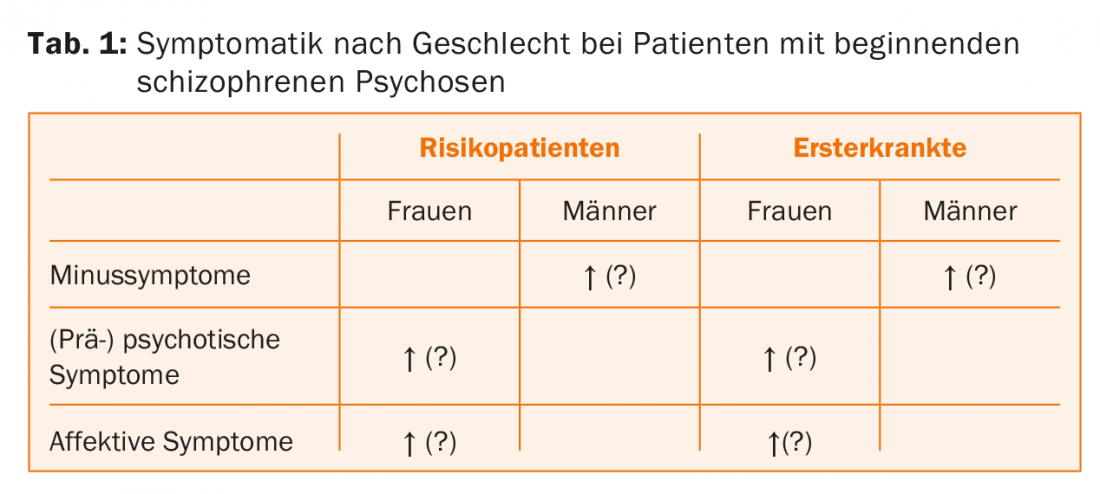
Patients with onset psychosis show only minor, if any, sex differences in symptomatology. Some studies found more pronounced minus symptoms in men, while women more often had affective and psychotic symptoms. Overall, the picture is mixed.
Sex differences in schizophrenic psychosis have been described in the literature for some time [1,2]. One of the best documented findings is an earlier onset of disease in men. In addition, women appear to have a more favorable disease course than men, although this is strongly dependent on psychosocial and cultural factors. Similarly, substance abuse is less common among women. The incidence is sometimes described as slightly higher in men than in women [3], but when the cumulative lifetime risk is considered, it appears almost identical for both sexes [4]. This is due to the fact that while men are more likely to develop the disease at a young age, women have a higher rate of initial manifestations after the menopause.
It should be noted that the epidemiologic characteristics of a disease can provide important clues in elucidating the underlying etiology. Therefore, it also seems important to investigate sex differences already in patients with a first psychotic episode (FEP; “first episode psychosis”) or even earlier, in psychosis risk patients (ARMS; “at-risk mental state”). In the following, we will discuss sex differences in psychosis onset (patients with a first episode of psychosis and those at risk) in the three important topics of psychopathology, cognitive functioning, and endocrinology.
Sex differences in psychopathology
With regard to the symptomatology of first-episode psychosis patients, there is no uniform picture. Some studies found more pronounced minus symptoms in men, while women more often had affective and psychotic symptoms. On the other hand, there are also scientific studies that did not find any gender differences in symptoms [2]. A very similar, mixed picture emerges in psychosis risk patients [5]. In a separate study, we examined sex differences in first-episode psychosis and at-risk patients. We found a stronger expression of minus symptomatology in men and a stronger expression of (pre-)psychotic symptomatology and depressivity in women (Table 1) [6]. However, these differences were no longer significant when statistically corrected for multiple testing. Thus, the sex differences found were either due to random variation or were too small to be reliably detected with our medium-sized sample. Given that other studies had found sex differences that tended to go in exactly the same direction, the latter interpretation seems plausible to us. In summary, it can be said that gender differences in symptomatology are present at most to a minor extent and thus the clinical significance of these differences can also be classified as rather low.
Sex differences in cognitive functions.
Impairments in cognitive functioning are commonly recognized as a core feature of schizophrenia and may be observed as early as in patients with a first episode of psychotic illness or in individuals at risk for psychotic illness [7].
Consideration of such cognitive impairments may contribute to improved prediction of transition to psychosis (i.e., transition from risk status to full-blown psychosis). For example, in a study we conducted [8], it was shown that by including the test results of the neuropsychological examination, transition could be predicted better than on the basis of psychopathology alone. In the context of this, it is particularly important to also investigate differences in cognitive function between men and women, especially as these may provide important clues to underlying pathogenic mechanisms.
