Scabies occurs worldwide and affects people of all ages. In this country, there has recently been an increase in the number of cases. The clinical picture of scabies is varied and is largely determined by the number of mites and the age and immune status of those affected. The combination of permethrin and ivermectin is still considered the first-line treatment. There are various explanations for the recent increase in treatment failure with permethrin. Consistent implementation of the recommended measures can increase the chances of successful treatment.
Since the end of 2023, there has been a significant increase in cases of scabies in Switzerland [1]. If scabies is not treated, there is a risk of superinfections, according to Dr. Siegfried Borelli, Head Physician, Dermatology Outpatient Clinic, Triemli City Hospital, Zurich [2]. The infection caused by the scabies mite Sarcoptes scabiei var. hominis is limited to the stratum corneum of the epidermis – the entire life cycle of the mite takes place in this compartment [3]. The intense itching induces frequent scratching and scratch excoriations facilitate infection of the lesions with bacteria, typically streptococci or staphylococci. “We very often see patients, especially from the asylum sector, with corresponding superinfections, which is not uncommon,” reported the speaker [2]. The clinical consequences of a superinfection with streptococci can be serious and can range up to erysipelas, lymphangitis and lymphadenopathy [3]. In group A streptococci, rheumatic fever and glomerulonephritis occur as complications [4].
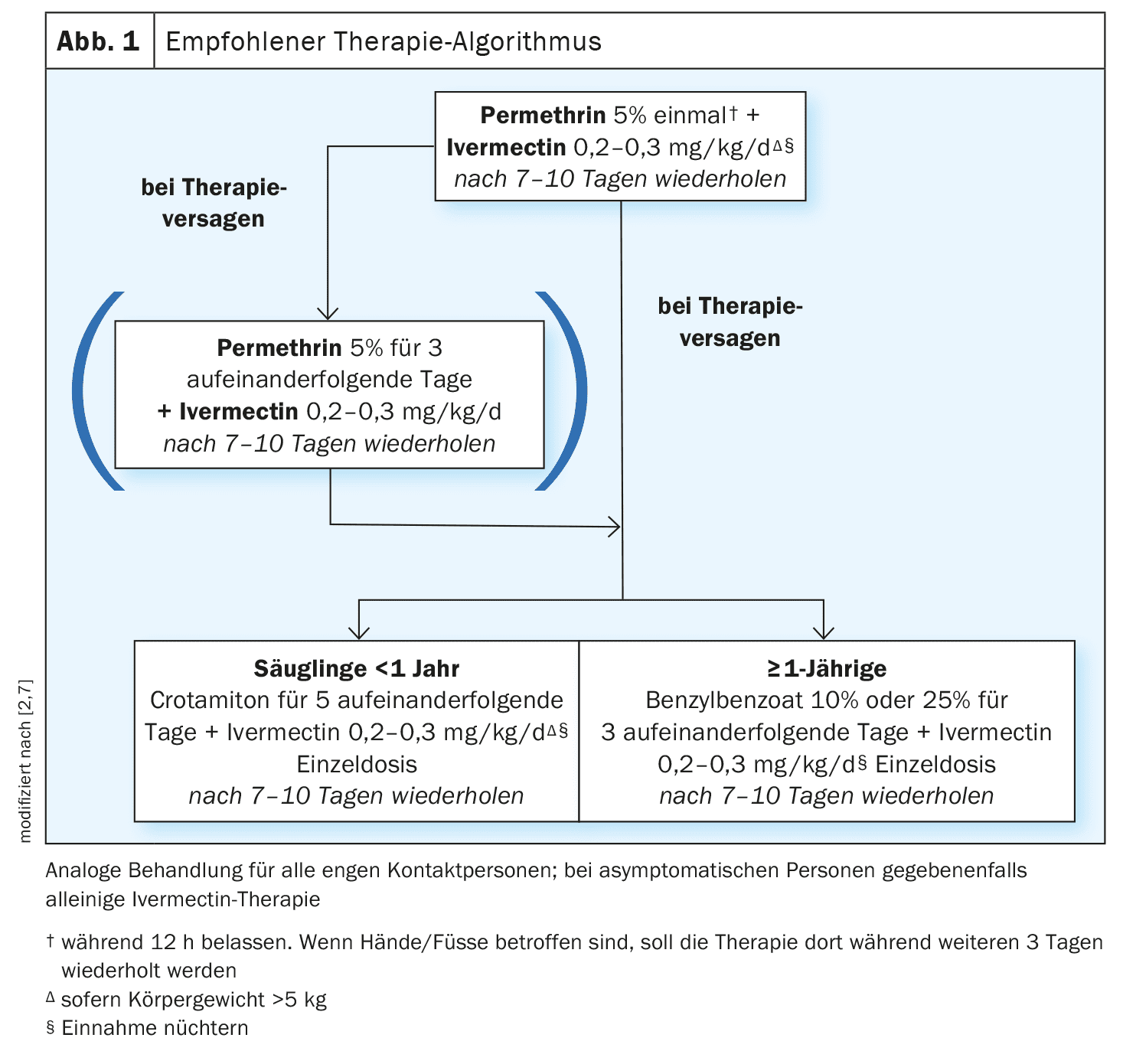
As a rule, scabies is transmitted through direct skin-to-skin contact. Theoretically, transmission of scabies mites via textiles is possible, but rarely occurs [5]. As a first-line treatment for scabies, it is recommended to combine permethrin 5% cream with systemic therapy with ivermectin (capsules or suspension) and to repeat this after 7-10 days (Fig. 1) [2]. Scabi-med® 5% (permethrin) cream is currently the only permethrin preparation approved in Switzerland and is covered by basic health insurance [6]. Permethrin has insecticidal, acaricidal and insect repellent properties. Ivermectin capsules or suspensions can be prepared as an extemporaneous preparation in pharmacies and covered by health insurance [7]. Ivermectin has antiparasitic and antihelmintic properties. The effects are based on binding to glutamate-controlled chloride channels, which are found in nerve and muscle cells. The result is increased permeability of the cell membranes for chloride ions and hyperpolarization.
Typical efflorescences in classic localization
In an initial infection, the first symptoms appear after two to five weeks [5]. Epidemics are not uncommon with scabies. The risk of outbreaks is particularly high in facilities where people live together in a confined space for long periods of time. Scabies should be suspected if there are very itchy, papulovesicular efflorescences at a typical predilection site and the itching intensifies at night. The primary efflorescences consist of comma-like mite ducts a few mm to 1 cm long, at the end of which a small vesicle sometimes forms [5]. Predilection sites for scabies are the interdigital folds of the hands and feet, axillae, elbows, areola, navel, penis shaft, inguinal, perianal and ankle regions and the inner edges of the feet [3]. The back is rarely affected, the head and neck are usually spared. In infants and young children, however, typical skin lesions are also found on the hairy head, face and palmoplantar region.
