A brief overview of surgical treatment options for traumatic spinal injuries, spinal tumors, and degenerative changes with paraplegic symptoms.
Paraplegia is always a major challenge for the interdisciplinary treatment team. From the surgical side, the aim is to relieve the spinal cord as quickly, completely and gently as possible and – if necessary – to restore the stability of the spinal column in order to create favorable conditions for subsequent rehabilitation. This article provides a brief overview of surgical treatment options for traumatic spinal injuries, spinal tumors, and degenerative changes with paraplegic symptoms.
Paraplegia is paralysis resulting from incomplete or complete damage to the spinal cord or cauda equina, with loss of motor, sensory and autonomic functions. These lesions can lead to tetra- or paraparesis (incomplete paralysis) or -plegia (complete paralysis), depending on the level. Initially there is a flaccid motor paralysis, the so-called “spinal shock”, later the paralyses become spastic. In addition, urogenital and rectal dysfunction occurs. Complete damage to the conus medullaris or cauda equina results in permanent flaccid paralysis.
Paraplegia is often caused by damage to the spinal cord due to a traumatic injury or tumor, and occasionally by degenerative changes in the spine. Whereas traumatic spinal injuries in most cases lead immediately to the appearance of corresponding neurological deficits, in the case of neoplasia symptoms may develop insidiously over a longer period of time, which finally often worsen acutely in the course of decompensation. The same can be observed in degenerative changes, where, for example, high-grade cervical spinal stenosis leads to acute paraplegic symptoms after a minor trauma. In these cases, a rapid response is required and the patient must be promptly evaluated neurologically and neuroradiologically.
Surgical treatment for paraplegic lesions
Surgical interventions for a paraplegic syndrome have two goals: On the one hand, complete decompression of the spinal cord to prevent secondary neurological deterioration and allow for better recovery; on the other hand, stabilization of the spine to restore its normal load-bearing capacity and function. In the case of complete paralysis, the existing neurological deficits usually cannot be reversed by surgical measures. Here, too, however, residual instability due to stretching and compression of the myelon can cause further secondary damage, which is clinically manifested mainly by an ascending level of paralysis. Restoration of spinal statics and load stability is also a prerequisite for effective early rehabilitation with avoidance of problems associated with prolonged bed confinement, such as pneumonia, pressure ulcers, muscular deconditioning, contractures, and thromboembolic events. Furthermore, successful stabilization can often significantly improve the pain situation and reduce the need for analgesics [1].
In principle, early surgical treatment is now recommended (level of evidence 2c) [2]. After acute care has been provided, paraplegic patients should be transferred as soon as possible to a specialized institution with the necessary experience in the rehabilitation of paraplegics.
Traumatic spinal injuries
Traumatic paraplegia often occurs in polytraumatized patients who require specialized interdisciplinary care. Traumatic injuries to the spine can lead to paraplegia immediately if there is direct structural damage to the myelon, but neurological symptoms may also occur with a delay if there is secondary damage to the spinal cord, for example, due to instability or hemorrhage.
Paraplegia can be classified according to its severity according to the ASIA classification (Table 1) [3]. Incomplete paraplegic lesions (ASIA B-D) usually require surgical management if myelon compression or instability is demonstrated. Similarly, a surgical approach should be chosen for the onset of paralysis after a free interval, ascending (progressive) paralysis, open spinal injury, osseous or disco-ligamentous instability, or dislocation [4]. However, evidence-based recommendations do not exist. Nursing aspects (e.g., agitation or lack of cooperation in craniocerebral injuries) must also be included in the indication. If compression compromises perfusion of the myelon, for example, compression of the anterior spinal artery (so-called “snake eyes lesion” on T2-weighted MRI) worsens the prognosis [5].