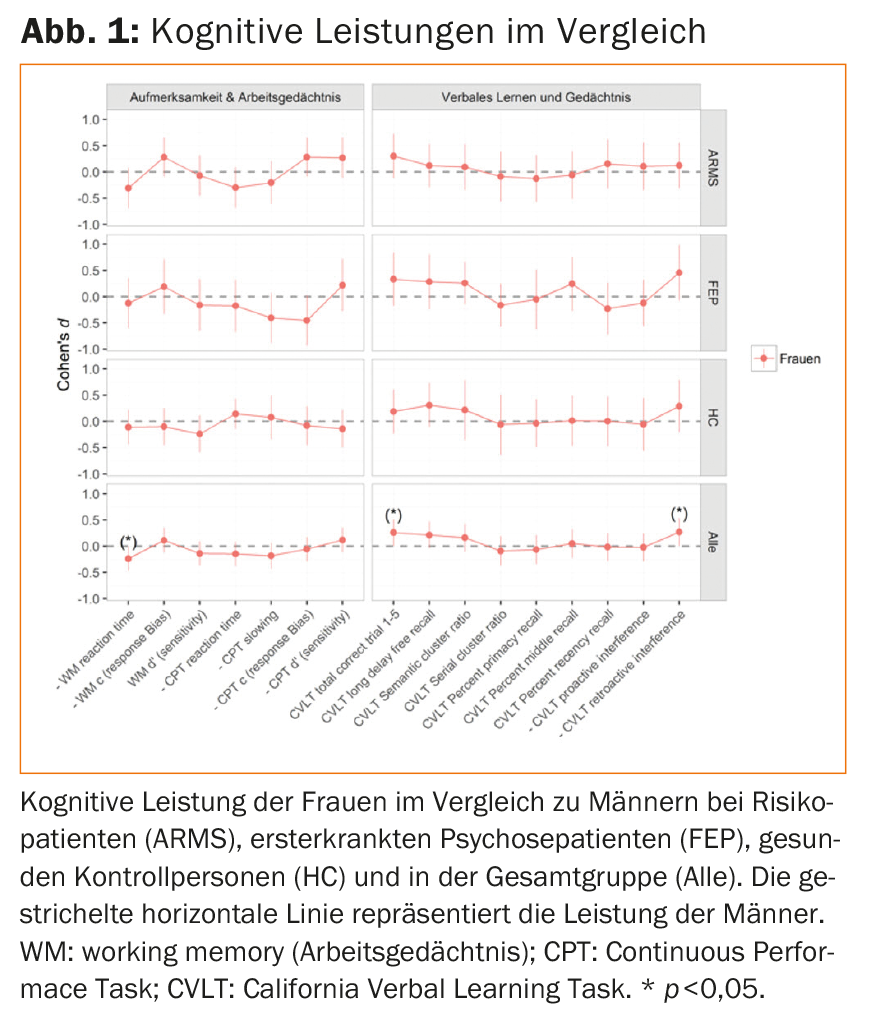
In healthy individuals, women on average have better verbal skills while men show better performance in visuospatial tasks. In first-episode psychosis patients, increased evidence can also be found for better performance of women in verbal learning and verbal memory [2]. There are no consistent findings in the areas of IQ, attention and working memory, and executive functions [2]. In patients at risk, there have been very few studies to date. In a separate study, we examined sex differences in cognitive functioning in high-risk patients, first-episode psychosis patients, and healthy controls [9]. Females in our study showed better performance in verbal learning and verbal memory, while males had a shorter reaction time in working memory with the same performance (Fig.1). These sex differences were similar in magnitude across groups, indicating that there is no change in sex differences in neurocognitioin with progression of psychotic illness and that the sex differences found in patients are similar to those found in healthy individuals.
Sex differences in endocrinology.
As mentioned above, post-menopausal women have a significantly increased risk of developing psychosis. As a possible explanatory model, the so-called estrogen hypothesis can be used, which assumes a protective effect of estrogens between puberty and menopause in women. According to this hypothesis, the drop in estrogen levels during (pre)menopause leads to reduced protection against schizophrenic psychosis [10].