The diagnosis of scabies is preferably made by a dermatologist. Collaboration between dermatologists, general practitioners and the institution concerned is crucial in the further course of the disease. According to the consensus criteria of the International Alliance for the Control of Scabies, the clinical picture of scabies includes at least one of the following criteria [8]:
- Scabies passages
- Typical skin changes on the male genitals
- typical skin changes in characteristic distribution and two anamnestic features (itching, positive contact history).
The diagnosis is confirmed by the microscopic detection of mites, eggs or scybala from skin scrapings or by the detection of mites using a dermatoscope (reflected light microscopy) or adhesive tape test [5].
Special case of Scabies crustosa
The risk of infestation correlates positively with the number of mites on the patient’s skin and is very high in Scabies crustosa. In this case, mites multiply unchecked, so that even brief skin contact can lead to infestation. With immunosuppression, the risk of developing scabies crustosa is higher, which is why this is more common in old people’s homes and care facilities. The clinical picture differs from that of common scabies and shows diffuse hyperkeratosis, occasionally crusts and bark on an erythematous base with fine to medium lamellar scaling, often with palmoplantar hyperkeratosis and nail infestation [5]. The typical itching is often mild or completely absent in this form of scabies. Predilection sites are the fingers, back of the hand, wrists and elbows [3]. There is a tendency to spread to the scalp, ears, toes, soles of the feet and back.
Scabies therapy: real or supposed permethrin resistance?
In the recent past, there have been increasing reports of treatment failure with permethrin and there is debate about what this is all about. The speaker presented a publication published in the British Journal of Dermatology in 2024 [2,9]. The secondary analysis by Mbuagbaw et al. included 147 randomized and quasi-randomized studies published in the period 1983-2021 [9]. The analysis showed that treatment failure was higher in studies after 2011 than in the period before (17.4% vs. 12.8%). Furthermore, it was shown that treatment failure increased by 0.27% per publication year. Whether the observed phenomenon of treatment failure is a genuine permethrin resistance or a pseudo-resistance (e.g. due to incorrect application) has long been the subject of debate among experts.
The mechanism of action of permethrin is a selective neurotoxic effect on arthropods, whereby this effect is caused by disruption of voltage-dependent sodium channels resulting in prolonged sodium influx into nerve cells [5,10,11]. There are several possible explanations for resistance to permethrin. Firstly, there is the hypothesis of metabolic resistance, i.e. that repeated application of permethrin in sublethal doses induces elimination enzymes in the mites, which can lead to a reduction in the effectiveness of permethrin [13].
