Breast-conserving therapy is the standard of surgical treatment for breast carcinoma and should be offered to all age groups. Mastery of oncoplasty is an important foundation for meeting both oncologic and plastic demands. An interdisciplinary therapy concept is a prerequisite for individual and optimal therapy in every breast cancer patient. Radical axillary surgery can be avoided in most cases.
At the end of the 19th century, physicians were convinced that extensive surgery was the best treatment for breast carcinoma. Thus, William Stewart Halsted developed radical mastectomy with removal of the mammary and pectoral muscles, including axillary lymph nodes. It was not until 1977, when the first results of the NSABP-B-04 trial showed that so-called modified mastectomy (removal without muscle, MRM) combined with radiotherapy was equivalent to radical mastectomy in terms of disease-free survival and overall survival, that the rethinking began. The subsequent NSABP-B-06 trial provided the major breakthrough for breast conservation with radiotherapy after breast-conserving surgery, which is equivalent to mastectomy. With 70-75% breast-conserving breast carcinomas operated on, this therapy is now the standard. Since the advent of genetic analysis and the associated search for BRCA-1/2 mutations, there seems to be a renewed trend toward mastectomy, particularly in the United States. In senology and breast surgery, the question of prophylactic mastectomy or mastectomy for non-BRCA mutations is increasingly being raised.
Oncological safety meets aesthetics
Breast-conserving therapy places technically quite different demands on breast surgery than mastectomy. The inclusion of the so-called oncoplasty allows the combination of an oncologically safe removal of the tumor with an appealing preservation of the breast shape. Breast-conserving therapy almost always results in a reduction of breast volume. This should be done as far as possible without large dent formation, distortion of the nipple or scarring of the décolleté. The breast-tumor relationship is as diverse as the demands of individual patients and requires broad oncoplastic knowledge and a great deal of empathy on the part of the breast surgeon.
