For strokes caused by occlusion (thrombus) of the basilar artery in the posterior part of the brain, treatment recommendations have been based primarily on registry data. Now, almost simultaneously, two Chinese studies [1, 2] confirm that, in addition to standard treatment, affected individuals benefit significantly from removal of the thrombus by vascular catheter (endovascular thrombectomy), as is already an established procedure for occlusions of other large cerebral arteries. The 90-day mortality decreased and the functional outcome improved.
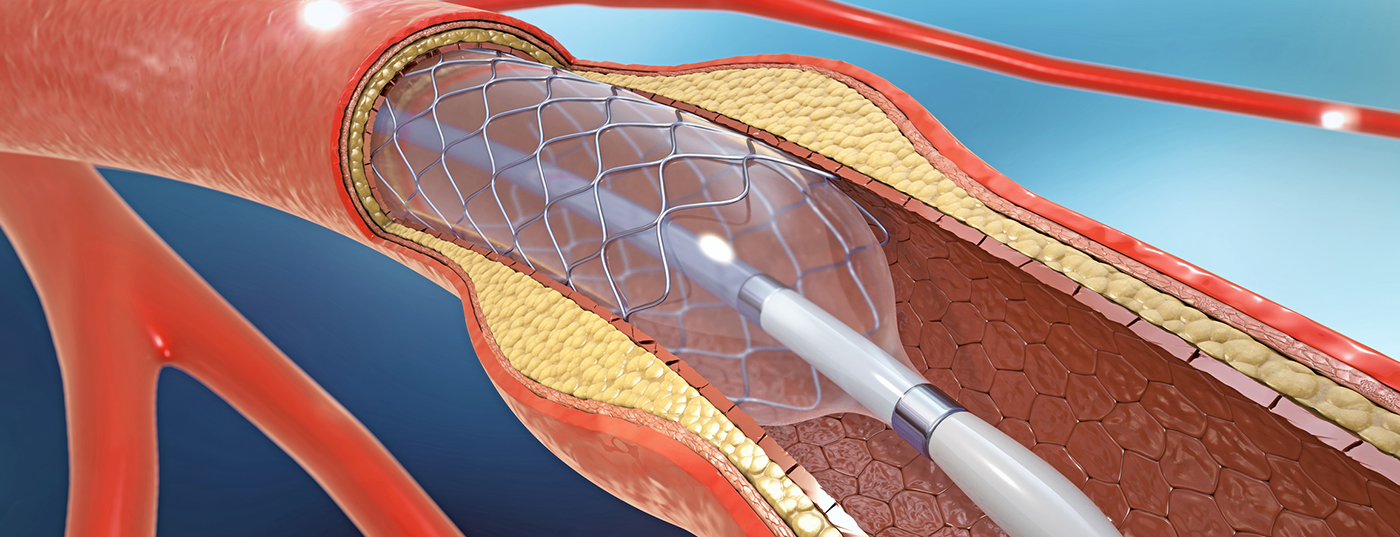
If the basilar artery is affected in a stroke (so-called acute basilar artery occlusion), this can quickly become life-threatening, because the basilar artery supplies the cerebellum and brain stem, where vital nerve centers are located, such as the respiratory center. As with all ischemic strokes, therapy must begin as soon as possible; the time window is usually considered to be 4.5 hours. The later it is started, the greater the risk that damage will remain. Specific therapy may involve drug dissolution of the clot (intravenous thrombolysis) or mechanical removal of the thrombus with a vascular catheter intervention (interventional or endovascular/intravascular thrombectomy). Combining both procedures is also useful in certain situations, such as longer transport times to the nearest thrombectomy center.
Whether those with basilar artery occlusions benefit from intravascular thrombectomy as much as those with occlusions of other large cerebral arteries has not been adequately established by clinical randomized trials. Two studies from China with a total of over 500 participants have now been published on this issue.
