The acute variant of pityriasis lichenoides is known as pityriasis lichenoides et varioliformis acuta (PLEVA) alias Mucha-Habermann’s disease. Small blotchy papules form, particularly in the area of the trunk, which in some cases are accompanied by itching or burning. A rare and severe special form of PLEVA, febrile ulceronecrotic Mucha-Habermann disease (FUMHD for short) manifests itself with an accompanying high fever and is potentially life-threatening.
A 13-year-old boy presented with a maculopapular rash that quickly spread to the palms of his hands and soles of his feet, as well as itchy, swollen and painful lips and conjunctivitis that had appeared one day before hospitalization [1]. He suffered from headaches, dizziness, fatigue, an episode of vomiting, chills and a constant fever of up to 40.5°C. The symptoms had started 2 days before hospitalization. His medical history was unremarkable, apart from mild asthma treated with inhaled steroids and an epiphysiodesis of the right tibia and femur. In the previous weeks, the family had been on vacation in Malta. There, the patient suffered from mild diarrhea. The laboratory findings showed pronounced leukopenia with an increased ratio of immature/total granulocytes, slight thrombocytopenia, an increase in C-reactive protein, procalcitonin and ferritin.
| Explanations of the therapeutic procedure The initial hematologic findings with leukopenia and thrombocytopenia documented in this case report expanded the possible differential diagnoses of febrile ulceronecrotic Mucha-Habermann disease (FUMHD) to include hematologic clinical pictures such as leukemia or hemophagocytic lymphohistiocytosis (HLH) and influenced the therapeutic considerations. In the initial course of the disease, treatment was empirical, including broad-spectrum systemic antibiotics, antifungals and antiviral treatment. Hematological diseases such as leukemia or HLH, which would have required systemic steroid treatment, were excluded. Under the impression of a possible Kawasaki syndrome or an unidentified infection, treatment with immunoglobulins was initiated [2]. The multisystemic inflammatory syndrome associated with SARS-CoV-2 in children was ruled out by repeated PCR and serology as well as analysis of a skin biopsy [3]. In the authors’ opinion, empirical treatment was retrospectively appropriate for a mycoplasma infection that may have triggered FUMHD [4]. In the further course of the disease, systemic immunosuppression was actively avoided, as secondary infectious complications via the open skin barrier were feared. As outlined in the previous literature on FUMHD, prognosis is likely to depend on timely histologic diagnosis and adequate standard treatment, including intensive care if needed. |
Skin changes in the course
The initial dermatologic findings resembled a viral exanthema [1]. On the third day, the clinical picture with conjunctivitis, mucosal involvement and exanthema showed similarities with Kawasaki syndrome. On day 6, an ulceronecrotic aspect involving the palmar and plantar regions was the predominant feature of the dermatologic changes. Healing of the mucous membranes began on 8th day and the healing of the body skin began on 9th day with detachment of the ulceronecrotic epidermal lesions.
The differential diagnostic examinations revealed the following:
- Osteomyelitis after epiphysiodesis could be excluded radiologically
- Serology was negative for acute infection with Treponema pallidum, herpes simplex virus type 1 and 2, Toxoplasma gondii, HIV, hepatitis A/B/C/D/E and SARS-CoV-2
- PCR tests were negative for adenovirus, EBV, cytomegalovirus, human herpesvirus type 6, parvovirus B19, bocavirus, human metapneumovirus, influenza A/B, measles, parainfluenza, rhinovirus/enterovirus, HSV 1/2, varicella and SARS-CoV-2.
On the other hand, a positive result for Mycoplasma pneumoniae antibodies (type IgM) was found in the serum, indicating a recent infection.
