Sexual dysfunction is a “side show” of MS disease. Nevertheless, a considerable proportion of all those affected suffer from it. Not only MS itself, but also the comorbidity “depression” plays a role here.
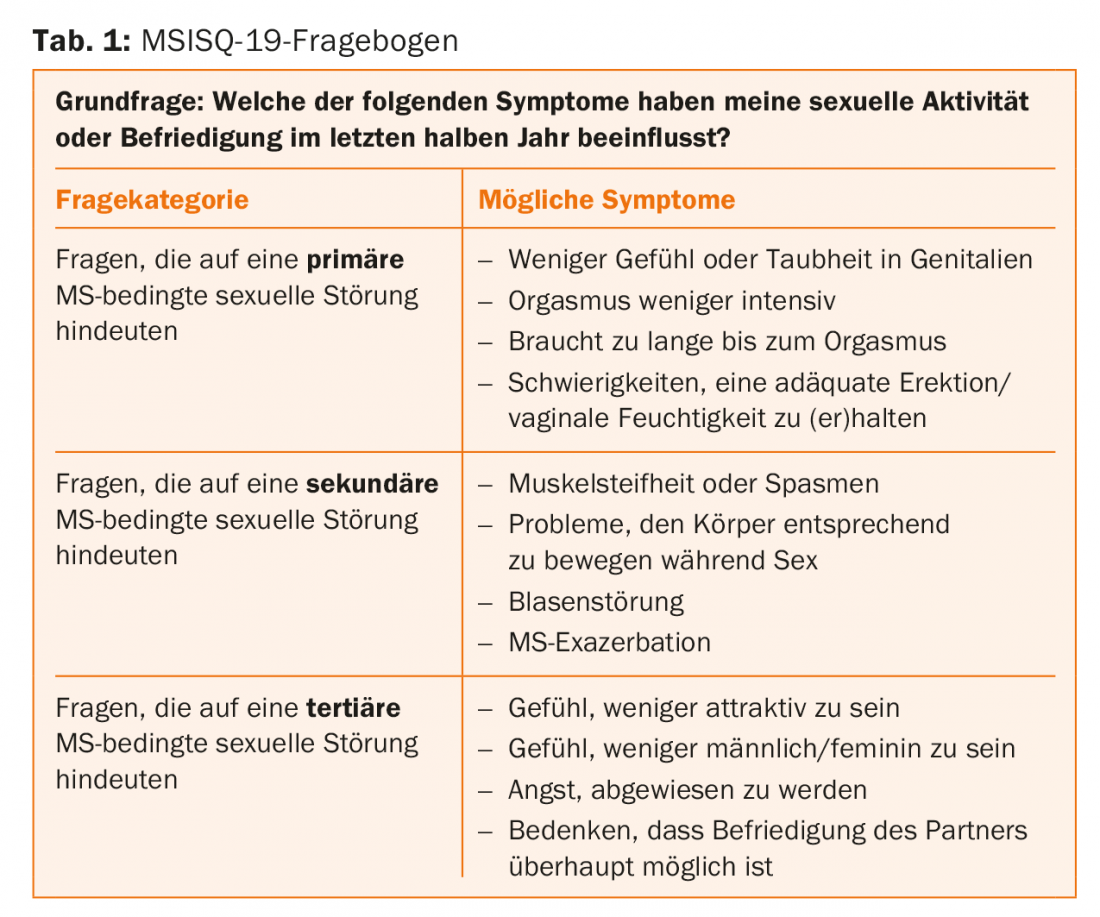
Sexual problems are not uncommon in multiple sclerosis patients. Researchers attribute them equally to neurological and psychological causes. Cerebral/spinal cord lesions, of course, come first. According to the authors of a paper presented at the congress, they are responsible for the so-called “primary sexual dysfunctions”. In addition, MS-associated physical disabilities such as bladder or bowel problems and induced psychological disturbances concerning self-image/self-esteem are considered to be the cause of “secondary” and “tertiary” sexual dysfunctions. (Tab.1). However, those affected not only suffer from these, but in up to half of all cases also from depression, which in turn has a sensitive effect on sexual activity.
Depression could be a consequence of the neuropathologic process of MS itself, but could just as easily be a response to the psychosocial stress associated with the diagnosis (or both). Although the relationship between MS and depressive disorders is highly complex and in many respects still unresolved, MS severity appears to influence both depression and sexual (dys)function.
Possible connections
The German-led study sought to examine more closely the associations between the three parameters of “MS,” “depression,” and “sexual dysfunction” using 83 female MS patients. Seventy-six had relapsing-remitting MS, six had secondary progressive MS, and one person had primary progressive MS. The median age was 36.2 years. Various questionnaires/scales were used as survey instruments and for endpoint analysis:
- Beck Depression Inventory-V (BDI-V) for the assessment of depression
- 19-item Female Sexual Function Index (FSFI) to assess sexual dysfunction.
- Multiple Sclerosis Intimacy and Sexuality Questionaire-19 (MSISQ-19) to classify sexual dysfunction in MS as “primary,” “secondary,” and “tertiary” (Table 1).
- Expanded Disability Status Scale (EDSS) to assess MS severity.
Examining the correlations of these scores with each other, the authors concluded that the BDI-V, depression, is inversely related to sexual function, i.e., the FSFI (for the latter, higher scores indicate better function, for the BDI-V, it is the other way around). The more severe the depression, the more unsatisfactory the sexual activity. Overall, depression was present in just over one-third of the women and sexual dysfunction in almost half (i.e., a score of ≤26.55 on the FSFI).
At the same time, the BDI-V correlated significantly with the MSISQ-19 score for “tertiary” MS-related sexual problems. This is fundamentally unsurprising: as depression becomes more likely, the possibility of psychological factors negatively affecting sexual intercourse increases. However, it also supports the validity of the MSISQ-19 questionnaire. Based on this, a possible depression-related sexual disorder can be concluded in a simple first diagnostic step.
The EDSS, in turn, correlated significantly with the MSISQ-19 score for “secondary” MS-related sexual problems, again a result that was to be expected: increasing disability severely limits sexual activity and satisfaction. Again, the key finding is that the MSISQ-19 scale can thus provide a first quick indication of the cause of the sexual problem.
Overall, 73.7% had “primary,” 84.2% (also) had “secondary,” and 57.9% (also) had “tertiary” sexual dysfunction according to MSISQ-19.
What next?
According to the authors, knowing whether the sexual dysfunction is primarily due to MS itself or depression is critical to defining next steps. Do you need to treat the depression or the MS (or the sexual dysfunction itself) to make sexual intercourse more attractive to the patient again? The study contributed an important finding to clarify this very question: While both causes may be equally responsible for the unsatisfactory sexual situation of many MS patients, the simple and quick-to-complete MSISQ-19 questionnaire provides a good initial insight into which of the two spheres dominates in the individual case. That depression reached significance in the domain of “tertiary” sexual disorders and disability in the domain of “secondary” ones illustrates the intrinsic value of both parameters as causes of sexual problems and the relevance of the MSISQ-19 questionnaire in the therapeutic decision-making process. Depending on the dominance of one or the other, antidepressants may or may not be useful. Treating sexual dysfunction that is not due to depression with antidepressants creates more problems and can worsen the situation.
Source: Congress of the European Academy of Neurology (EAN), June 24-27, 2017, Amsterdam.