Accurate staging of cancer patients is essential to initiate appropriate treatment. Bone is a frequent site of metastasis for many tumors, mainly breast, prostate and lung carcinomas, followed by renal cell and thyroid carcinomas. Bone metastasis can be diagnosed by several nuclear medicine modalities, such as bone scintigraphy, 18F-FDG PET-CT or more tumor-specific modalities, such as iodine scintigraphy for thyroid cancer. Depending on the tumor type and the bone lesion characteristics (lytic, sclerotic or mixed), one modality may be preferred over another. 18F-FDG PET/CT is the preferred modality for the detection of bone metastasis in patients with 18F-FDG avid tumors, such as breast or lung cancer. Bone scintigraphy is still the preferred modality in nuclear medicine for the detection of osteoblastic bone metastasis in patients with prostate cancer. 18F-FDG PET/CT is not recommended in renal cell carcinoma as the tumor is mostly not FDG avid. New modalities such as 18F-NaF PET/CT might play an important role for these tumors in the future. 18F-FDG PET/CT and iodine scintigraphy are both useful in staging of thyroid carcinoma.
Accurate initial staging of cancer patients is essential in order to initiate the appropriate treatment. Bone is the third most common site of metastasis after lung and liver [1]. The most common malignancies that spread to the bone are breast in women and prostate in men, followed by lung [2]. Thyroid and renal cancer are also likely to spread to bone. Metastasis to the bone commonly occurs in the spine (predominantly in the lumbar spine), pelvis, ribs, skull, proximal femur, and proximal humerus [1,3]. Indeed, these sites are well vascularized and are constantly undergoing remodeling. During remodeling many substances are produced, such as chemokines and cytokines. These can interact with metastatic cells, allowing them to grow. In turn, metastatic cells can produce substances that stimulate osteoclasts or osteoblasts, leading to lytic or sclerotic bone lesions respectively [4].
Nuclear Medicine Modalities
Bone metastasis can be diagnosed by several modalities in nuclear medicine. Depending on the tumor type and the bone lesion characteristics (mainly lytic, sclerotic or mixed), one modality may be preferred over another.
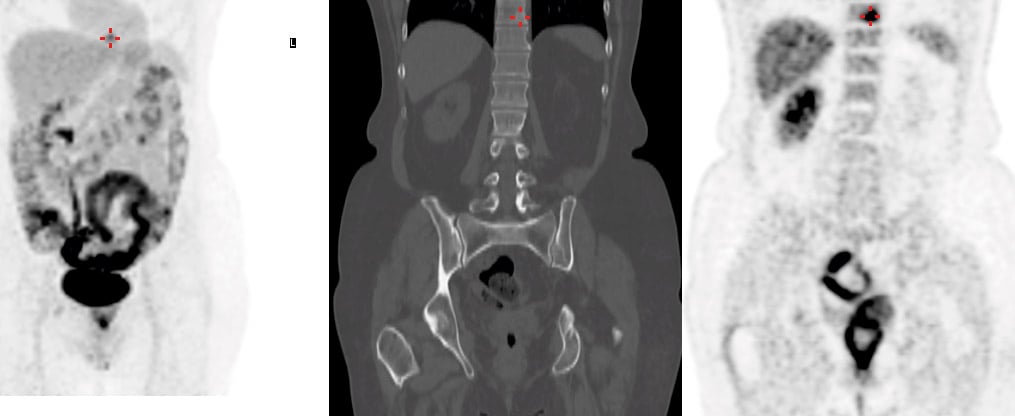
Bone scintigraphy is the most widely available modality for the detection of bone metastasis. Radiolabeled diphosphonates are absorbed by the hydroxyapatite crystals in the remodeling bone. 99mTc-labelled diphosphonate uptake depends not only on osteoblastic activity, but also on vascularity and environmental factors influencing extraction efficiency. Bone scintigraphy has a high sensitivity for osteoblastic lesions, but a low specificity, as benign conditions such as degenerative disease also have an increased bone turnover and may mimic metastasis on the scan. Combining the functional information given by a three dimensional acquisition called SPECT (Single Photon Emission Computed Tomography) with the morphologic information acquired by CT (Computed Tomography) in the same session, greatly improves specificity [5] (Fig. 1). Of note, lytic lesions without osteoblastic component can be missed on bone scintigraphy, leading to false negatives.
