In one of this year’s issues of the American Journal of Kidney Diseases, the official publication of the National Kidney Foundation, an article on magnesium metabolism disorders has been published. Among other things, the pathogenesis, diagnosis and treatment of hypomagnesemia will be discussed. Hypomagnesemia can be caused primarily by congenital genetic mutations or occur secondarily as a result of other underlying diseases.
Magnesium regulates a variety of biochemical and cellular functions, as it acts as a cofactor of over 600 enzymes [1]. Magnesium (Mg++) is involved in stimulus transmission, muscle contraction, heart rhythm, vascular tone, blood pressure and bone turnover due to its membrane and electrolyte regulating properties. An inadequate magnesium supply is associated with an increased risk of numerous diseases (e.g. metabolic syndrome, type 2 diabetes, cardiovascular diseases) [2]. Magnesium deficiency often occurs as a comorbidity and can contribute to the exacerbation of diseases.
Risk groups for magnesium deficiency
Deficiency symptoms can develop secondarily as a result of impaired intestinal magnesium absorption or increased renal magnesium excretion [1]. Possible causes are gastrointestinal disorders such as acute or chronic diarrhea, vomiting, malabsorption or small bowel resection/bypass. A magnesium deficiency can also occur as a result of kidney disease, chronic alcohol consumption or long-term use of certain medications (including diuretics, antibiotics, oral contraceptives). Renal transplant recipients and patients with diabetes mellitus, including those with diabetic nephropathy, often have decreased plasma/serum Mg++ concentrations, which can accelerate the progression of renal involvement [3]. In addition, there are various hereditary diseases (e.g. Gitelman syndrome, Bartter syndrome) that predispose to hypomagnesemia. Other risk groups for magnesium deficiency are people with anorexia nervosa, cancer patients and people with heart disease [3,4]. Furthermore, the consumption of caffeine and alcohol can increase magnesium excretion via the kidneys. And it is being discussed whether sporting activity leads to increased magnesium losses via sweat or urine [1].
How can you recognize a magnesium deficiency?
It is recommended to routinely perform a Mg++ determination in the plasma of potential, even asymptomatic patients at risk [3,4]. With regard to the amount of magnesium in the blood serum (“serum magnesium”) determined by laboratory chemistry, 0.77-1.03 mmol/l is given as the reference value for women and 0.73-1.06 mmol/l for men. In children, the corresponding values are 0.60-0.95 mmol/l and 0.48-1.05 mmol/l for newborns [5]. Patients with mild hypomagnesemia are often asymptomatic [4]. Symptoms of magnesium deficiency only appear at very low serum concentrations of less than 0.5 mmol/l [6]. The first signs can be loss of appetite, nausea, vomiting, tiredness and general weakness. Neurological and cardiovascular symptoms (e.g. numbness, tingling, muscle cramps, sudden behavioral changes and cardiac arrhythmia) may occur as the disease progresses [1]. By impairing the release of PTH (parathyroid hormone) and contributing to end-organ resistance to PTH, hypomagnesemia can lead to hypocalcemia [4]. In addition, hypomagnesemia leads to renal potassium loss, which is probably due to an intracellular blockade of the ROMK (renal outer medullary potassium) channel and can result in hypokalemia.
