At the Dermatological Training Days in Zurich, various regional dermatoses were presented on the basis of case histories: How do dermatoses of the ear, diseases of the mucous membranes and thed mucosa and female genitalia or palmoplantar dermatoses? What are the (new) therapeutic options?
(ag) PD Dr. med. Thomas Kündig from the University Hospital Zurich presented dermatoses of the ear: “What one finds here again and again is, for example, otitis externa, the inflammation of the outer ear. It can be caused by maceration of the skin of the ear canal by means of fluid, but also by injuries, e.g. with cotton swabs, or by foreign bodies that have penetrated the skin and trigger an infection. Bacterial superinfection is mainly caused by Pseudomonas aeruginosa and Staphylococcus. Symptoms include otalgia in about 70%, somewhat less frequently itching, and less frequently (22%) hearing impairment.” For mild forms, topical antibiotics with topical steroids are used therapeutically; for severe forms, systemic antibiotics are used for Pseudomonas aeruginosa and Staphylococcus aureus. “Malignant otitis externa occurs primarily in immunodeficient patients and in diabetics. It manifests as invasive infection of the ear cartilage and bone, and often even facial paresis. A CT scan is also part of the diagnosis,” says the expert.
An exceptional example of ear dermatosis, which theoretically can also occur on other parts of the body, is the so-called “cell phone dermatitis”: Local dermatitis occurs in the ear area, which is attributed to nickel, which was sometimes still contained in the buttons of older cell phones [1].
Diseases of the oral mucosa
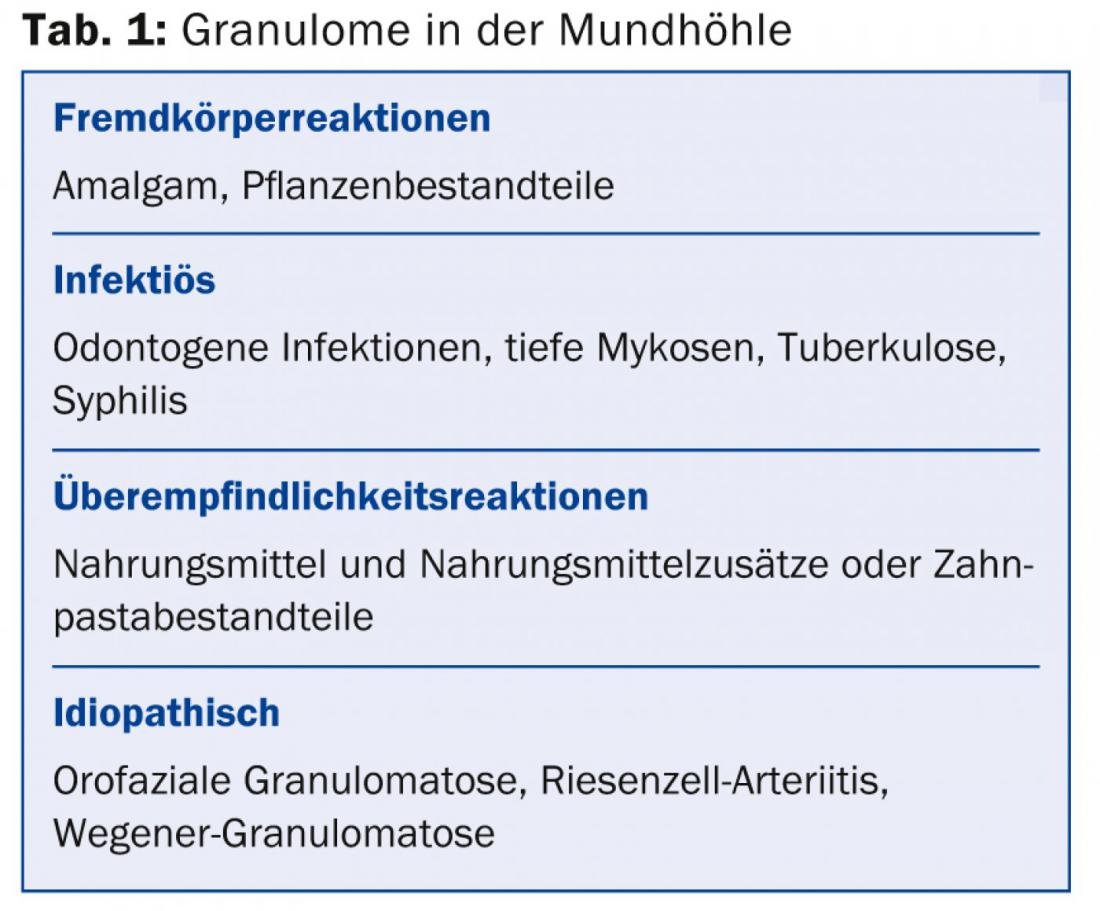
According to PD Dr. med. Jivko Kamarachev of the University Hospital Zurich, granulomas in the oral cavity can be either infectious, caused by foreign body or hypersensitivity reactions, or idiopathic (Table 1).
