On the first day of the Swiss Derma Day congress in Lucerne, the focus was on sexually transmitted diseases. A differentiated insight into the epidemiology and the possibilities of diagnosis and therapy was offered. In between, remarkable casuistics provided the necessary practical relevance.
Severin Läuchli, MD, University Hospital Zurich, gave an update on the management of HPV infection. This is the most common sexually transmitted infection (STI), with 5.5 million new infections per year in the U.S., and is a major carcinogen (anal and cervical). 90% of anal carcinomas are caused by HPV (incidence increasing in both men and women). MSM (men who have sex with men), HIV-positive patients, and immunosuppressed patients after organ transplantation have the highest risk of developing anal carcinoma. HPV is also found in 72% of oropharyngeal carcinomas and is also an independent risk factor for HIV infection (disruption of mucosal barrier, CD4 cells in mucosa).
To date, more than 180 HPV types are known. Basically, the viruses can be divided into the so-called low-risk (with the main representatives HPV 6, 11) and high-risk group (with the main representatives HPV 16, 18). Infection occurs via skin/mucosal contact, usually at a young age, and is often transient. The incubation period is one to three months, and 90% of infections are undetectable after two years. The infection is often latent, but reactivation is still possible after years. Recently, a study showed that the risk of oral viral persistence increases significantly with male sex, older age, and especially cigarette use [1].
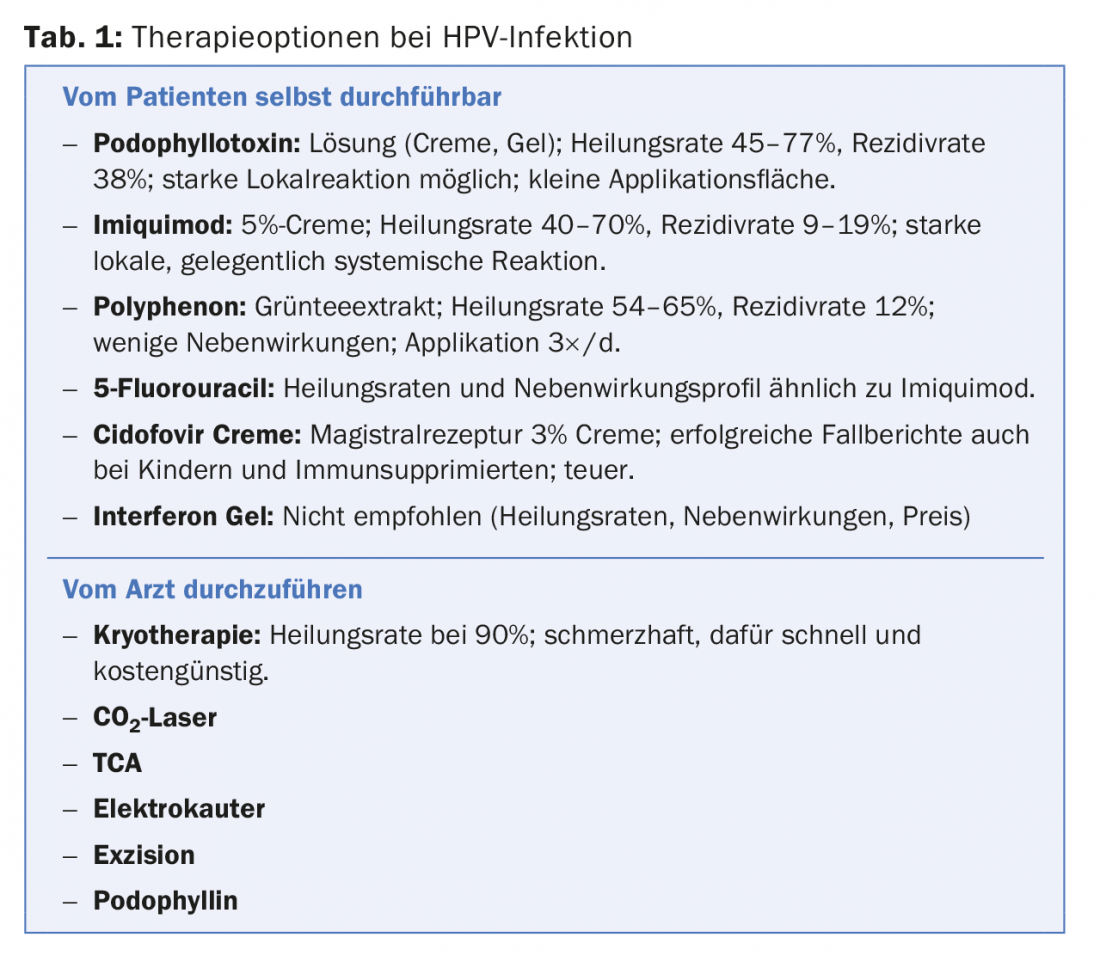
The goal of treatment is to remove symptomatic warts – even in the partner, although partner treatment has no evidence overall. The therapeutic options are summarized in Table 1. A combination therapy of a foreign-applied (cryotherapy orCO2 laser) and a self-applied procedure (podophyllotoxin for the penis, imiquimod perianal, polyphenon or 5-fluorouracil if necessary) is recommended. For example, combiningCO2 laser with imiquimod 3×/week for three months achieved a success rate of 65.4% with a recurrence rate of 7.3% at six months [2].
“Regarding surgical risk with theCO2 laser, although viral DNA has been detected in smoke and on the surgeon, warts are no more common overall in laser surgeons than in the normal population, according to one study [3],” he said.
In the U.S., HPV vaccination is recommended for girls up to age 26 as well as for boys. The FOPH recommends vaccination of all girls before their 15th birthday (two doses of vaccine 4-6 months apart, “catch-up” vaccination up to age 26 with three doses). At the time of the event, the question of what immunization efforts should be undertaken in boys was still unanswered. In the meantime, however, the FOPH has also extended its vaccination recommendations to the male sex.