The required distance to the resection margin has been continuously corrected downwards in recent years, so that today only one row of cells is required between the ink-marked resection margin (“ink = margin”) and the tumor (“no ink on tumor”). This principle is independent of molecular subtype or the presence of an intraductal component.
However, in the presence of ductal carcinoma in situ (DCIS) alone, 2 mm distance to the resection margin is required, and large prospective studies are lacking. In synopsis, it seems strange that more radical surgery is still called for in the preliminary stage.
Surgical techniques and radiotherapy
The following surgical techniques are commonly used in oncoplasty:
- Round block technique with periareolar approach (Fig. 1)
- B-Plastic
- Dermoglandular displacement flap
- Inverted T-plasty and tumor-adapted
- Reduction plastic
- Modified Lejour technique
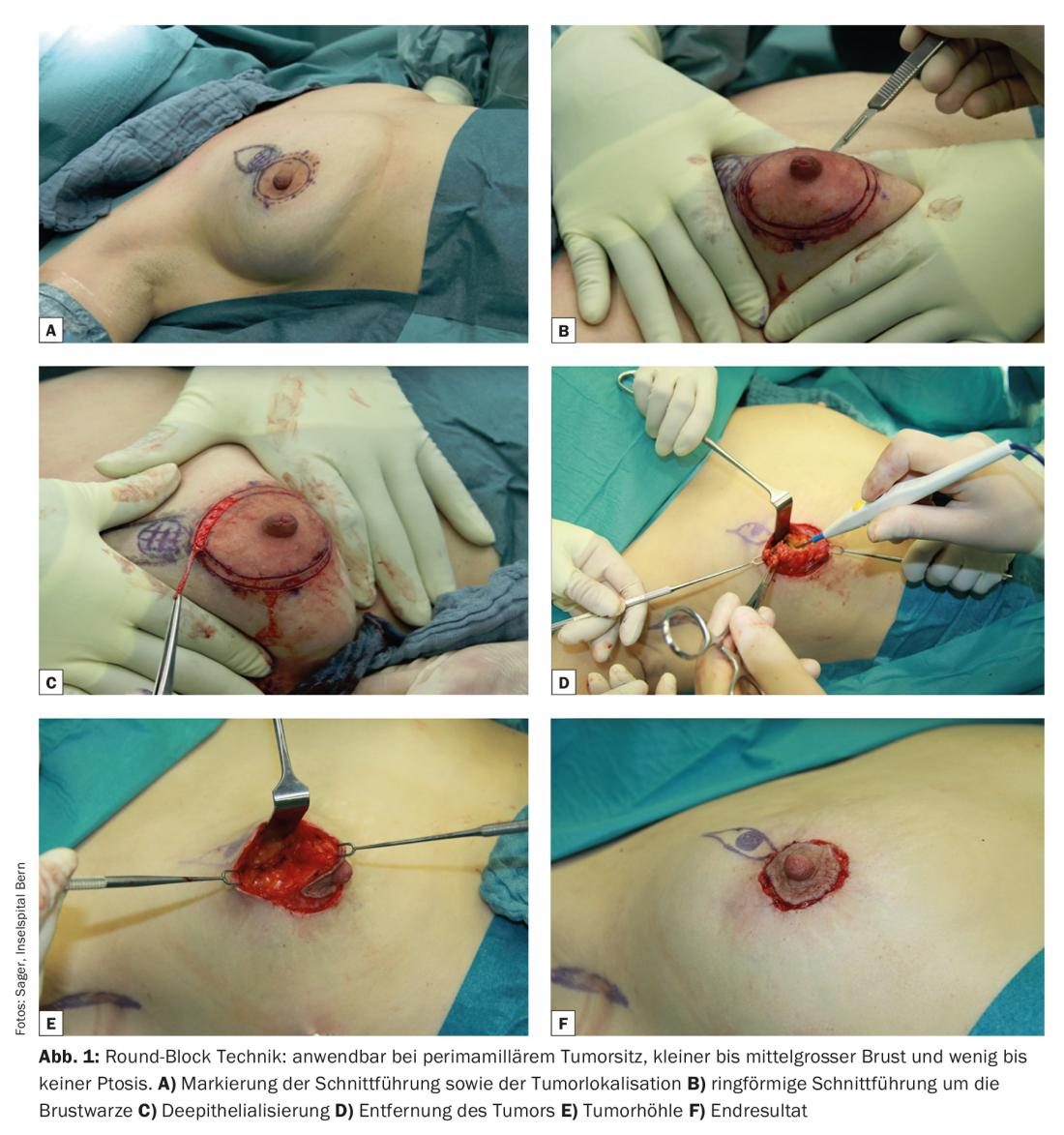
All these techniques and their combinations include defect coverage with the patient’s own breast tissue. If a greater asymmetry is to be expected, an adjustment of the other side of the breast is possible. Especially in the case of hyperplastic mamma, this not only represents a cosmetic effect, but also enables simplified follow-up care due to the reduction of glandular tissue. For some years now, such an adjustment has also been covered by health insurance.
Breast-conserving therapy always entails radiotherapy of the mammary gland. This must always be explicitly discussed with the patient. Older patients often struggle with the thought of weeks of radiation and often desire ablation for this reason. With partial breast irradiation (HD brachytherapy), it is possible to avoid weeks of radiation. As a result, older patients are increasingly opting to preserve their breasts. The applicators, which act as a guide for the steel sources to the tumor, can be used intraoperatively after breast-conserving therapy. Partial breast irradiation can take place immediately postoperatively. This only prolongs the stay by a few days, and also puts less strain on the heart, lungs and skin.