Orofacial granulomatosis, which Dr. Kamarachev presented in more detail, is an idiopathic constellation of symptoms. It manifests as recurrent or persistent swelling of the face and oral cavity, enoral mucosal changes, and histologically demonstrable, non-caseating, epithelioid cell granulomatous inflammation. “Orofacial granulomatosis” is therefore a descriptive umbrella term for Melkersson-Rosenthal syndrome, cheilitis granulomatosa (Miescher), orofacial manifestations of Crohn’s disease, and sarcoidosis.
“This condition is rare and is more common in children, adolescents, and young adults than in the elderly. 10-37% of cases are associated with Crohn’s disease. There are familial clusters, especially in Melkersson-Rosenthal syndrome. Otherwise, environmental influences such as intolerance to various foods, food additives, amalgam, or toothpaste components are possible pathogenesis factors. Disorders at the immunological level also play a role (up to 60% of patients are atopic),” says Dr. Kamarachev.
Melkersson-Rosenthal syndrome: The first manifestation is lymphedema in 75% of cases in the course of cheilitis granulomatosa. In about one third of cases, peripheral facial nerve palsy is also found, which is more common on the side of the swelling and may precede the edema by a long time (especially in children). A lingua plicata is observed about as frequently. However, this is not disease-specific.
Therapeutically, possible triggers must first be eliminated. In addition, corticosteroids (topical, intralesional, systemic), agents for immunomodulation (e.g., clofazimine, azathioprine) and surgical measures (e.g., lip reduction plasty) are used.
HPV – Oncogenic risk should not be underestimated
In conclusion, Dr. Kamarachev urged that the widespread use of HPV vaccination in the future must also be promoted in boys. “A large-scale study [2] has shown that one in ten sexually mature U.S. adults is orally infected with human papillomavirus (HPV). The prevalence is significantly higher in men than in women, including oncogenic HPV-16 (1% of adults). Because infection with HPV-16 increases the risk of HPV-16-associated oropharyngeal squamous cell carcinoma (OSCC) by a factor of 50, I, in agreement with many other experts, advocate vaccination of both sexes to effectively combat this viral infection,” Dr. Kamarachev concluded.
Therapeutic treasure chest
Alexander Navarini, MD, from the University Hospital Zurich, opened his “therapeutic treasure chest” after several case presentations, i.e. improved treatment methods, sometimes in the area of rhagades. If they appear on the soles of the feet, baths and exfoliation work. “Closed footwear is also important, because, for example, in sandals the foot really swells out over the edges of the sole, creating even more traction. Also preferable would be soft ground, which of course you can hardly influence.” In addition to pasta cerata and silver nitrate, there is an agent that has been available in principle for a long time and is now being used increasingly: The acrylate adhesive (e.g., wound adhesive Epiglu®). According to Dr. Navarini, this is a simple way to achieve very good results.
Botulinum toxin, on the other hand, seems to offer effective help in dyshidrosiform eczema [3] and Raynaud’s syndrome [4]. “Raynaud’s syndrome and ischemic fingers were first treated with Botox in 2004. The injection results in immediate improvement of pain and blood flow. However, the mechanism of action is unclear,” Dr. Navarini said.
