Urinary incontinence is common and the level of suffering is often unrecognized. Urinary incontinence needs to be further de-tabooed. Urinary incontinence should be rationally clarified and primarily treated conservatively. Surgical procedures for urinary incontinence are efficient and grateful.
Urinary incontinence includes any form of involuntary loss of urine, it is called a disease when social or hygienic problems arise for the patient [1]. Epidemiologically, incontinence is difficult to capture because it remains a taboo subject. It is estimated that about 400,000 women and men in Switzerland are affected by urinary incontinence. In the over-65 population, it is estimated that 15% of women and 10% of men suffer from incontinence.
In symptomatic incontinence, a thorough history and complete status should be obtained to differentiate between the different forms of incontinence. This also includes the exclusion of a urinary tract infection, a residual urine determination, and a cystoscopy. For further rational clarification, a conclusive urodynamic examination helps [2]. Once the form of incontinence has been determined, appropriate conservative therapy, usually consisting of pelvic floor physiotherapy and drug therapy, can be initiated. If conservative therapy does not improve the symptoms, a surgical procedure can be evaluated.
The surgical therapy concept is primarily based on the underlying etiology of the incontinence. Table 1 shows the different forms of incontinence with their causes, symptoms and treatment options.

Stress incontinence
Stress incontinence is due to inadequate closure of the urethra, which manifests itself in situations where intra-abdominal pressure is increased. Typically, this is the case, for example, when coughing or laughing; in more severe forms, urine leakage already occurs when climbing stairs and, in the most severe form, even at rest. In male patients, radical prostatectomy is the most common cause of pelvic floor weakness; in women, it is age-related or childbirth-associated decrease in muscular pelvic floor tone. Surgical treatment of stress incontinence thus starts with the mechanical support of the pelvic floor.
Bulking agents: Short-term improvement of sphincter function can be achieved using bulking agents. These are applied submucosally to the sphincter zone during urethrocystoscopy to form urethral padding. Since the effect lasts only three months on average, this is only an option for patients who are only seeking temporary symptom improvement or are inoperable due to secondary conditions [2]. In men after prostatectomy, this method is not suitable because the injection site is in the area of the vesicourethral anastomosis, which is usually scarred.
Slings: In both women and men, an artificial abutment dorsal to the urethra, to improve the urethral closure mechanism, can be inserted using minimally invasive sling insertion.
In women, the retropubic tension-free urethral tape (“Tension-free Vaginal Tape” [TVT]) is most commonly used and achieves a continence rate of 75% [3]. In this procedure, a blunt needle is used to push the two ends of a polypropylene tape between the bladder and the symphysis from the vaginal side. Alternatively, the sling can be pulled through the obturator foramen, which is equivalent to a transobturator TVT. However, with this method, patients are more likely to suffer from pelvic pain postoperatively than with retropubic DVT, but the risk of bladder perforation is lower [2]. The hospitalization time is short with these procedures and they can be performed even in old age.
In men, there are two concepts to improve continence by means of a sling. One approach is based on urethral compression, which increases urethral resistance and thus improves continence. The second approach is aimed at repositioning the bulbar urethra. In addition, there are sling systems that can be retightened in the event of insufficient continence postoperatively; these are then referred to as adjustable slings. However, these have an increased rate of infection. The success rates of the different sling systems are comparable and are around 50-75% [4–6].