Another explanation is provided by the hypothesis of genetic resistance, which refers to a knockdown resistance mutation in the mites’ sodium channel gene [5,14]. A publication published in JEADV in 2023 was able to prove genetic resistance. It showed that a Kdr-associated M918L mutation in the VSSC gene in Sarcoptes scabiei var. hominis leads to the following effects [12]:
- The structure of the sodium channels is changed,
- Pyrethroids can no longer bind effectively,
- Sodium channels close normally, which leads to normal nerve function and corresponds to resistance to pyrethroids
Pyrethroids bind to sodium channels and keep them in an open state. This causes overexcitation of the nerve cells and leads to paralysis and death of the insect.
What are the implications for anti-scabiosis treatment?
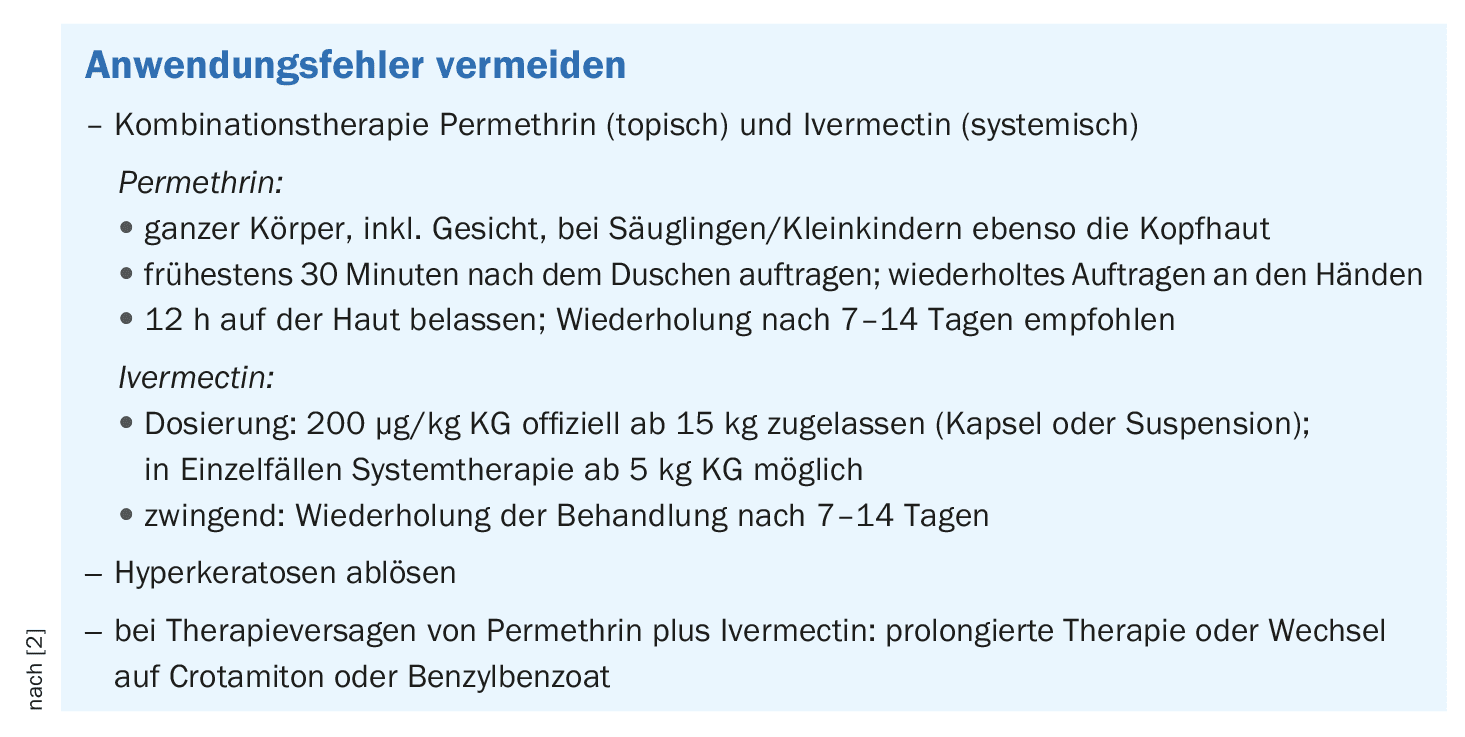
Dr. Borelli summarized some important points that should be considered when treating scabies with permethrin 5% cream and systemic ivermectin (capsules or suspensions) in order to increase the chances of successful treatment. It is strongly recommended to combine permethrin with ivermectin, whereby the treatment should always be adapted to the age and weight of the patient (Fig. 1). It is also advisable to extend the exposure time of permethrin to 12 h if possible. If this combination treatment does not work, crotamiton or benzyl benzoate** can be used for 3-5 consecutive days, with washing off only at the end of the treatment cycle. The speaker pointed out that renewed anti-scabial therapy is only indicated after renewed detection and mentioned post-scabial eczema in this context [2]. Post-scabial eczema is a skin rash as a result of local therapy or dryness of the skin. Anti-inflammatory ointments and creams work best against this.