Update on gonococci
“The number of gonococcal infections is slightly decreasing in Switzerland for the first time since 2014,” said Philipp Cesana, MD, University Hospital Basel. Demographically, (homosexual) men from the 20-24 age group are most affected. The incubation period for infection with Neisseria gonorrhoeae is two to seven days. Males usually develop classic urethritis; females often present with cervicitis and concomitant urethritis or a nonspecific clinical presentation (in more than 50% of females, the infection remains asymptomatic). Pharyngeal and rectal gonorrhea is asymptomatic in 90% of cases. “In high-risk individuals (MSM, HIV, multiple partners), it is therefore reasonable to perform gonococcal screening of the pharynx and rectum,” Dr. Cesana said. “A correctly performed swabbing technique significantly increases the yield. Pharyngeal care must be taken to apply sufficient pressure when swabbing. The oropharynx including both tonsils should be swabbed. The elicitation of gag reflex correlates with the detection rate [4].”
Of all the detection methods, the “Nucleic Acid Amplification Tests” (NAATs) have the highest diagnostic sensitivity and can be used with virtually all clinical test materials. However, it should be noted that NAATs from female urine specimens have lower sensitivity compared to genital swab specimens. Before antibiotic treatment, a gonococcal culture should always be performed in addition to gene amplification.
Highly resistant pathogens or treatment failure to ceftriaxone have not been observed in this country. However, due to resistance trends abroad, it is to be expected that the resistance situation will continue to deteriorate in Switzerland as well. For uncomplicated Neisseria gonorrhoeae infection of the urethra, cervix, rectum, or pharynx, the 2012 IUSTI/WHO guidelines recommend a single dose of 500 mg ceftriaxone i.m. in combination with 2 g azithromycin per os. The Federal Commission on Sexual Health also recommends 500 mg ceftriaxone for all sites and even during pregnancy and lactation, but combined with 1 g azithromycin. Treatment in special situations (invasive infection, resistance, etc.) should be done in consultation with a specialist. A so-called “test of cure”, i.e. a therapy control, is generally indicated for all treated persons (two weeks after the end of therapy by means of NAAT). If the symptoms persist three to seven days after the start of treatment or if there is a recurrent course after an initial response, it is mandatory to perform a culture and – if this is negative – a supplementary NAAT.