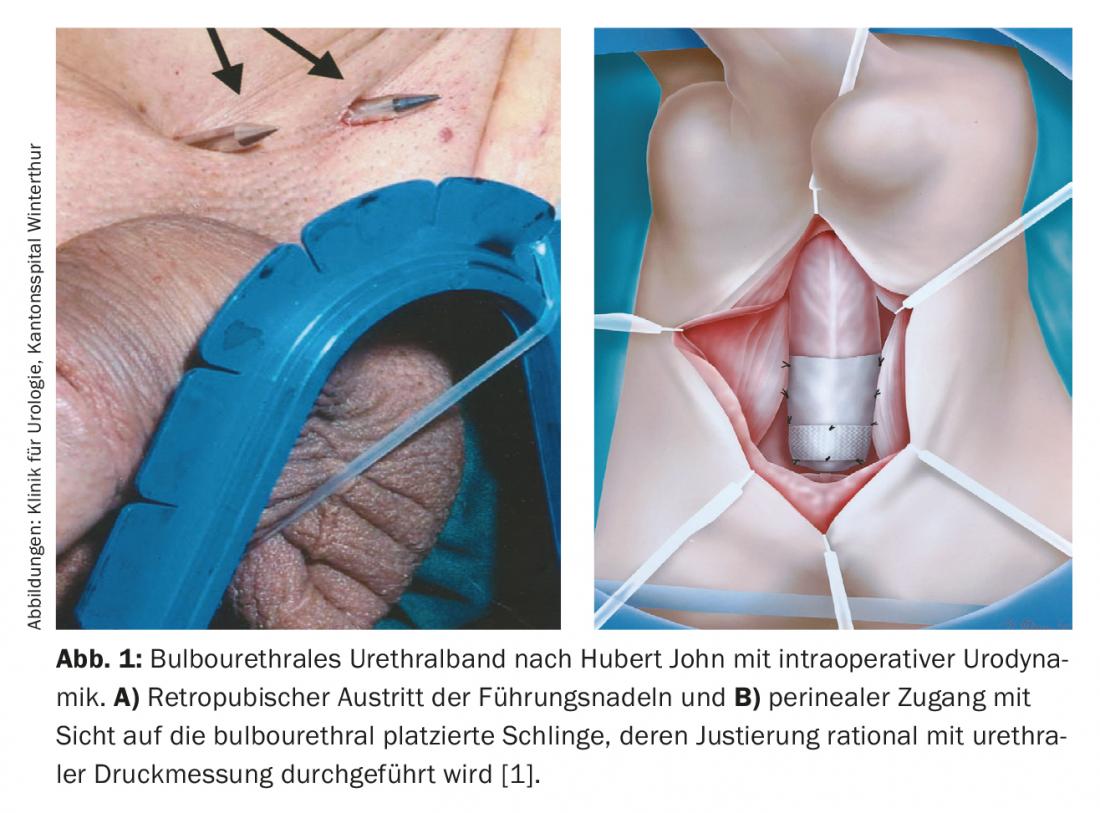
At the Winterthur Cantonal Hospital, we use the bulbourethral suspension developed by Prof. Hubert John in 2002 in men, for which urodynamics with urethral pressure measurement is performed intraoperatively and readjusted accordingly (Fig. 1A and B). The principle of action is based on the reduction of the urethra without exerting compression on the urethra. The success rate for this technique is 74% [7–10]. Only 15% of men still require the creation of an artificial sphincter after this sling technique in the course, which is technically still quite possible – but in 85% of these men, spontaneous micturition can be obtained without implantation of significant foreign material.
Artificial sphincter: As an alternative to tape techniques, there is the possibility of AMS sphincter implantation. It is often the first choice for severe incontinence after radical prostatectomy or small pelvic radiation, but is also used in women. It consists of an inflatable periurethral cuff, a pressure-regulating balloon, and a control pump. By manually pressing the balloon, which is placed in the scrotal compartment for men and in the labia area for women, the cuff is deflated prior to micturition and allows micturition without resistance.
The system is implanted through a perineal incision for placement of the cuff, and an incision in the lower abdomen through which the balloon and control pump are inserted.
The success rate is 80%, which is higher than with the sling systems. However, the revision rate is 20% in the first five years [5,11]. Reasons for revision are infections, arrosions and urethral atrophies. Preoperatively, it should be ensured that patients are cognitively and manually able to operate the sphincter system.