The second modality for the detection of bone metastasis is 18F- sodium fluoride positron emission tomography, combined with computed tomography (18F- NaF PET/CT). Like with diphosphonates, fluoride accumulates in the remodeling bone, binding to hydroxyapatite. Therefore, 18F- NaF PET/CT enables the detection of bone metastasis, with a better spatial resolution and an increased sensitivity compared to bone scintigraphy [1]. It has not yet replaced bone scintigraphy as it is still more expensive and less widely available. This tracer has less radiation burden than 99mTc-labelled diphosphonates, which can be of interest in the treatment of children.
18F-Fluorodeoxyglucose (FDG) PET/CT is routinely used in the staging of different malignancies, and has an important role in the detection of bone metastasis. FDG is a glucose analogue, which is absorbed by metabolically active cells such as tumor cells. The efficiency of FDG uptake by tumor cells depends on the tumor type. However, uptake of FDG is not specific to cancer cells. Other cells, such as brain or inflammatory cells, are also metabolically active.
There are several tracers used in nuclear medicine that are used to specifically detect certain tumors. One of them is radioiodine, which is used to detect metastasis of differentiated thyroid cancer (DTC). Radiolabelled somatostatine analogues (111In-octreotide scintigraphy or 68Ga-DOTATATE PET) are tracers that can be used to detect metastasis of neuroendocrine tumors. Finally, scintigraphy using 123I-radiolabeled metaiodobenzylguanidine (mIBG) as tracer, allows the detection of metastasis of tumors of the neuroectodermal system (pheochromocytoma, neuroblastoma, and paragangliomas).
All these modalities allow a diversity of methods, which can each specifically target certain types of tumors. The modality chosen to detect bone metastasis is therefore highly dependent on the tumor type. We will focus on the most common malignancies spreading to bone: breast, prostate, lung, thyroid, and renal cell carcinoma.
Breast Cancer
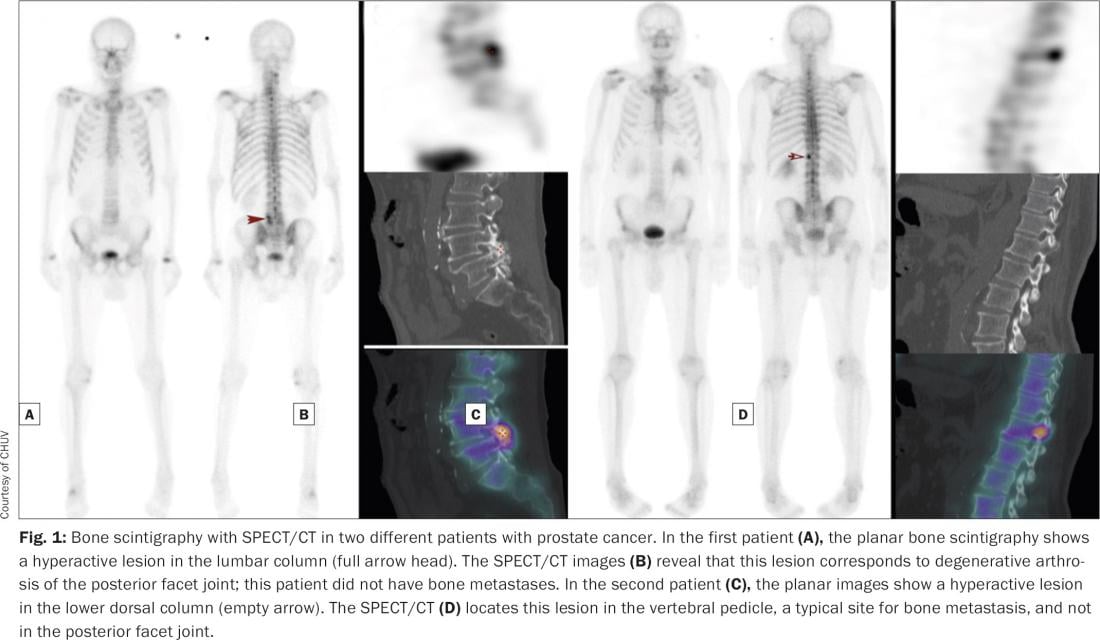
Bone metastasis is the most common site of metastasis in breast cancer patients. Bone lesions in breast cancer patients are mostly mixed sclerotic and lytic lesions. Chest radiography, abdominal ultrasonography, and bone scintigraphy are widely used as first intention to diagnose distant metastasis in breast cancer patients. This conventional imaging has been progressively replaced by 18F-FDG PET/CT in patients with advanced breast cancer, as 18F-FDG PET/CT tends to have a higher sensitivity and accuracy than bone scintigraphy for the detection of bone metastasis in breast cancer patients [6,7] (Fig. 2). Guidelines recommend 18F-FDG PET/CT for staging of newly diagnosed stage III breast cancer patients, as the incidence of distant metastasis is low in stage I and II disease. However, factors other than stage may influence PET/CT utility, such as young age or a triple negative histology. Indeed, PET/CT has been seen to be useful in patients presenting with these factors [8,9].