All partners in the last 60 days should be tested by NAAT and culture due to the high rate of infection. Partner treatment must be performed simultaneously (i.e. before the test result is available). If the therapy has been completed and there are no more symptoms, sexual intercourse must be avoided for one week.
Hepatitis and STI
According to Prof. Andri Rauch, MD, Inselspital Bern, acute hepatitis B is most commonly sexually acquired in adults in Switzerland. 23% of sexual partners of patients with acute hepatitis B also become infected within six months. With regard to hepatitis A and C, epidemics are observed among homosexual men, but these two virus types are not considered sexually transmissible per se and are mainly transmitted orofaecally via involuntary contamination (A) or via blood, e.g., through intravenous drug use (C). The increase in “sexually transmitted” hepatitis C (with a concomitant decrease in the classic injection-induced form) is due in no small part to certain sexual techniques, such as fisting or causing bloody anorectal trauma, whose practice is increasing.
The goal of all hepatitis therapies is to avoid long-term hepatic complications. Acute HCV infection is more likely to become chronic than acute HBV infection (50-85% vs. 5-25%), and the risk of cirrhosis or any subsequent hepatocellular carcinoma is high for both forms after ten years (in some cases it is 20-25%). The viral life cycle dictates the treatment goal in that viral suppression is the goal for HBV and thus years to lifelong therapy is necessary, but for HCV viral elimination and thus a cure is in prospect. Thus, it is primarily hepatitis C treatment that has recently attracted much attention (and also criticism). The interferon-free combinations of direct antiviral drugs (DAA) caused a real revolution with cure rates of more than 90% – this with shorter therapy duration, simpler intake mode and good tolerability. However, due to pricing and access restrictions, they also trigger profound ethical and professional discussions.
Oral manifestations
Some case studies of oral STI manifestations were presented by Prof. Peter Itin, MD, University Hospital Basel. The motto of the first case was: Do not forget the proximate causes. A 35-year-old male patient presents because of new onset of oral mucosal changes. The medical history shows that the man has been HIV-positive for years but is reliably taking the antiretroviral drugs and has no detectable viral load. He is in a committed relationship. Physical examination is normal, laboratory unremarkable. What is the diagnosis? The simplest explanation here is the correct one: hematoma after orogenital intercourse, the so-called fellatio syndrome.
Another case involved a patient with painful aphthae (for two months) and 8 kg weight loss. The diagnosis here was: Lues II. “And again it shows: Syphilis is the chameleon of dermatology,” says Prof. Itin. “Typical oral mucosal lesions in stage II syphilis include condylomata lata, angina specifica, plaques opalines, and erosive cheilitis. Dental manifestations (Hutchinson’s teeth) are possible in congenital syphilis.” In any case, the congenital form should be kept in mind, he said, because in recent years there has been a marked increase in infected women of childbearing age [5].
“10% of HIV-infected individuals have their first clinical manifestation in the oral mucosa,” Prof. Itin explained. For example, one of these manifestations, HIV-associated aphthosis, has the following features: atypical localization (anywhere in the oral mucosa), atypical size (unusually large), atypical course (protracted healing over months), and atypical therapeutic response (extremely refractory to therapy).
Anorectal manifestations
Finally, Prof. Dr. med. Stephan Lautenschlager, Stadtspital Triemli, presented the case of a 42-year-old patient who had been suffering from recurrent anal abscesses for a year. He had already undergone three surgeries, was married, and reported no same-sex contact. His medical history was otherwise unremarkable. Finally, lymphogranuloma venereum (caused by Chlamydia trachomatis L1-L3), which is rare in the Western world but appears to be increasing in frequency, was identified [6]. The STD occurs predominantly among homosexual (HIV-positive) men in Western regions. The most common is the Chlamydia trachomatis L2b variant (much rarer L2c). The numbers are too small to document any clinical differences between the different variants.