In the prospective randomized trials BAOCHE (“Basilar Artery Occlusion Chinese Endovascular”) [1] and ATTENTION (“Endovascular Treatment for Acute Basilar-Artery Occlusion”) [2], affected individuals with basilar artery occlusion were analyzed over a period of several years. The duration from symptom onset to randomization was 6-24 hours [1] or could not exceed 12 hours [2]. In both studies, intravenous lysis could be started first (i.e., if no individual contraindications or study exclusion criteria were present). Further treatment was either standard therapy (“standard/best medical care”) plus endovascular thrombectomy (thrombectomy group) or standard conservative therapy alone (control group). The primary outcome was good functional status at 90 days, defined as an mRS score of 0-3 (on the modified ranking scale of mRS 0 = no symptoms/disability to 6 = death). The primary safety outcome included symptomatic intracranial hemorrhage at 24-72 hours and 90-day mortality.
In the BAOCHE study [1], 217 participants were finally evaluated (110 in the thrombectomy group and 107 in the control group, average age about 64 years, about 73% men). Randomization was median approximately 11 hours (663 minutes) after symptom onset. Thrombolysis had been received by 14% of participants in the thrombectomy group and 21% in the control group. In the ATTENTION trial [2], 340 participants were included in the analysis (226 in the thrombectomy group and 114 in the control group; mean age approximately 66 years, 66 and 72% men, respectively). Randomization had occurred after a median of approximately five hours (300 minutes). Thrombolysis had been received by 31% and 34%, respectively.
The BAOCHE trial [1] was stopped after a prespecified interim analysis because of the superiority of thrombectomy. A good mRS score of 0-3 had been achieved by 46% (n=51/110) in the thrombectomy group – compared with 24% (n=26/107) in the control group (adjusted RR 1.81, p<0.001). Symptomatic intracranial hemorrhage occurred in 6/102 (6%) in the thrombectomy group and in 1/88 (1%) in the control group (RR 5.18). The 90-day mortality was 31% in the thrombectomy group and 42% in the control group (adjusted RR 0.75). Complications from treatment occurred in 11% in the thrombectomy group.
In the ATTENTION trial [2], 46% (n=104/226) in the thrombectomy group also achieved good functional status (mRS score ≤3) at 90 days – compared with 23% (26/114) in the control group (adjusted RR 2.06, p<0.001). Symptomatic intracranial hemorrhage occurred in 12/226 participants (5%) in the thrombectomy group, compared with 0% in the control group. The 90-day mortality was 37% in the thrombectomy group and 55% in the control group (adjusted RR 0.66); complications associated with the procedure occurred in 14% in the thrombectomy group (including one death due to arterial perforation).
“Two relatively large, randomized prospective studies showed a significant therapeutic benefit of additional mechanical thrombectomy to standard therapy in acute basilar artery occlusion – practically twice as many patients achieved a good functional outcome,” commented Prof. Dr. Hans-Christoph Diener, Essen, Germany. “Mortality over 90 days, however, remained high at about one-third, although it was significantly lower than with standard therapy alone.”
“The significant reduction in mortality of up to 34% occurred despite more frequent complications overall, such as the higher risk of intracerebral hemorrhage,” Diener said. “In the two studies, however, the time windows for starting therapy were significantly more than the 4.5 hours otherwise required. To further improve treatment outcomes, it will be important to ensure that patients reach the hospital as quickly as possible, even for this particular type of stroke.” However, the expert also points to the particular patient population of the studies, which make it difficult to transfer the results: The majority of participants were from Asia, with a higher proportion of preexisting basilar artery stenoses than Caucasians. “It would be desirable if studies confirmed the results in a European population.”
[1] Jovin TG, Li C, Wu L et al. for the BAOCHE Investigators. Trial of Thrombectomy 6 to 24 Hours after Stroke Due to Basilar-Artery Occlusion. N Engl J Med 2022; 387: 1373-84
[2] Tao C, Nogueira RG, Zhu Y et al. for the ATTENTION Investigators. Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion. N Engl J Med 2022; 387: 1361-72.
Source:
https://2022.dgn.org/presse/pressemitteilungen/schlaganfaelle-durch-einen-basilaris-verschluss-signifikanter-nutzen-der-thrombektomie/