Prostate Cancer
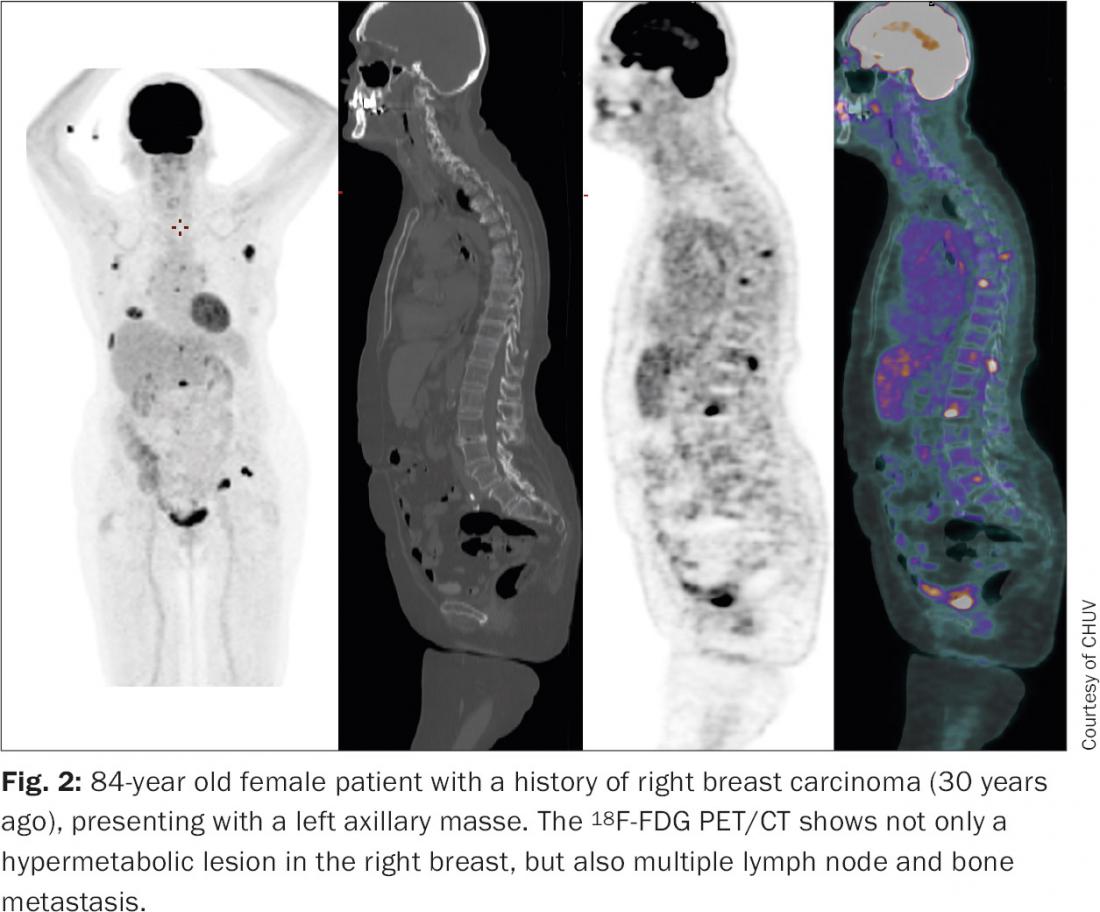
Prostate cancer is the most common cancer in men and bone metastasis is the first site of distant metastasis in these patients. Metastatic bone lesions of prostate cancer are predominantly osteoblastic, and therefore bone scintigraphy has a high sensitivity for their detection and is widely used for staging (Fig. 3). Bone metastasis have been found on bone scans in 2,3–5,3% of patients with a PSA level of <20 ng/ml, in 5,6% of patients with a Gleason Score ≤7, and in 30% of patients with a Gleason score of >8 [3]. Therefore, there is controversy at which cutoff of PSA level a bone scintigraphy should be done: some guidelines recommend a bone scintigraphy when the PSA level is above 20 ng/ml and/or the Gleason score is 8 or above, and others recommend a cutoff level of PSA above 10 ng/ml, or whenever radical treatment is planned [10].