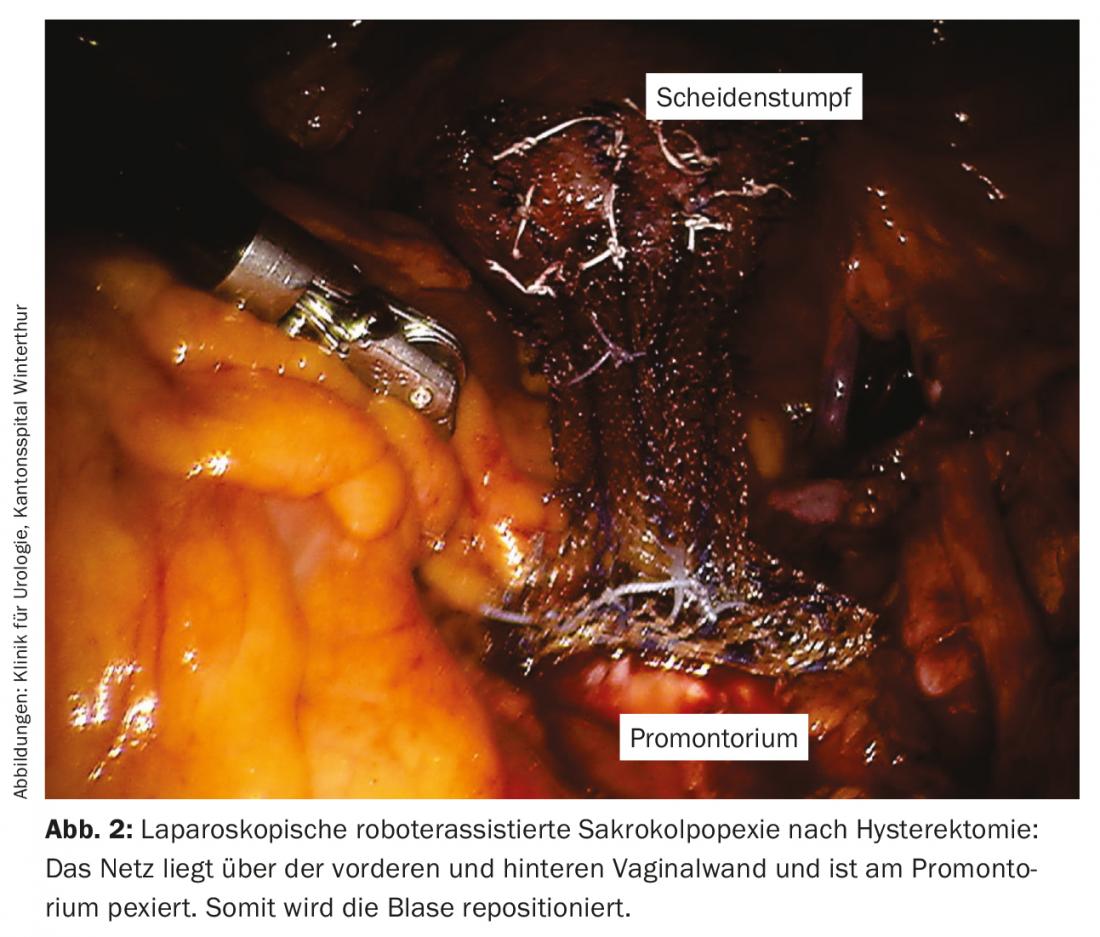
Laparoscopic robot-assisted sacrocolpopexy: In the case of stress incontinence with simultaneous descensus genitalis, the option of vaginal sacrospinous fixation or abdominal sacrocolpopexy is available as a therapy for women in addition to conservative pessary therapy. We favor laparoscopic robotic-assisted sacrocolpopexy using the DaVinci™ 4-arm system. The technique is suitable for reduction of all three pelvic floor compartments and is beneficial for a sexually active woman to avoid vaginal surgery. Vaginal mesh inserts have also been criticized. In sacrocolpopexy after hysterectomy or with uterus in situ, the bladder is repositioned through the mesh strips (polypropylene interposition) from the anterior and posterior vaginal wall to the promontory (Fig. 2). Special risks of the operation are access-related possible intestinal lesions and bleeding, which, however, are rarities in the literature. Occasionally, unmasked stress incontinence occurs after sacrocolpopexy.
