Osteoporosis leads to an increased risk of fracture due to the loss of bone mass and density. The indication for therapy is mainly based on fracture history, bone density (DXA) and individual risk factors. The cut-off values of the DXA measurement that are relevant for drug interventions are age- and sex-dependent. The antiresorptive and osteoanabolic drugs available today can effectively reduce the risk of fracture.
For the question of which patient should be diagnosed and treated how, there are good and regularly updated guidelines of the umbrella organization Osteology (DVO), says Univ.-Prof. Dr. med. Martin Fassnacht, Head of Endocrinology and Diabetology, University Hospital Würzburg [1,2]. The DVO is an interdisciplinary association of scientific societies in Germany, Austria and Switzerland [2]. Osteoporosis a common disease that significantly affects quality of life. Regarding general prophylactic measures, the best possible counteraction should be taken against known risk factors, the speaker said. Those who exercise a lot and stress their skeleton thereby promote processes that stimulate the build-up of bone density. If underweight (65 years of age or older with a BMI <20), ensure adequate caloric intake. It is also extremely important to have an adequate calcium intake (100 mg/d) – ideally covered by the diet – as this promotes the stability of bone tissue [1]. It is also important to ensure an adequate supply of vitamin D, as this promotes the absorption of calcium and its incorporation into the bones. Particularly in the winter months, the amount of vitamin D supplied by the diet and produced by the body itself with the help of sunlight is not always sufficient. If the risk of