A new breast or the skin and nipple sparing mastectomy with reconstruction
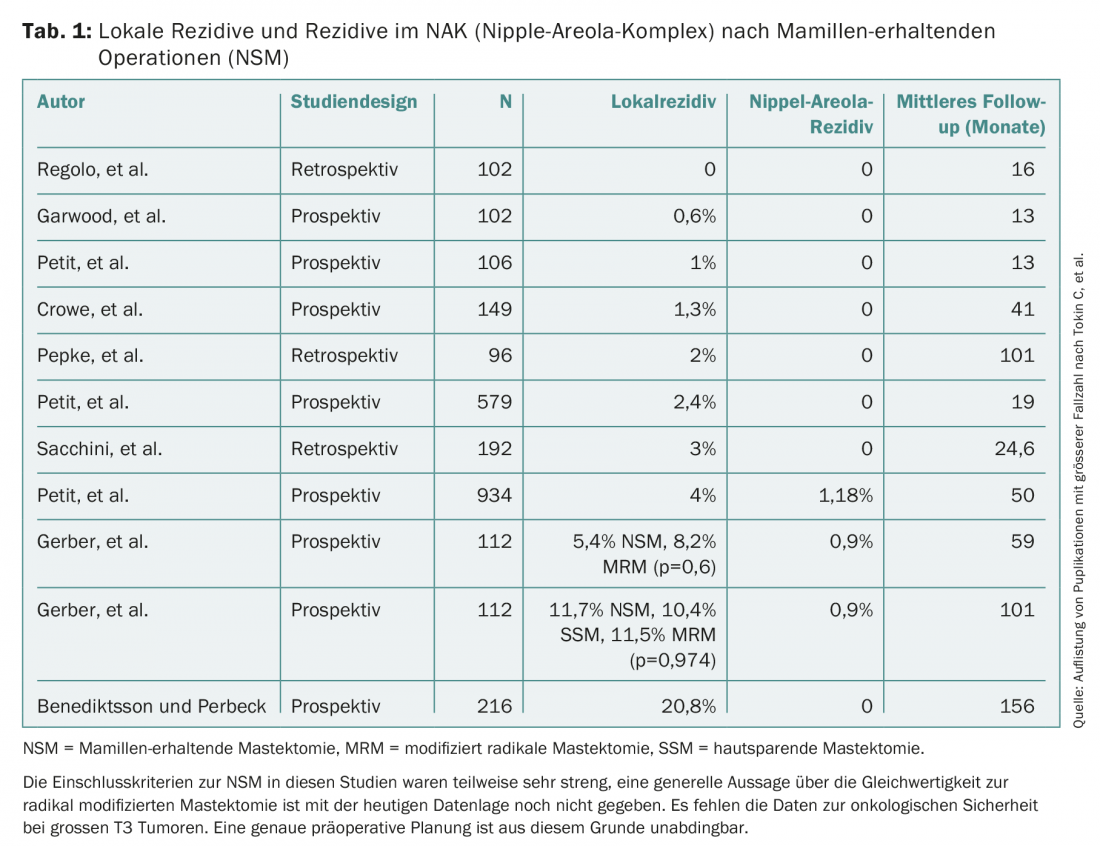
In cases of large multicentric tumor and unfavorable breast-tumor ratio, the possibility of skin-sparing or nipple-sparing mastectomy (SSM/NSM) with reconstruction is discussed. In this procedure, the entire glandular body is removed and replaced either with an implant or with the patient’s own tissue. Oncologic safety is highly dependent on resection of the glandular tissue as completely as possible. This places certain demands on the surgeon. If the resection is too radical, the blood supply to the skin suffers and necrosis may occur. If too much glandular tissue is left, the recurrence rate is too high (Tab. 1) . In most cases, it should be possible to preserve the nipple. The following must be observed: The tumor must be approx. 2 cm from the nipple. Intraoperatively, a retromammillary frozen section is performed to confirm the absence of tumor in this area. No glandular tissue should be left in the retromammary area. The volume is then restored either autologously using flap plasty or heterologously using a silicone implant. A matrix (Strattice® or TiLoop®) is often used for the caudal covering of the implant. This is used to fix the muscle in retromuscular insertion.
For many women, decision making is very difficult when they are newly diagnosed with breast cancer. A close-meshed care in an interdisciplinary setting is indispensable for a successful and satisfactory therapy of the patients. All tumor patients should be presented and evaluated in an interdisciplinary preoperative board. It should be noted that any augmentation can never replace the natural breast. It is therefore all the more important to prepare patients sufficiently for the “new breast”.
Can surgery of the axilla still be justified?