Tips for the diagnostic work-up
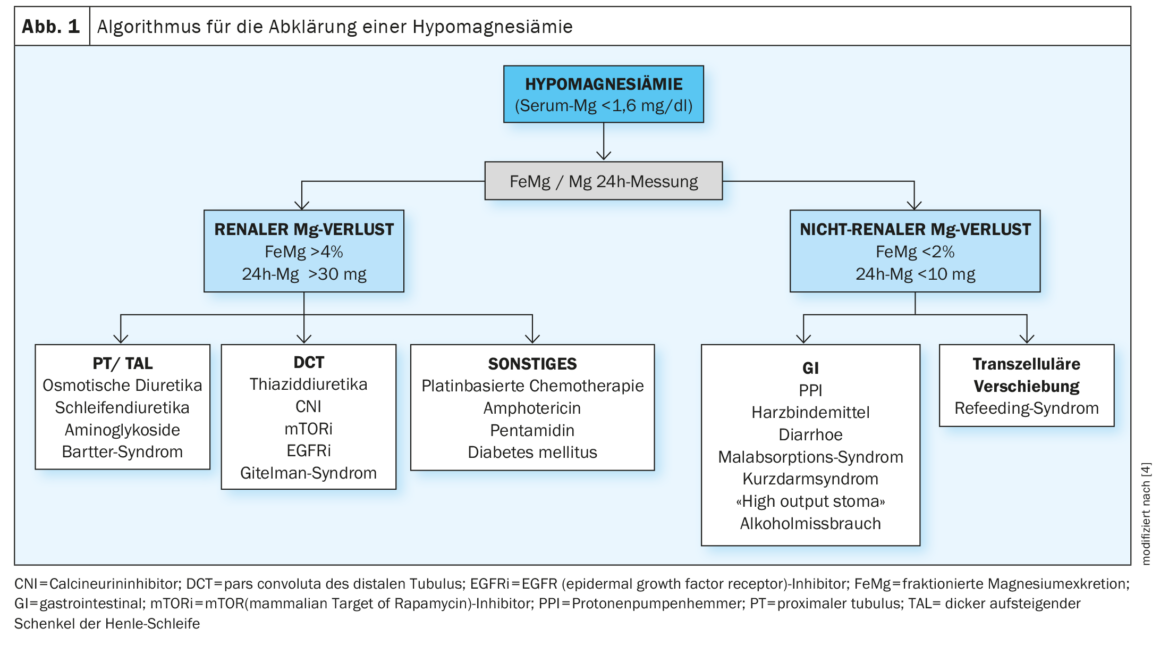
The diagnosis of Mg++ deficiency consists of the pillars of deficiency symptoms, laboratory diagnostics and risk factors [2]. In the article entitled “Magnesium Disorders: Core Curriculum 2024” published in the American Journal of Kidney Diseases by Adomako & Yu, it is recommended that if hypomagnesemia is detected, it should be clarified whether it is due to a renal or extrarenal cause (Fig. 1) [4]. In order to detect any other electrolyte disorders, the laboratory test should also include creatinine, potassium, calcium, phosphorus and PTH. Most renal Mg++ deficiencies are due to primary or secondary tubuloepithelial transport disorders, preferentially in the ascending thick part of the loop of Henle and the subsequent distal nephron segment. This is the case, for example, in Gitelman syndrome and Bartter syndrome, renal tubular acidosis and tubular disorders following acute renal failure [3]. Since almost a third of the magnesium in the blood is bound to plasma protein, hypoproteinemia (e.g. hypoalbuminemia) can cause low magnesium levels without the biologically active magnesium being reduced [7]. The following formula corrected for the albumin concentration is therefore proposed for calculating the magnesium concentration [6,7]: Corrected Mg++ [mmol/l] = 0.102 + 0.58 × serum Mg++ [mmol/l] – 0.001 × albumin [g/l].
Mg++ substitution is carried out by means of oral or intravenous preparations.
Literature:
- Deutsche Gesellschaft für Ernährung, www.dge.de/gesunde-ernaehrung/faq/ausgewaehlte-fragen-und-antworten-zu-magnesium/#c3594, (last accessed 13.06.2024).
- Micke O, et al.: Magnesium: Bedeutung für die hausärztliche Praxis – Positionspapier der Gesellschaft für Magnesium-Forschung e. V [Magnesium: Relevance for general practitioners – a position paper of the Society for Magnesium Research e. V.]. Dtsch Med Wochenschr 2020; 145(22): 1628–1634.
- S2k-Leitlinie Rationelle Labordiagnostik zur Abklärung Akuter Nierenschädigungen und Progredienter Nierenerkrankungen; Stand: 19.04.2021, gültig bis: 18.04.2026.
- Adomako EA, Yu ASL: Magnesium Disorders: Core Curriculum 2024. Am J Kidney Dis 2024; 83(6): 803–815.
- Flexikon: Serum magnesium, https://flexikon.doccheck.com,(last accessed 13.06.2024).
- Basten MI: Dissertation: Beobachtungsstudie zur Bedeutung des ionisierten Magnesiums bei chronischer Niereninsuffizienz [Dissertation/PhD Thesis]. Aachen: Rheinisch-Westfälische Technische Hochschule Aachen 2018. https://publications.rwth-aachen.de/record/749745, (letzter Abruf 13.06.2024)
- Flexikon: Hypomagnesemia, https://flexikon.doccheck.com,(last accessed 13.06.2024).
HAUSARZT PRAXIS 2024; 19(6): 32–33