falls/fractures is high, administration of 800-1000 IU vitamin D3/d is reasonable [1]. What else can be done prophylactically besides these measures? Since nicotine consumption has a negative effect on the risk of osteoporosis, it should be avoided. In patients taking fracture-promoting medications (e.g., glucocorticoids, antidepressants, neuroleptics, proton pump inhibitors), regular benefit-risk assessment of these medications is advised.
When is there an indication for specific osteoporosis medication?
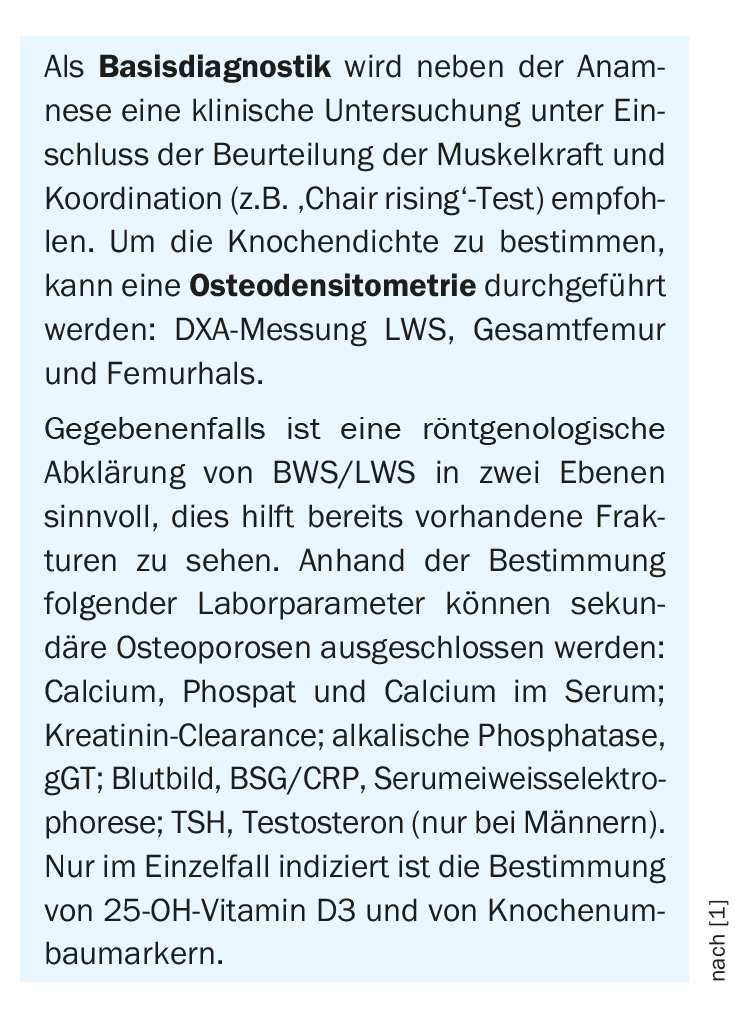
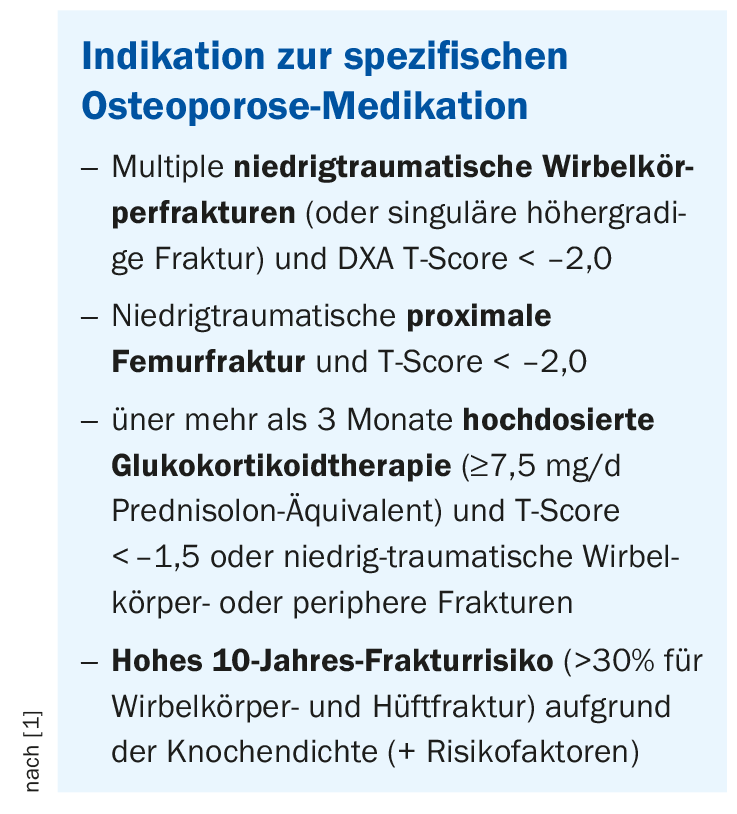
A 77-year-old previously spry woman tripped in the garden a few weeks ago and broke the neck of her thigh. After rehab, she comes to the doctor’s office with the question, “What can I do now so I don’t break my other femur, too?” Osteodensitometry should be performed as part of a basic diagnostic workup (box) to determine bone density. The cut-off values of bone density (T values) that are relevant for primary prophylaxis with medication are age- and sex-dependent. “The T-score is always the score compared to the population of 20-40 year olds, while the z-score is the score for peers,” explains Prof. Fassnacht. In low-traumatic proximal femur fracture, a T-score <2.0 is an indication for osteoporosis-specific medications. The same applies to multiple low-traumatic vertebral fractures (or singular higher-grade fractures) and to high-dose long-term glucocorticoid therapy (>3 months, ≥7.5 mg/d prednisolone equivalent) and a T-score < -1.50. In addition, osteoporosis-specific medications are indicated for high 10-year fracture risk (>30% for vertebral and hip fracture) based on bone density and certain risk factors (Box) .