** Benzyl benzoate: adults 25%; children 10%
In addition to the combined multiple treatment with permethrin and ivermectin, topical keratolysis with external agents containing salicylic acid or urea and, if necessary, mechanical removal of severe hyperkeratosis is recommended. Permethrin should be applied to dry skin, at the earliest 30 minutes after showering. The face and neck should also be treated, apply repeatedly to the hands; fingernails should preferably be trimmed.
All close contacts in the 6 weeks prior to the onset of symptoms should be treated simultaneously and also twice (taking into account contraindications). Close contacts are [1,7]:
- Family members in the same household
- Persons living in the same room
- People who share a bed
- Children who play together for hours or have close contact. Prolonged and continuous skin contact of at least 5-10 minutes is necessary for the transmission of itch mites
- Persons with prolonged close skin-to-skin contact after occupational exposure (e.g. healthcare workers, nursing staff in homes, childcare staff) or after exposure during leisure time; in the case of Scabies crustosa, brief skin-to-skin contact is sufficient.
Furthermore, the recommended hygiene measures must be observed [1,7]: all clothes, towels, bed linen and other textiles (including stuffed animals) that have come into contact with the skin in the 4 days prior to treatment must be washed at a temperature of at least 60°C. If this is not possible, textiles should either be dry-cleaned or stored dry in a plastic bag. If this is not possible, textiles are either dry-cleaned or stored dry in a plastic bag for 3-4 days. Upholstered furniture, textile floor coverings, car seats etc. should be vacuumed.
Scabies is not notifiable. However, clusters in institutions should be reported to the cantonal medical service using the FOPH reporting form “Cluster of findings” [1,7].
Congress: Zurich Dermatology Training Days (ZDFT)
Literature:
- “Communicable diseases & vaccinations”, Canton of Zurich, www.zh.ch/de/gesundheit/gesundheitsberufe/fachspezifische-informationen/medizin.html#981665765,(last accessed 09.10.2024).
- “Parasitic skin infections”, Dr. med. Siegfried Borelli, Zurich Dermatology Training Days (ZDFT), 22-23.06.2024.
- Robert Koch Institute (RKI): Scabies infestation, 2009, https://edoc.rki.de,(last accessed 08.10.2024).
- Heukelbach J, Feldmeier H: Scabies. Lancet 2006; 367: 1767-1774.
- Sunderkötter C, et al: S1 guideline on the diagnosis and treatment of scabies, 2016, AWMF register number: 013-052. https://register.awmf.org,(last accessed 09.10.2024)
- Swissmedic: Medicinal product information, www.swissmedicinfo.ch,(last accessed 09.10.2024)
- Canton of Zurich, Department of Health: Scabies, leaflet, Cantonal Medical Service, June 2024, www.zh.ch,(last accessed 09.10.2024).
- Engelman D, et al: The 2020 International Alliance for the Control of Scabies Consensus Criteria for the Diagnosis of Scabies. Br J Dermatol 2020; 183(5): 808-820.
- Mbuagbaw L, et al: Failure of scabies treatment: a systematic review and meta-analysis. Br J Dermatol 2024: 190: 163-173.
- Currie BJ, McCarthy JS: Permethrin and ivermectin for scabies. N Engl J Med 2010; 362: 717-725.
- Zlotkin E: The insect voltage-gated sodium channel as target of insecticides. Annu Rev Entomol 1999; 44: 429-455.
- Riebenbauer K, et al: Detection of a knockdown mutation in the voltage-sensitive sodium channel associated with permethrin tolerance in Sarcoptes scabiei var. hominis mites. JEADV 2023; 37(11): 2355-2361.
- Sunderkötter C, Wohlrab J, Hamm H: Epidemiology, diagnosis and therapy of scabies. Dtsch Arztebl Int 2021; 118: 695-704.
- Pasay C, et al: High-resolution melt analysis for the detection of a mutation associated with permethrin resistance in a population of scabies mites. Med Vet Entomol 2008; 22: 82-88.
DERMATOLOGIE PRAXIS 2024; 34(5): 38-40 (published on 28.10.24, ahead of print)