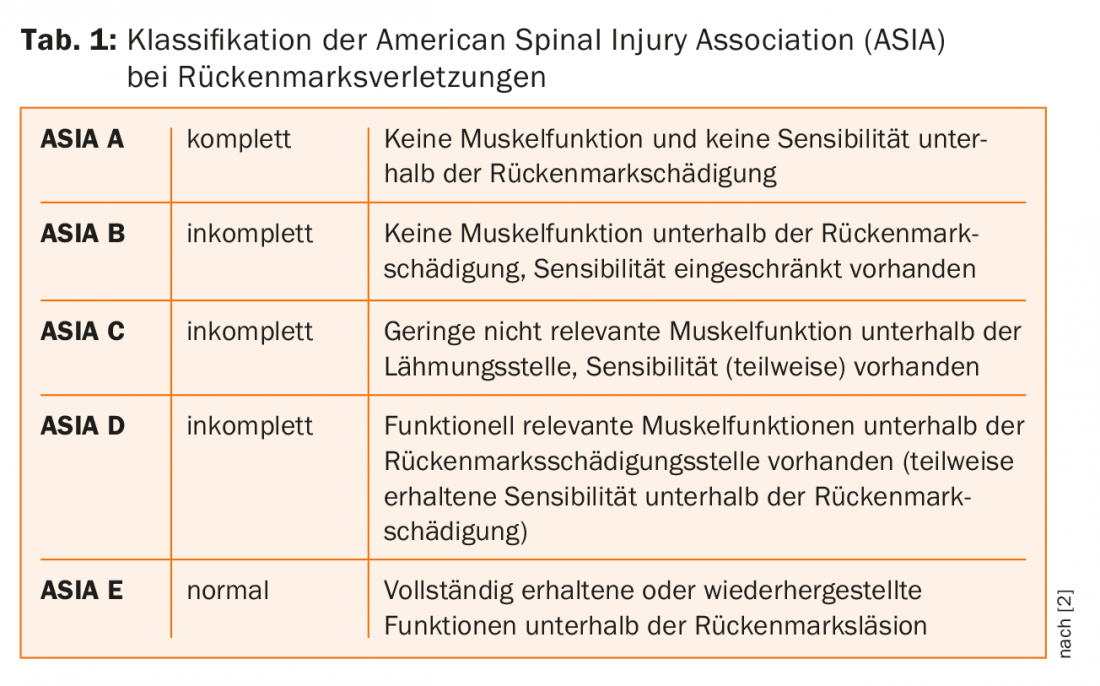
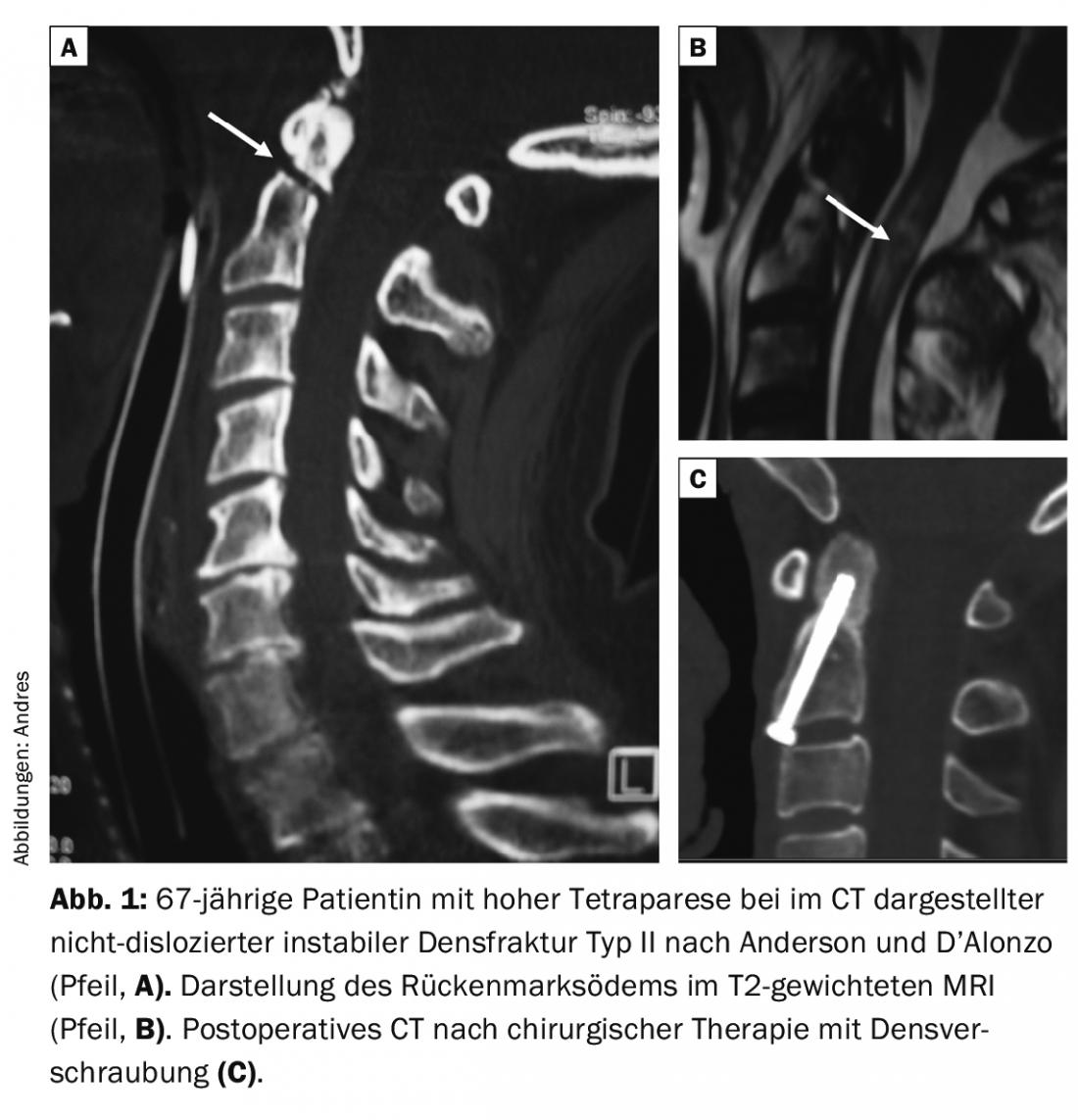
Surgical treatment is performed according to the principles of microsurgical decompression combined with reduction, straightening and stabilization. Decompression is not required for unstable fractures without residual compression of neural structures, for example, most dens fractures (Fig.1). Otherwise, osseous fragments, ruptured or prolapsed disc portions, and hematomas in the spinal canal are removed under the surgical microscope, the dura is reconstructed if necessary, displaced vertebral bodies are reduced, and whenever possible, load-stabilized fixation is performed to allow early mobilization without orthotics (Fig.2). Intraoperative electrophysiological monitoring with evoked potentials (MEP and SSEP) is now often used as standard, but a possible benefit is still controversial in the literature [6]. Whereas in the past the cervical spine was mainly treated from the front using plate osteosynthesis and the thoracic or lumbar spine was stabilized from the dorsal side using a fixator system, today the surgical technique depends on the localization and extent of the damage. Increasingly, combined restorations are being performed via anterior and dorsal approaches.