Antiresorptive agents and denosumab as the first choice
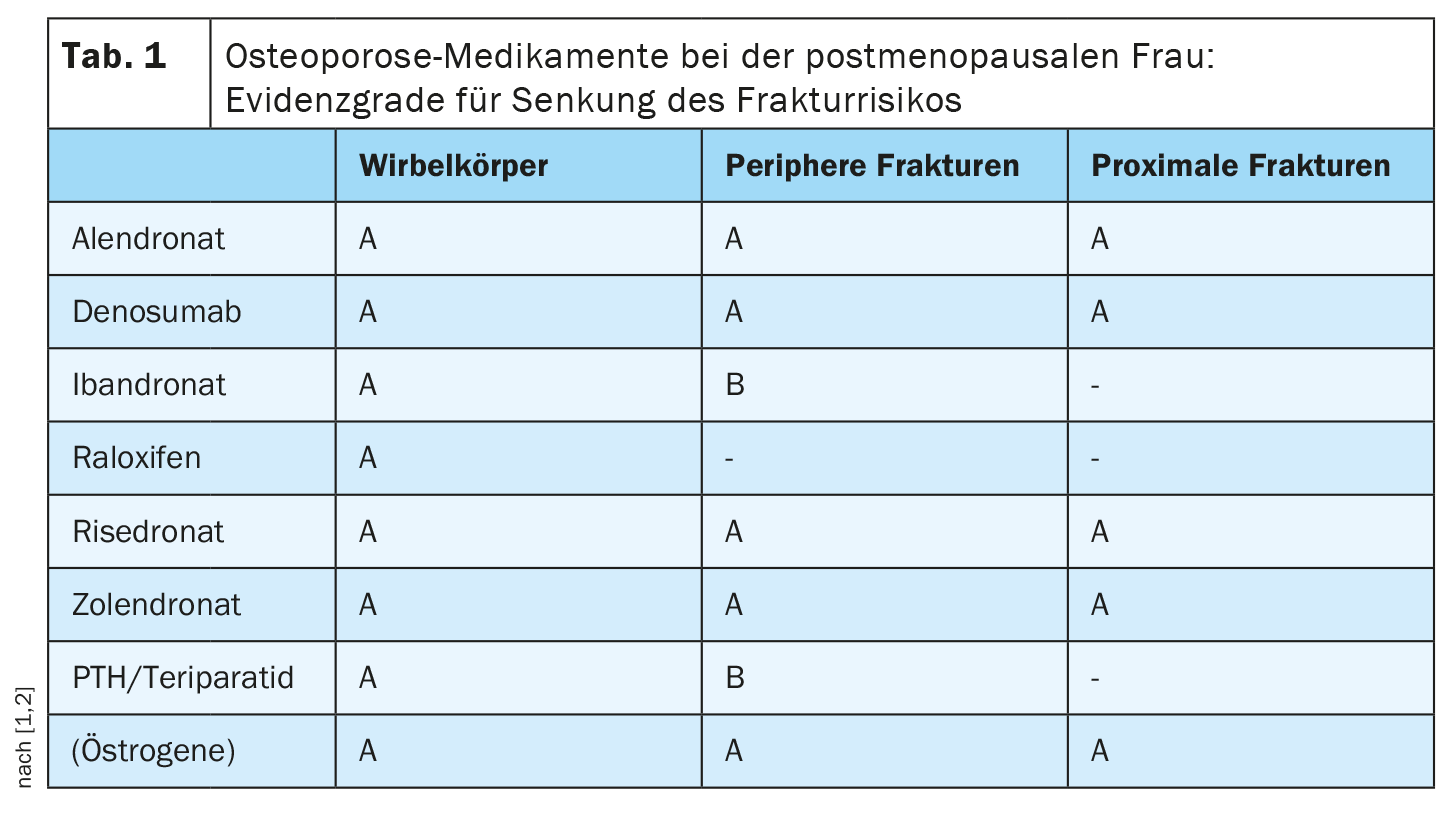
Fracture risk can be very effectively reduced by osteoporosis-specific medications, the speaker said. The agents available today can be classified as antiresorptive (inhibit bone resorption), osteoanabolic (promote bone formation), or dual-acting. Bisphosphonates (alendronate, ibandronate, risedronate, zoledronate) and denosumab are among the antiresorptive drugs and are still clearly first-choice drugs, Prof. Fassnacht explained. According to the guideline, several agents from different substance classes have an evidence level A for reducing the risk of proximal femur fractures and peripheral fractures (Table 1).
The number needed to treat (NNT) is very low at 13-22. It is important to discuss treatment options and any concerns about side effect risks with the patient, he said. The risk for gastrointestinal side effects can be reduced by taking the medication properly. Osteonecrosis of the jaw is often a major concern on the part of physicians, although the incidence (1:100,000) is very low. A dental check-up before starting therapy may be advisable. Furthermore, it should be considered that a benefit-risk evaluation of the osteoporosis-specific medication should be performed after every 3 to 5 years of therapy.
Literature:
- “Osteoporosis,” Univ. Prof. Martin Fassnacht, MD, freshup Family Medicine, Endocrinology 1, Dec. 16, 2022.
- S3-Guideline Prophylaxis, Diagnosis and Therapy of Osteoporosis, Umbrella Organization of German-speaking Scientific Osteological Societies
Societies (DVO), AWMF Register No.: 183/00, https://dv-osteologie.org/osteoporose-leitlinien,(last accessed Jan. 10, 2023).
HAUSARZT PRAXIS 2023; 18(1): 24-25