With improved preoperative diagnostics and very high-resolution ultrasound equipment, assessment of the axilla has become very precise. Axillary dissection per se has not been performed for a long time. Today, targeted sentinel excision (removal of the sentinel lymph node) is standard in clinically negative axilla. But even this established standard is being shaken up. The INSEMA study and the SOUND study are currently investigating whether sentinel biopsy can even be omitted in clinically negative axilla. The first results are expected in 3-5 years.
Already, axillary dissection should be avoided if the tumor is small and there is only micrometastasis (IBCSG-23-01 trial). Already the meta-analysis by Sanghani et al. of three large trials evaluating axial dissection vs. no axial dissection showed no advantage in overall survival, axillary recurrence, or locoregional recurrence. Since the publication of the Z0011 study, axillary dissection can be omitted under certain conditions in the case of a single macrometastasis in the sentinel lymph node and prior clinically unremarkable axilla. The dreaded lymphedema, which considerably restricts the patients’ quality of life, can thus be avoided.
Conclusion
Oncologic safety and aesthetics are very compatible in mammary surgery. In doing so, the breast surgeon must be proficient in a wide range of oncoplastic and reconstructive procedures. The planning of these mammary procedures must be interdisciplinary in a preoperative board. This is the only way to achieve high quality.
Take-Home Messages
- Breast-conserving therapy is the standard of surgical treatment for breast carcinoma and should be offered to all age groups.
- Mastery of oncoplasty is an important foundation for meeting both oncologic and plastic demands.
- An interdisciplinary therapy concept is a prerequisite for individual and optimal therapy in every breast cancer patient.
- Radical axillary surgery can be avoided in most cases.
Further reading:
- Halsted WS.: A clinical and histological study of certain adenocarcinomata of the breast: and a brief consideration of the supraclavicular operation and of the results of operations for cancer of the breast from 1889 to 1898 at the Johns Hopkins Hospital. Ann Surg 1898; 28: 557-576.
- Fisher B, et al: Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002; 347: 1233-1241.
- Veronesi U, et al: Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002; 347: 1227-1232.
- Hughes KS, et al: Lumpectomy plus tamoxifen with or without irradiation in women age 70 or older with early breast cancer. J Clin Oncol 2010; 28: 15s.
- Berry MG, et al: Oncoplastic breast surgery: A review and systematic approach. J Plast Reconstr Aesthet Surg 2010; 63(8): 1233-1243.
- Krag DN, et al: Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomized phase 3 trial. Lancet Oncol 2010; 11: 927-933.
- Veronesi U, et al: Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg 2010; 251: 595-600.
- Giuliano AE, et al: Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 2011; 305: 569-75.
- Canavese G, et al: A risk score model predictive of the presence of additional disease in the axilla in early-breast cancer patients with one or two metastatic sentinel lymph nodes. Eur J Surg Oncol 2014; pii: S0748-7983(14)00350.
- Cunnick GH, Mokbel K.: Skin-sparing mastectomy. Am J Surg 2004; 188(1): 78-84.
- Cense HA, et al: Nipple sparing mastectomy in breast cancer: a viable option? Eur J Surg Oncol 2001; 27: 521-526.
- Clemens MW, Kronowitz SJ: Acellular dermal matrix in irradiated tissue expander/implant-based breast reconstruction: evidence-based review. Plast Reconstr Surg 2012 Nov; 130(5 Suppl 2): 27S-34S.
- Berry MG: Oncoplastic breast surgery: A review and systematic approach. J Plast Reconstr Aesthet Surg 2010; 63(8): 1233-43.
- Rezai M,Veronesi U.: Oncoplastic principles in breast surgery. Breast Care 2007; 2: 277-278.
- Sanghani M, Balk EM, Cady B: Impact of axillary lymph node dissection on breast cancer outcome in clinically node negative patients: a systematic review and meta-analysis. Cancer 2009; 115(8): 1613-1620.
- Tokin C, et al: Oncologic safety of skin-sparing and nipple-sparing mastectomy: a discussion and review of the literature. Int J Surg Oncol 2012; 2012: 921821.
InFo ONCOLOGY & HEMATOLOGY 2017; 5(4): 22-25.