Empirical therapy was successful
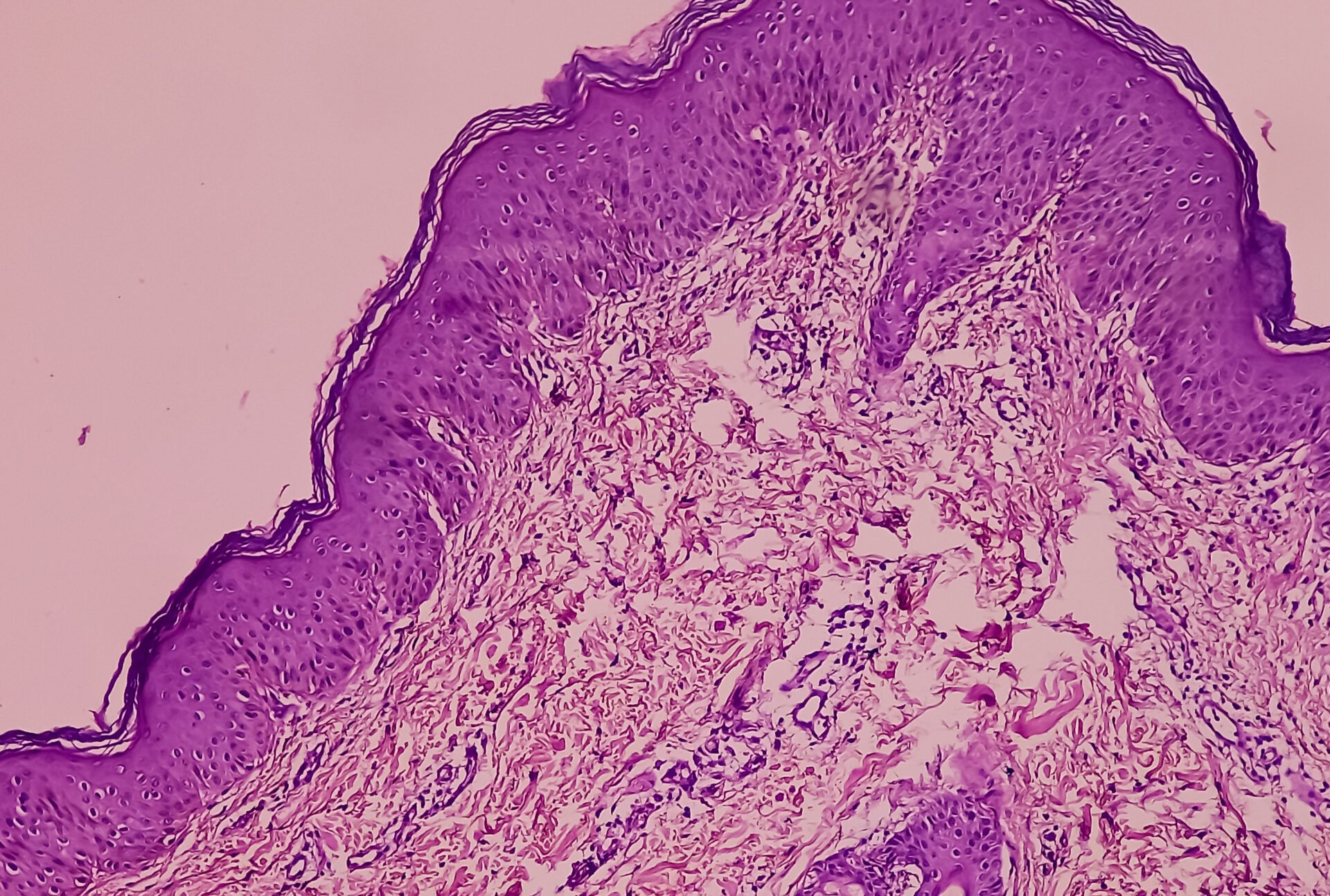
The patient was transferred to the pediatric intensive care unit on day 6 of illness due to systemic involvement with rapidly progressive skin changes, accompanied by tachycardia, oliguria and additional oxygen requirements. The bone marrow aspirate showed no malignancy and was negative for Leishmania. The skin biopsy taken on day 6 showed signs of FUMHD with interface dermatitis and predominantly CD8+ cytotoxic T cells. The PCR for SARS-CoV-2 was negative in the skin biopsy. Empirical treatment consisted of ceftazidime, vancomycin, doxycycline, liposomal amphotericin B and intravenous immunoglobulins (cumulative 2 g per kg body weight on days 6 and 7). The patient received additional oxygen and diuretics and was kept on spontaneous respiration. Topical treatment of the skin consisted mainly of topical preparations containing urea and triclosan. Under these measures, the patient’s condition improved continuously, without systemic immunosuppressive treatment. He was transferred to the normal ward on day 11 and discharged on day 18. At that time, his main complaint was still visual impairment due to corneal involvement. Retrospectively, the patient’s condition was interpreted as FUMHD, possibly triggered by a mycoplasma infection. Six months after the FUMHD episode, the patient has fully recovered without any relevant sequelae or recurrence of dermatological symptoms.
Literature:
- Blohm ME, et al: Mucha-Habermann disease: a pediatric case report and proposal of a risk score. International Journal of Dermatology 2022; 61(Issue4): 401-409.
- Weins AB, et al: Mucha-Habermann’s disease under the picture of Kawasaki syndrome. J Dtsch Dermatol Ges 2020; 18: 140-142.
- Schneider DT, Puetz-Dolderer J, Berrang J. Pediatric multisystemic inflammatory syndrome associated with SARS-CoV-2 infection. Dtsch Arztebl Int 2020; 117: 431.
- Terraneo L, et al: Unusual eruptions associated with mycoplasma pneumoniae respiratory infections: review of the literature. Dermatology 2015; 231: 152-157.
DERMATOLOGY PRACTICE 2023; 33(6): 21