Spinal tumors
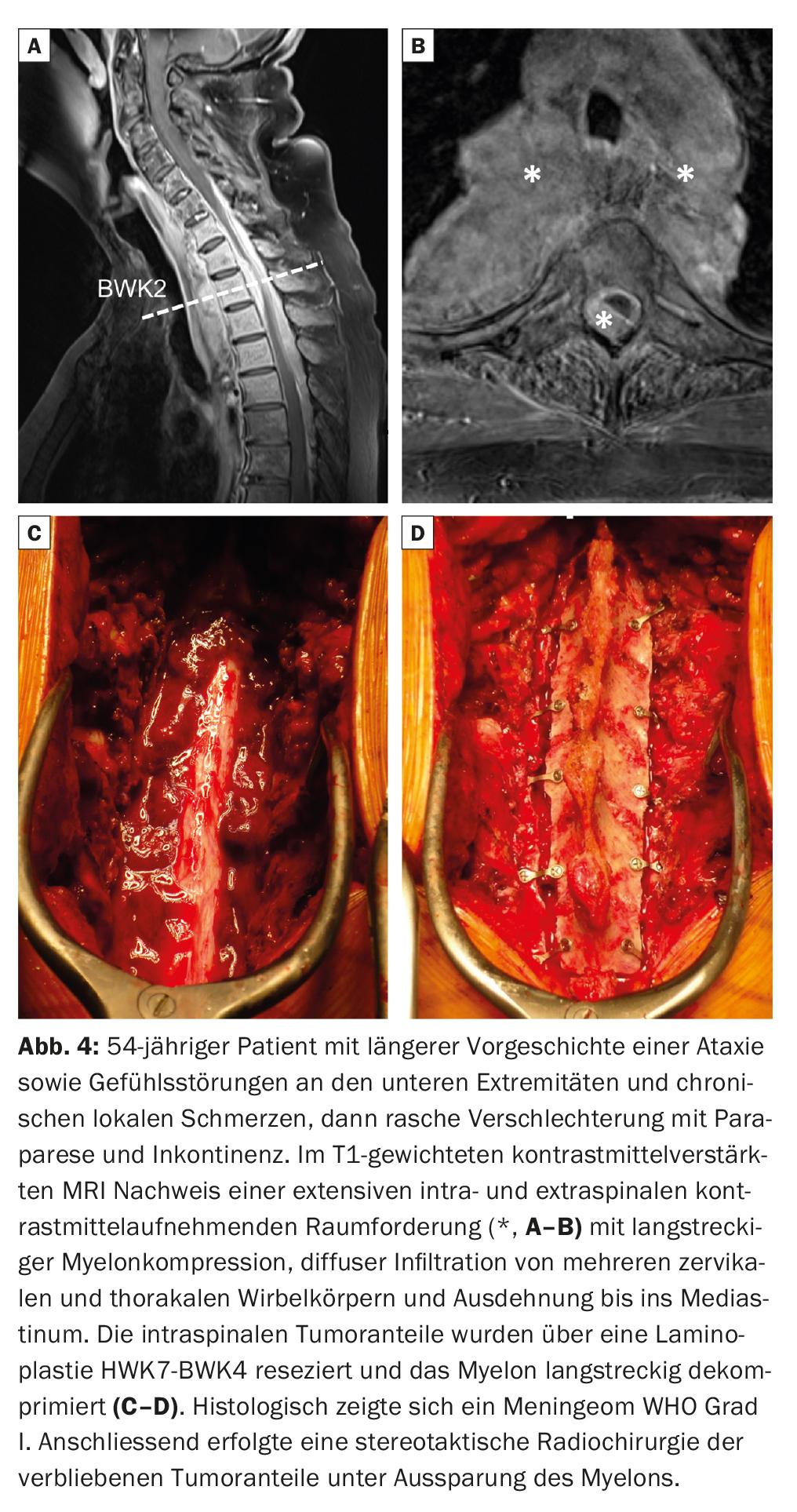
Tumors can either destroy the spinal cord directly (intramedullary tumors, e.g., ependymomas or astrocytomas), damage it by increasing pressure (usually intraspinal extramedullary tumors, e.g., meningiomas, schwannomas, or metastases), or affect it by causing instability or pathologic vertebral body fracture (usually osteolytic growing tumors of the axial skeleton such as metastases). In all of these cases, acute, subacute, or slowly increasing paraplegic symptoms may develop. Often, when tumor growth is slow, patients notice little discomfort for a long time as the myelon is slowly displaced and compressed and allowed to adapt. As soon as it reaches the limit of its compensatory capacity, severe deficits up to para- or tetraplegia quickly occur.
The available treatment options depend on the type, location and growth behavior of the tumor. The patient’s overall situation must also be taken into account when planning therapy. In