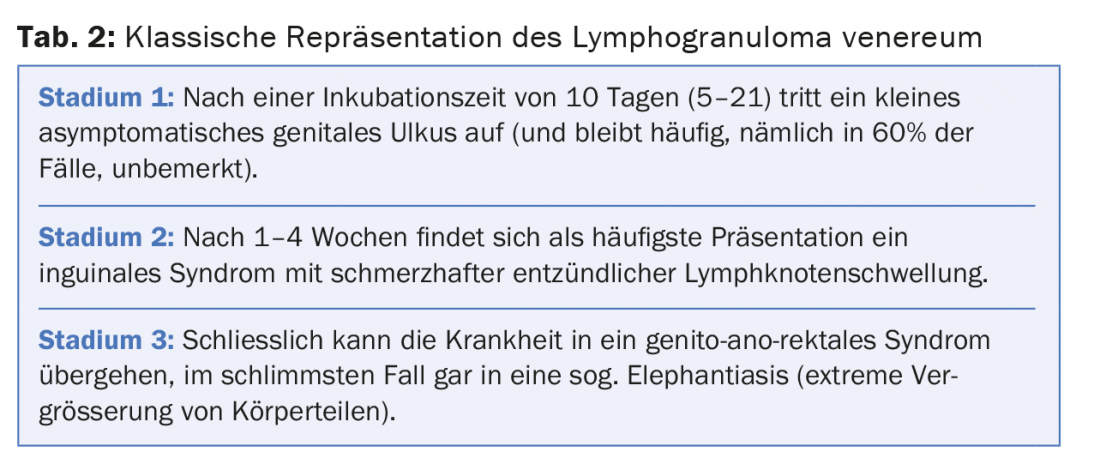
Classically, the condition presents in three stages (Table 2). However, in the current epidemic among homosexual men, proctitis and anorectal ulcers, rectal pain, bloody/purulent rectal discharge, absence of inguinal “bumps,” and constipation are characteristic. According to a recent study [7] of 587 Dutch people, there is currently no evidence that lymphogranuloma venereum spreads as rapidly among heterosexuals as it does among homosexual men (although a few cases have been observed in Europe in recent years).
There is little evidence overall on therapy: oral doxycycline 2× 100 mg/d for three weeks (recommended), erythromycin 4× 500 mg/d for three weeks (second-line), and possibly azithromycin 1 g/week for three weeks (no evidence) may be considered. The new 2013 IUSTI guidelines [8] also recommend STI screening of all patients with lymphogranuloma venereum including HIV and HCV testing. To exclude reinfection, a control screening three months after diagnosis is recommended.
Based on several case reports, the possible spectrum of STI perianal, endoanal and rectal was presented in a final overview. Especially in the presence of proctitis, STDs must be included in the differential diagnosis in MSM, but also in women.
Source: Swiss Derma Day, January 28-29, 2015, Lucerne
Literature:
- Beachler DC, et al: Risk Factors for Acquisition and Clearance of Oral Human Papillomavirus Infection Among HIV-Infected and HIV-Uninfected Adults. Am J Epidemiol 2015 Jan 1; 181(1): 40-53.
- Hoyme UB, et al: Effect of adjuvant imiquimod 5% cream on sustained clearance of anogenital warts following laser treatment. Infect Dis Obstet Gynecol 2002; 10(2): 79-88.
- Gloster HM, Roenigk RK: Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol 1995 Mar; 32(3): 436-441.
- Mitchell M, et al: Sampling technique is important for optimal isolation of pharyngeal gonorrhoea. Sex Transm Infect 2013 Nov; 89(7): 557-560.
- Meyer Sauteur PM, et al: Congenital syphilis in Switzerland: gone, forgotten, on the return. Swiss Med Wkly 2012 Jan 11; 141: w13325. doi: 10.4414/smw.2011.13325.
- Vargas-Leguas H, et al: Lymphogranuloma venereum: a hidden emerging problem, Barcelona, 2011. Euro Surveill 2012 Jan 12; 17(2). pii: 20057.
- Heiligenberg M, et al: No evidence for LGV transmission among heterosexuals in Amsterdam, the Netherlands. BMC Res Notes 2014 Jun 10; 7: 355.
- de Vries HJC, et al: 2013 European Guideline on the Management of Lymphogranuloma Venereum. J Eur Acad Dermatol Venerol 2014 [epub ahead of print].
DERMATOLOGIE PRAXIS 2015; 25(2): 34-36