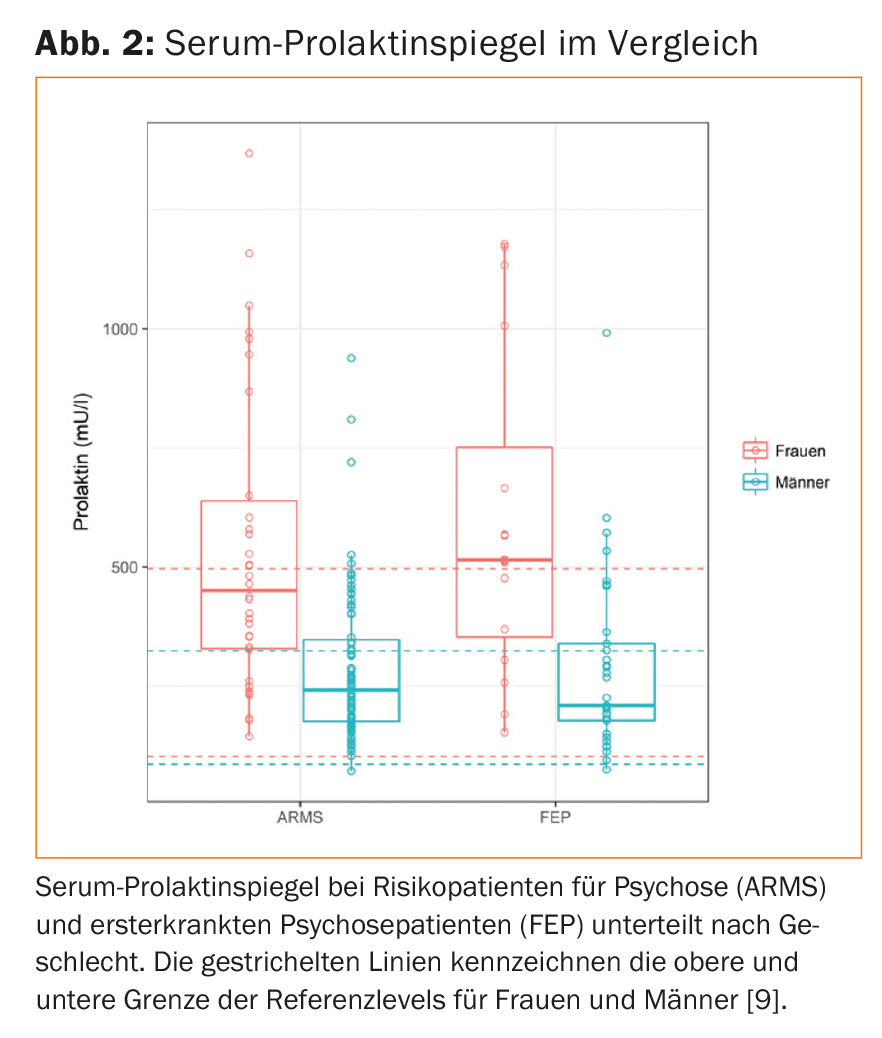
A study by our research group was also able to show that in both patients at risk for psychosis and first-time sufferers, around one third of antipsychotic-naïve patients had what is known as hyperprolactinemia. In both groups, women had an even greater increase in blood prolactin levels than men (fig. 2), which may possibly indicate increased stress sensitivity in women, since prolactin is also a stress hormone [11].
Conclusion
More attention should be paid to possible sex differences in psychosis onset. Even if these seem to be rather small in the field of psychopathology, in individual cases lack of drive and social withdrawal in men can conceal the first indications of an incipient psychosis, while in women a depressive mood should also make one alert. In addition, it is important to consider schizophrenic psychosis in patients in midlife as well, since onset of illness even after menopause is not uncommon, especially in women. For the practitioner, this means always being sensitive to the signs that may be reported differently by women and men.
Take-Home Messages
- Research on sex differences in psychosis onset can make a significant contribution to understanding the etiopathogenesis of these disorders.
- Patients with onset psychosis show little, if any, sex difference in symptomatology, with increased expression of minus symptoms most likely in males and increased expression of (pre)psychotic and depressive symptoms in females.
- In terms of cognition, similar to healthy controls, patients with onset psychosis are found to perform better in verbal learning and verbal memory in females.
- The stress hormone prolactin appears to be elevated more frequently in women with psychosis onset than in men, independent of antipsychotic medication, which may indicate increased stress sensitivity in women.
Literature:
- Riecher-Rössler A, Pflueger M, Borgwardt S: Schizophrenia in women. In: Kohen D (ed.) Oxford textbook of women and mental health. Oxford, Oxford University Press 2010; 102-115.
- Ochoa S, et al: Gender Differences in Schizophrenia and First-Episode Psychosis: A Comprehensive Literature Review. Schizophrenia Research and Treatment 2012; 2012: Article ID 916198: 9 pages.
- Häfner H, et al: Sex differences in schizophrenic disorders. Fortschr Neurol Psychiat 1991; 59: 343-360.
- Van der Werf M, et al: Systematic review and collaborative recalculation of 133693 incident cases of schizophrenia. Psychological Medicine 2014(44): 9-16
- Barajas A, et al: Gender Differences in Individuals at High-Risk of Psychosis: A Comprehensive Literature Review. The Sci World J 2015; 2015: Article ID 430735: 13 pages.
- González-Rodríguez A et al: Gender Differences in the Psychopathology of Emerging Psychosis. Isr J Psychiatry Relat Sci 2014; 51(2): 85-93.
- Bora E, Murray RM: Meta-analysis of Cognitive Deficits in Ultra-high Risk to Psychosis and First-Episode Psychosis. Schizophrenia Bull 2014; 40(4): 744-755.
- Riecher-Rössler A, et al: Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry 2009; 66(11): 1023-1030.
- Ittig S, et al: Sex differences in cognitive functioning in at-risk mental state for psychosis, first episode psychosis and healthy control subjects. Eur Psychiatry 2015; 30: 242-250.
- Riecher-Rössler A: Estrogens, prolactin, hypothalamic – pituitary – gonadal axis, and schizophrenic psychoses. Lancet Psychiatry 2017; 4(1): 63-72.
- Ittig S, et al: Sex differences in prolactin levels in emerging psychosis. Schizophr Res 2017; https://doi.org/10.1016/j.schres.2017.02.010
Additional literature can be requested from the authors.