principle, a function-preserving operation should be aimed for. Additional neurological deficits caused by therapy should be avoided. In thoracic tumors, segmental nerve roots can be sacrificed in favor of radicality if necessary, since only loss of sensation in circumscribed areas is the result. Cervical and lumbar procedures are generally prohibited. Here, we will try to leave the neural structures intact, even if sacrifices have to be made in terms of radicality. The interdisciplinary development of a multimodal therapy concept (oncology, neurosurgery, orthopedics, radio-oncology, pathology) is of central importance.
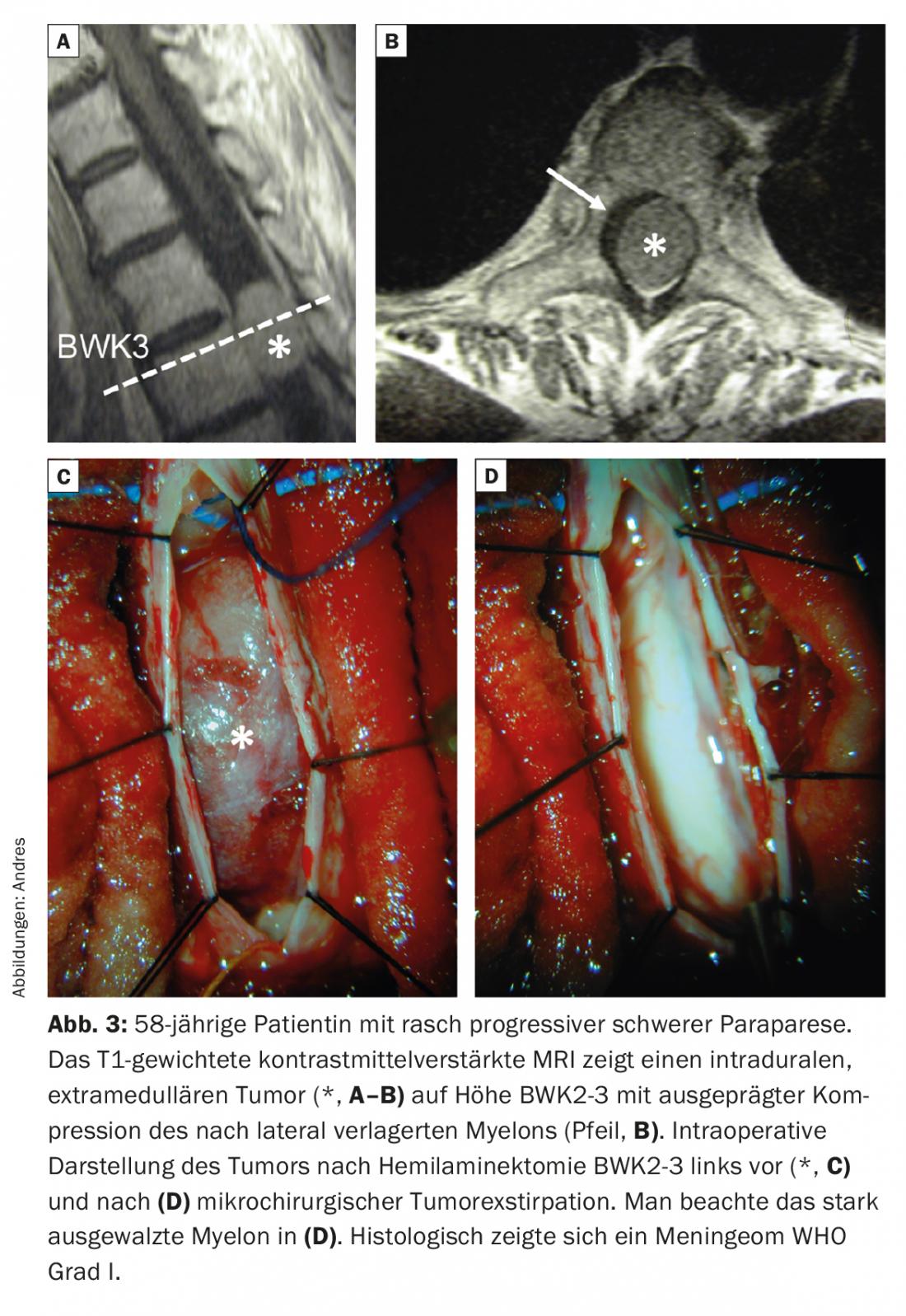
Intraspinal tumors can usually be operated on via microsurgical approaches to preserve stability (Fig. 3). For intramedullary tumors, myelotomy is performed followed by microsurgical resection. Improved neuromonitoring techniques may be helpful in sparing critical structures during surgery [7]. For extramedullary tumors, the lesion is visualized from the cranial to the caudal pole, centrally volume reduced using an ultrasound aspirator, and then circularly devascularized and dissected away. For tumors involving the vertebral body and paraspinal structures, a decision must be made as to whether these can be resected curatively in healthy tissue. Such a so-called oncologic “en bloc” resection should be sought for primary malignant spinal tumors such as sarcomas or solitary metastases from prognostically favorable primary tumors. This often requires a so-called 360° operation with combined dorsal and ventral approach and subsequent reconstruction and stabilization of the spine [8]. If this is not possible or advisable, for example in the case of diffuse growth with infiltration of the neural structures (Fig. 4) or in a palliative overall situation, the spinal cord is surgically decompressed and the tumor tissue resected if possible. If the stability of the spinal column is impaired or endangered by arrosion of the osseous structures, stabilization is performed at the same time (Fig. 5) . Subsequently, tumor control is sought by means of radio and/or chemotherapy. Modern carbon/PEEK implants, which cause few artifacts on MRI and CT, facilitate follow-up and subsequent radiotherapy.