Finally, he presented the clinical case of a 50-year-old female therapist who suffered from chronic persistent hand eczema (most likely cumulative-toxic) for three years: “Therapeutically, we tried everything from topical and systemic steroids, tar, acitretin to PUVA to methotrexate. Only treatment with alitretinoin 30 mg/tgl. brought any appreciable success.” A randomized, double-blind, controlled trial [5] showed significantly greater response than to placebo at both 30 mg and 10 mg doses for 12-24 weeks. This was defined as almost or completely free palms. On alitretinoin, up to 48% of patients responded, compared with 17% on placebo (p<0.001). At the same time the hands were re-greased. Topical steroids were not used. Among the side effects, the main ones are headache and hyperlipidemia. In the same study, recurrence (75% of original symptoms) was found after five to six months. However, another study showed that a renewed response is achievable in a vast majority of patients [6].
Diseases of the female genitals
The symptomatology and therapy of some genital conditions were presented by Dr. med. Katrin Kerl and Dr med. Cornelia Betschart from the University Hospital Zurich:
Genital psoriasis: The scaling typical of psoriasis is often absent in genital manifestations. Fissures appear for this purpose. About 40% of women with psoriasis complain of vulvar symptoms. However, genital infestation is detectable in only about 20%.
Therapy is anything but simple or uniform: local potent steroids and calcineurin inhibitors such as tacrolimus and pimecrolimus are used. Calcipotriol and betamethasone (Daivobet®) and in severe cases systemic therapy or anti-TNF biologics should also be considered.
Provoked local vulvodynia (formerly vestibulitis syndrome): Vulvodynia is defined by vulvar pain without a clinically relevant skin lesion or neurologic disease. It is associated with interstitial cystitis, stress, and anxiety, although not with sexual abuse. It often begins after antifungal therapy. The patch test is often negative.
Here, too, therapy is complex: empathy and an accurate explanation of the diagnosis are central. Topical applications should be omitted. Lidocaine 5% gel and also lubricants for sexual intercourse (KY gel, Replens, Pjur, Eros) help. Furthermore, tricyclic antidepressants and anticonvulsants may be considered, as well as cognitive therapy, behavioral therapy, and sex therapy. A study on the off-label use of Botox is currently being conducted at the USZ.
Lichen sclerosus: Occurs anogenitally in 85-98% of cases. There are two peaks in age: in prepubertal girls and perimenopausal women.
Treatment is with potent topical corticosteroids (Dermovate®) in an interval therapy or also intralesional steroids. Lubricating gel is used, as are clacineurin antagonists [7]. In cases of treatment failure or squamous cell carcinoma, vulvectomy should be considered.
Source: 4th Zurich Dermatology Training Days, June 25-28, 2014, Zurich.
Literature:
- Thyssen JP, et al: The outcome of dimethylglyoxime testing in a sample of cell phones in Denmark. Contact Dermatitis 2008 Jul; 59(1): 38-42.
- Gillison ML, et al: Prevalence of oral HPV infection in the United States, 2009-2010. JAMA 2012 Feb 15; 307(7): 693-703.
- Wollina U, Karamfilov T: Adjuvant botulinum toxin A in dyshidrotic hand eczema: a controlled prospective pilot study with left-right comparison. J Eur Acad Dermatol Venereol 2002 Jan; 16(1): 40-42.
- Neumeister MW: Botulinum toxin type A in the treatment of Raynaud’s phenomenon. J Hand Surg Am 2010 Dec; 35(12): 2085-2092.
- Ruzicka T, et al: Efficacy and safety of oral alitretinoin (9-cis retinoic acid) in patients with severe chronic hand eczema refractory to topical corticosteroids: results of a randomized, double-blind, placebo-controlled, multicentre trial. Br J Dermatol 2008 Apr; 158(4): 808-817.
- Bissonnette R, et al: Successful retreatment with alitretinoin in patients with relapsed chronic hand eczema. Br J Dermatol 2010 Feb 1; 162(2): 420-426.
- Goldstein AT, et al: A double-blind, randomized controlled trial of clobetasol versus pimecrolimus in patients with vulvar lichen sclerosus. J Am Acad Dermatol 2011 Jun; 64(6): e99-104.
DERMATOLOGIE PRAXIS 2014; 24(4): 32-33