18F-NaF PET has a higher resolution and is more sensitive than a bone scan, but it is less widely available and not yet covered by health insurance in Switzerland. 18F-NaF PET has a high overall impact on change of management in prostate cancer patients [11]. 18F-FDG uptake is low in differentiated prostate cancer lesions and its sensitivity in detecting bone metastasis is low. It is therefore not recommended in initial staging, although it might play a prognostic role in metastatic prostate cancer, since higher uptake values of FGD serve as an indicator of poor prognosis [12]. Choline kinase is upregulated in prostate cancer cells, leading to an increase in choline uptake by these cells. PET/CT with radiolabeled choline can be used to detect local recurrences and distant metastasis in patients with biochemical failure, allowing prompt initiation of appropriate treatment [13].
Lung Cancer
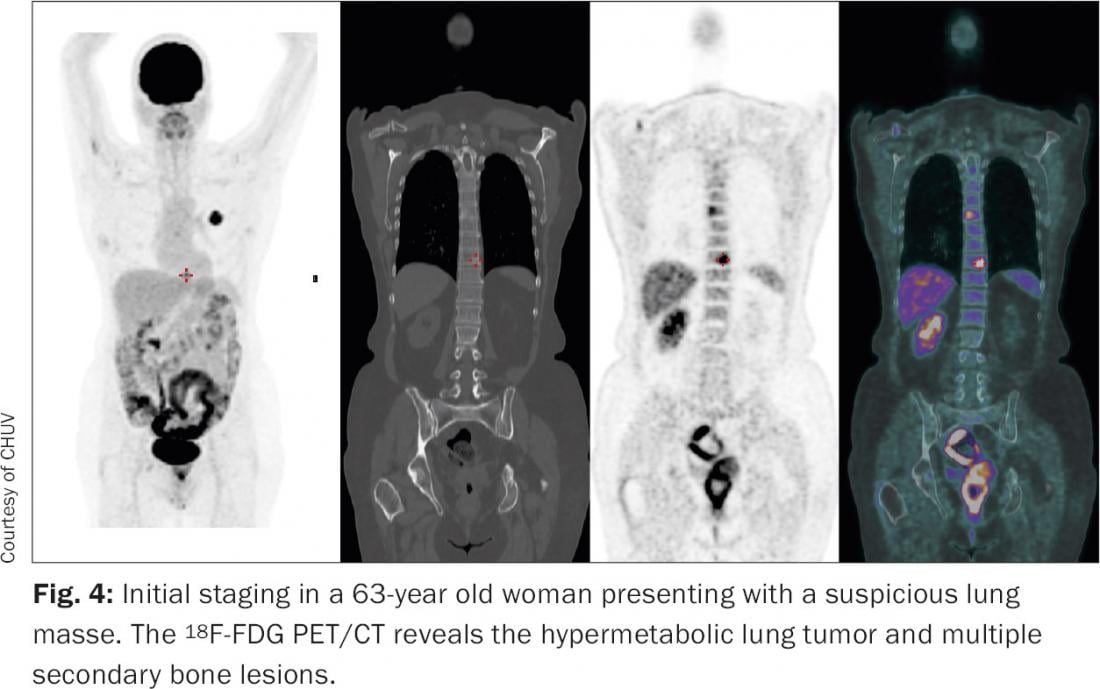
Lung cancer is the second most common tumor in developed countries. It is the leading cause of
cancer death in men and the second most common cause of cancer death in women. As many as 20 to 30% of patients with advanced lung cancer have bone metastasis at diagnosis. Patients with bone metastasis are no longer candidates for curative surgery, thus the importance of accurate staging. Bone scintigraphy has been widely used to detect lung cancer bone metastases, but seems less sensitive than 18F-FDG PET/CT [14,15]. This is in part due to the nature of bone metastases: it can be purely lytic in lung cancer and therefore remain undetected with bone scintigraphy. Since 18F-FDG PET/CT can also detect distant metastasis other than bone, it has become the standard imaging modality for lung cancer staging (Fig. 4).