Urge incontinence
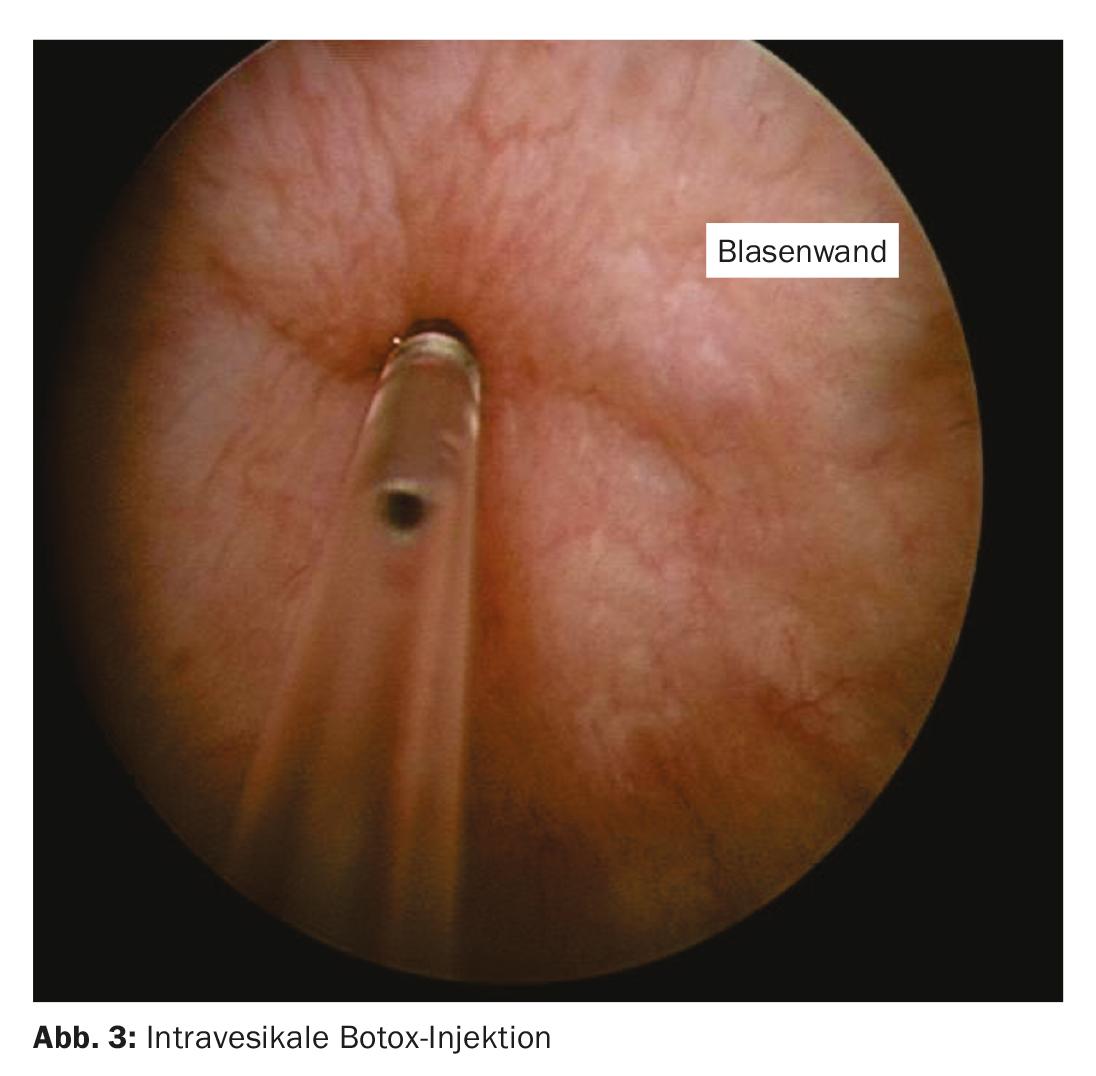
Urge incontinence often involves irritable bladder conditions that lead to bladder hypersensitivity. These include infections, bladder tumors, postactinic irritable bladders, or infravesical obstructions such as prostatic hyperplasia or urethral strictures. For these forms, the treatment of choice is causal therapy. Urge incontinence can also be triggered by neurological diseases, such as multiple sclerosis or Parkinson’s disease. If drug therapies have been exhausted, there is the option of a transurethral botulinum toxin type A injection into the detrusor muscle (Fig. 3). The toxin is injected into the bladder wall at 20 points, leaving out the trigone. However, patients must be informed that the effect begins only after 10-14 days and that the duration of action is on average six months, and accordingly the injections must be repeated [12,13]. There is also an increased risk of residual urine formation and the possibility of urinary retention, which must be treated by catheter. In about 5% of patients, such urinary retention occurs, triggered by too strong an effect of the toxin, which is why the residual urine must be checked by sonography after two weeks.
