, proteins and many types of enzymes. This is why it is sometimes so difficult to identify the actual causative agent or the responsible allergen of the malt allergy. Two allergens could be characterized in barley malt: Hor v 1, a 14.5 kD protein, and Hor v 9, a 30 kD protein. Different IgE-binding allergens of 31-56 kDa have been described in malt and in barley. A major protein of 38 kDA was isolated from a beer extract [10]. In sera from patients with urticaria triggered by beer, 5-20 kDa allergens were further isolated from the beer protein fraction [11]. The barley allergen in beer is different from the 16 kDa in barley flour. The major barley allergen responsible for baker’s asthma is a 16 kDa barley protein.
In white beer allergy, especially in the sense of wheat-dependent effort-induced anaphylaxis [15], the determination of sIgE to omega 5 gliadin (Tri a 19, marker allergen) is pathognomonic [16].
Literature:
- Wüthrich B: Acute recurrent Quincke’s edema in allergy to malt extract. Schweiz Med Wschr 1984; 114: 269-271.
- Wüthrich B: Is Quincke’s edema present? Differential diagnosis to angioedema. DERMATOLOGIE PRAXIS 2012; 1: 24-26.
- Wüthrich B: What is your diagnosis? (Quiz): status after single allergic reaction with Quincke’s oedema (lips, tongue, hands) to crustaceans. DERMATOLOGIE PRAXIS 2011; 3: 38, 42.
- Wüthrich B: What is your diagnosis? (Quiz): Recurrent angioedema in strongyloidiasis. DERMATOLOGIE PRAXIS 2012; 1: 7, 12.
- Wüthrich B: What is your diagnosis? (Quiz): Hereditary angioedema type I.DERMATOLOGIE PRAXIS 2012; 2: 25, 40.
- Wüthrich B, Scheidegger P: The somewhat different case. Debunked: acquired angioedema in non-Hodgkin’s lymphoma. DERMATOLOGIE PRAXIS 2013; 3: 16-17.
- Pichler WJ: IgE-mediated food allergies. Classification based on sensitization pathway. Allergology 1998; 21: 441-450.
- Wüthrich B, Blötzer IC: IgE-mediated food allergy type C: the rarer type of food allergy? A casuistry of 16 cases. Act Dermatol 2004; 30: 95-102.
- Bonadonna P, et al: Beer-induced anaphylaxis due to barley sensitization: two case reports. J Investig Allergol Clin Immunol 1999; 9: 268-270.
- Figueredo E, et al: Beer-induced anaphylaxis: identification of allergens. Allergy 1999; 54: 630-634.
- Curioni A, et al: Urticaria from beer: an immediate hypersensitivity reaction due to a 10-kDa protein derived from barley. Clin Exp Allergy 1999; 29: 407-413.
- Garcia-Casado G, et al: Isolation and characterization of barley lipid transfer protein and protein Z as beer allergens. J Allergy Clin Immunol 2001; 108(4): 647-649.
- Neise U, Sennekamp J: Barley malt – a rare food allergen? Allergology 1996; 19: 135-138.
- Sieber W: Incident in the beer garden. The General Practitioner 2015; 37: 49-50.
- Herzinger T, et al: Anaphylaxis to wheat beer. Ann Allergy Asthma Immunol 2004; 92: 673-675.
- Wüthrich B, Hofer T: Food-induced exertion-induced anaphylaxis in severe sensitization to cereal proteins, especially to omega-5 gliadin, and in questionable house dust mite-crustacean syndrome. Allergology 2010; 33: 205-210.
DERMATOLOGY PRACTICE 2015; 25(6): 36-39
DERMATOLOGIE PRAXIS 2018 Special Edition (Anniversary Issue), Prof. Brunello Wüthrich