Thyroid Cancer
The most common sites of distant metastasis in differentiated thyroid cancer (DTC) patients are lung and bone. After thyroidectomy, many patients undergo thyroid remnant ablation or adjuvant therapy with radioiodine, namely 131I. 131I-whole body scans are obtained after therapy and allow visualization of iodine avid tissues, such as remnant thyroid tissue, locoregional metastasis, and distant metastasis (Fig. 5). Sites of abnormal iodine uptake seen on a whole-body 131I scan can be further localized with a SPECT/CT. Because of dedifferentiation, about 20–50% of metastatic DTC cases have no ability to take up iodine. These dedifferentiated lesions tend to be FDG avid and therefore 18F-FDG PET/CT plays an important role in these patients, who present with elevated thyroglobulin levels and a negative 131I whole body scan. Qui et al. [16] showed that both iodine whole-body scans associated with SPECT/CT and 18F-FDG PET/CT have a high diagnostic value in detecting DTC bonemetastasis after the first 131I therapy, and that most patients (34/43 or 79%) had concordant findings with regard to bone metastasis in both exams. The possible reason could be that bone metastasis exhibited diverse differentiation in different parts of the same lesion [16]. The combination of the two examination modalities revealed all bone lesions. The authors also showed that a positive 18F-FDG PET was associated with a poorer prognosis in DTC patients with bone metastasis.
Renal Cell Carcinoma
The most common sites of metastasis in renal cell carcinoma patients are lung and bone. Bone metastasis of renal cell carcinoma (RRC) are predominantly lytic and therefore the sensitivity of bone scans is moderate and underestimates the extent of the disease.
18F-FDG PET may improve both sensitivity and accuracy of the diagnosis, but it still has a high rate of false negative results (up to 30%) [17]. Therefore, multi-detector computed tomography (MDCT) remains the primary modality for staging of RCC. Recently, Gerety et al. have shown that 18F-NaF PET/CT is significantly more sensitive than bone scintigraphy or CT for the detection of bone metastasis [18,19], and might play a role in the future for staging of RCC. 18F-FDG PET/CT might be of clinical value in patients with suspected recurrent RCC [20].
Conclusion
Nuclear medicine plays a key role in the detection of bone metastasis. The choice of modality depends not only on the onsite availability, but also on the nature of the metastatic bone lesion. Bone scintigraphy is most sensitive for osteoblastic lesions, such as prostate bone metastasis, but it may oversee pure osteolytic lesions. The sensitivity and specificity of planar bone scintigraphy has been improved by the addition of SPECT/CT. 18F-NaF PET/CT is a promising modality that is believed to be more sensitive than bone scintigraphy, but it is not yet widely available. 18F-FDG PET/CT is a valuable modality in primary staging of numerous FDG avid cancers, such as lung cancer and advanced breast cancer, and it allows for early detection of bone and other distant metastasis. 18F-FDG PET/CT is not recommended in routine staging in prostate and RCC patients, as these tumors are not commonly FDG avid. Finally, some specific radiotracers may detect bone metastasis of particular tumors. 131I scintigraphy, for example, can detect the iodine avid bone metastasis of DTC.