After failure of the above-mentioned surgical options, there is still the surgical option of bladder augmentation, in which the bladder is expanded with a small bowel segment, which eliminates the involuntary contractions. The urinary bladder can be completely eliminated by means of a cystectomy with creation of an ileum conduit or a neobladder; the operation represents the ultima ratio (Fig. 4).

Overflow incontinence
In overflow incontinence, urine leakage occurs when the bladder is overfull. In the case of a hypocontractile bladder, drug therapy is the primary treatment. In hyposensitive bladder, regular bladder emptying is the key therapeutic concept. If high residual urine volumes persist despite regular bladder emptying, intermittent self-catheterization can be learned. At our clinic, this is carried out by the urotherapist, who instructs women and men in the appropriate time slot.
However, subvesical obstruction often underlies the disease. In men, this is usually prostatic hyperplasia, which can be corrected by means of the standard transurethral prostatic resection. Urinary tract infections are common complications, so the urine is tested for infection by the primary care physician one week after removal of the indwelling catheter. Rarely, postoperative bleeding is so severe that surgical hemostasis is necessary.
In women, overflow incontinence is often due to a hypocontractile old-age bladder or, as an iatrogenic consequence, incomplete emptying after DVT – rarely incomplete emptying after orthotopic replacement bladder.
Reflex incontinence
Reflex incontinence occurs due to spinal cord damage between the pons and the spinal cord level S2. Since the central inhibition of the spinal reflex, which starts at a certain bladder filling level, fails, involuntary bladder emptying occurs. In the first instance, reflex incontinence is treated with medication; if this fails, self-catheterization can be learned or a vesical pacemaker system implanted. In addition, there is also the possibility of eliminating the bladder by the above-mentioned cystectomy with placement of an ileum conduit.
Extraurethral incontinence
Urinary fistulas can be congenital or occur postoperatively as a complication after pelvic surgery. Urinary fistula should be considered, especially in cases of continuous urine leakage. In new (<75 days) minor vesico-vaginal fistulas, spontaneous healing may occur using a transurethral indwelling catheter. Longer standing fistulas should be addressed surgically with appropriate distress [14].
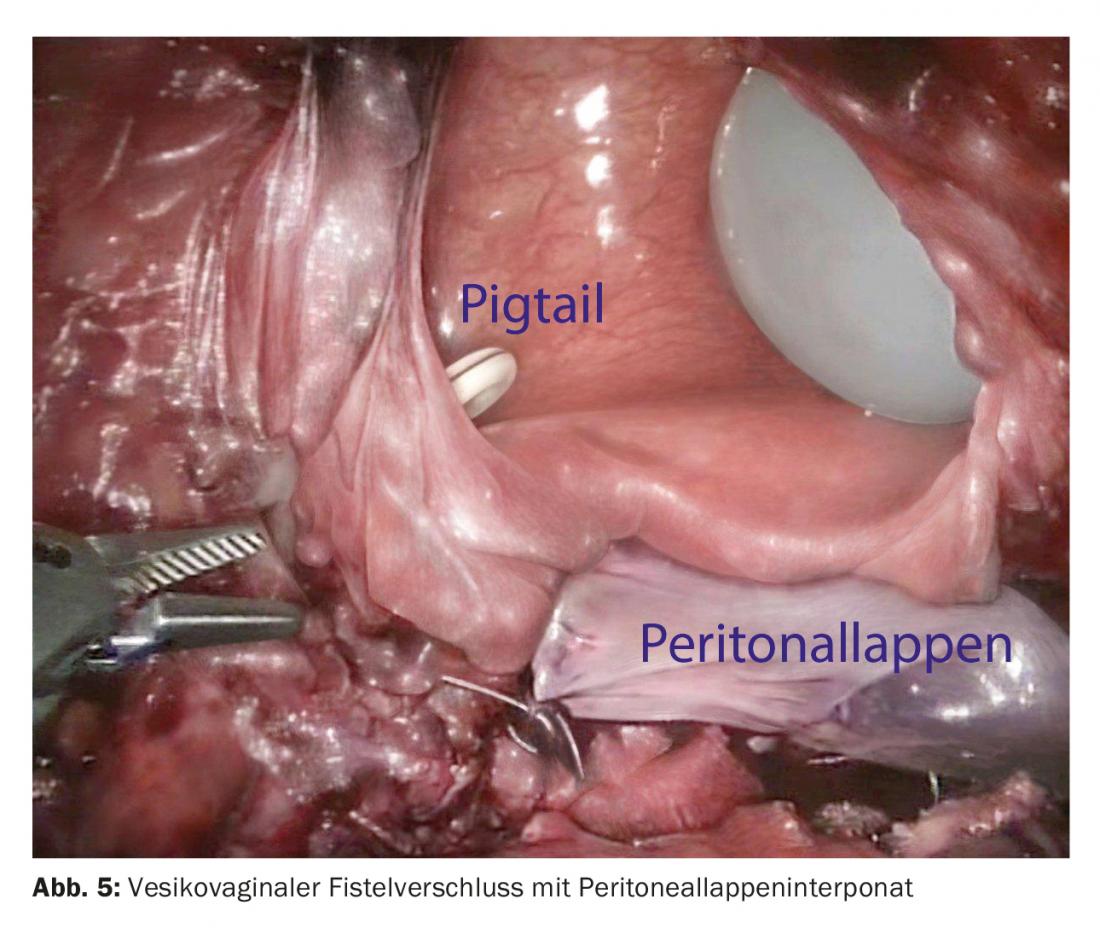
Fistula surgery depends on the extent of the fistula and also significantly on the etiology and requires an individual surgical approach from case to case. Simple high bladder fistulas after small pelvic surgery such as hysterectomy can usually be elegantly closed laparoscopically robotically [15], recurrent and postactinic fistulas require more complex surgical concepts up to upper urinary diversion to ileum conduit or catheterizable umbilical bladder (Fig. 5).