References:
- O’Sullivan GJ, Carty FL, and Cronin CG: Imaging of bone metastasis: An update. World J Radiol 2015; 7(8): 202–211.
- Piccioli A, et al.: Bone metastases of unknown origin: epidemiology and principles of management. J Orthop Traumatol 2015; 16(2): 81–86.
- Davila D, Antoniou A, and Chaudhry MA: Evaluation of osseous metastasis in bone scintigraphy. Semin Nucl Med 2015; 45(1): 3–15.
- Bussard KM, Gay CV, and Mastro AM: The bone microenvironment in metastasis; what is special about bone? Cancer Metastasis Rev 2008; 27(1): 41–55.
- Saha S, et al.: SPECT-CT: applications in musculoskeletal radiology. Br J Radiol 2013; 86(1031):20120519. doi: 10.1259/bjr.20120519. [Epub 2013 Oct 4]
- Rong J, et al.: Comparison of 18 FDG PET-CT and bone scintigraphy for detection of bone metastases in breast cancer patients. A meta-analysis. Surg Oncol 2013; 22(2): 86–91.
- Hong S, Li J, and Wang S: 18 FDG PET-CT for diagnosis of distant metastases in breast cancer patients. A meta-analysis. Surg Oncol 2013; 22(2): 139–143.
- Riedl CC, et al.: Retrospective analysis of 18F-FDG PET/CT for staging asymptomatic breast cancer patients younger than 40 years. J Nucl Med 2014; 55(10): 1578–1583.
- Ulaner GA, et al.: 18F-FDG-PET/CT for systemic staging of newly diagnosed triple-negative breast cancer. Eur J Nucl Med Mol Imaging 2016, Apr 30. [Epub ahead of print]
- Rajarubendra N, Bolton D, and Lawrentschuk N: Diagnosis of bone metastases in urological malignancies – an update. Urology 2010; 76(4): 782–790.
- Hillner BE, et al.: Impact of 18F-fluoride PET in patients with known prostate cancer: initial results from the National Oncologic PET Registry. J Nucl Med 2014; 55(4): 574–581.
- Beauregard JM, Pouliot F: New developments in the imaging of metastatic prostate cancer. Curr Opin Support Palliat Care 2014; 8(3): 265–270.
- Goldstein J, et al.: Does Choline PET/CT Change the Management of Prostate Cancer Patients With Biochemical Failure? Am J Clin Oncol 2014, Nov 4. [Epub ahead of print]
- Chang MC, et al.: Meta-analysis: comparison of F-18 fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastasis in patients with lung cancer. Acad Radiol 2012; 19(3): 349–357.
- Damle NA, et al.: The role of 18F-fluoride PET-CT in the detection of bone metastases in patients with breast, lung and prostate carcinoma: a comparison with FDG PET/CT and 99mTc-MDP bone scan. Jpn J Radiol 2013; 31(4): 262–269.
- Qiu ZL, et al.: Comparison of the diagnostic and prognostic values of 99mTc-MDP-planar bone scintigraphy, 131I-SPECT/CT and 18F-FDG-PET/CT for the detection of bone metastases from differentiated thyroid cancer. Nucl Med Commun 2012; 33(12): 1232–1242.
- Mueller-Lisse UG, et al.: Imaging of advanced renal cell carcinoma. World J Urol 2010; 28(3): 253–261.
- Fuccio C, et al.: 18F-Fluoride PET/CT in the detection of bone metastases in clear cell renal cell carcinoma: discordance with bone scintigraphy. Eur J Nucl Med Mol Imaging 2013; 40(12): 1930–1931.
- Gerety EL, et al.: Prospective study evaluating the relative sensitivity of 18F-NaF PET/CT for detecting skeletal metastases from renal cell carcinoma in comparison to multidetector CT and 99mTc-MDP bone scintigraphy, using an adaptive trial design. Ann Oncol 2015; 26(10): 2113-2118.
- Nakatani K, et al.: The potential clinical value of FDG-PET for recurrent renal cell carcinoma. Eur J Radiol 2011; 79(1): 29–35.
InFo ONKOLOGIE & HÄMATOLOGIE 2016; 4(6): 6-9