Literature:
- Abrams P, et al: The standartisation of terminology in lower urinary tract function: report from the standardisation sub-committee of International Continence Society. Urology 2003; 61: 37-49.
- Lucas MG, et al: EAU guidelines on surgical treatment of urinary incontinence. Eur Urol 2012; 62: 1118-1129.
- Ulmsten U, et al: Intravaginal sling-plasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Sand J Urol Nephrol 1995; 29: 75-82.
- Bauer RM, et al: Contemporary management of postprostatectomy incontinence. Eur Urol 2011; 59: 985-996.
- Herschorn S, et al: Surgical treatment of stress incontinence in men. Neurourol Urodyn 2010; 29: 179-190.
- Hubner WA, et al: Adjustable bulbourethral male sling: experience after 101 cases of moderate-to-severe male stress urinary incontinence. BJU Int 2011; 107: 777-782.
- John H: Bulbourethral composite suspension: a new surgical technique for post-prostatectomy incontinence. J Urol 2004; 171: 1866-1870.
- John H, et al: Mid-term outcome after bulbourethral composite suspension for postprostatectomy incontinence. Urology 2008; 71: 1191-1195.
- Horstmann M, et al: Pre- and postoperative urodynamic findings in patient after a bulbourethral composite suspension with intraoperative urodynamically controlled sling tension adjustment for postprostatectomy incontinence. Urology 2012; 79: 702-707.
- Horstmann M, et al: Comparison of stardized pre- and postoperative functional pelvic cine-MRI in patients with a bulbourethral composite suspension due to post-prostatectomy incontinence. Int Urol Nephrol 2013; 45: 967-973.
- Chung E, et al: 25-year experience in the outcome of artificial urinary sphincter in the treatment of female urinary incontinence. BJU Int 2010; 106: 1664-1667.
- Chapple C, et al: OnabotulinumtoxinA 100 U significantly improves all idopathic overactive bladder symptoms and quality of life in patients with overactive bladder and urinary incontinence: a randomized, double-blind, placebo-controlled trial. Euro Urol 2013; 64: 249-256.
- Nitti VW, et al: OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of phase 3, randomized, placebo controlled trial. J Urol 2013; 189: 2186-2193.
- De Ridder D, et al: Fistula. In: Abrams P, Cardozo L, Khoury S, Wein A (eds.): Incontinence 2013 (5th ed.). Paris: European Association of Urology and International consultation on urological diseases 2012; 1527-1579. www.icud.info/incontinence.
- Kurz M, et al: Robot-assisted laparoscopic repair of high vesicovaginal fistulae with peritoneal flap inlay. Eur Urol 2012; 61: 229-230.
HAUSARZT PRAXIS 2016; 11(12): 22-28