Degenerative changes
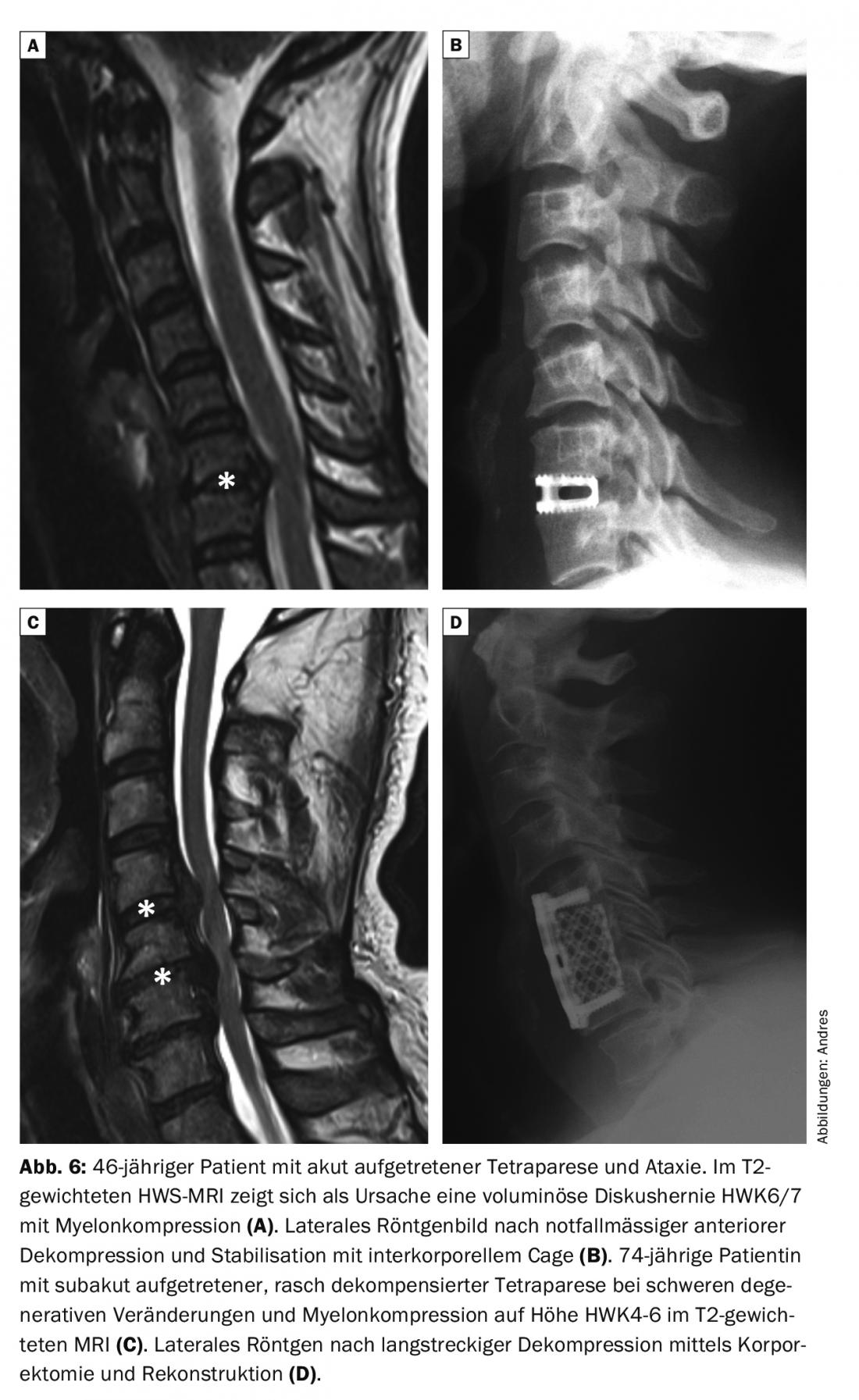
Degenerative changes of the spine are common, but overall rarely responsible for paraplegia. They are usually diagnosed and treated before high-grade spinal cord compression can occur. Nevertheless, for example, a large disc herniation with compression of the myelon (Fig. 6) or the cauda equina, as well as preexisting cervical spinal stenosis associated with trauma (Fig. 6), instability or a smaller disc herniation may acutely cause paraplegic symptoms. In elderly patients, paraplegic syndromes may be due to additional trauma, often mild, in the setting of a degeneratively narrowed cervical spinal canal without the presence of osseous lesions [9]. In these cases, which account for approximately 10% of all spinal cord injuries, the decision for conservative or surgical therapy must be individualized for each patient; evidence-based treatment algorithms do not exist [10]. Notably, the optimal timing for surgical intervention is also unclear, although isolated studies have demonstrated benefits of prompt decompression of neural structures [11]. Unfortunately, protracted and chronic courses are common in elderly patients.
Outlook
It is not yet possible to influence the damage to the myelon caused by compression or laceration by surgical intervention. This is where rehabilitation comes in, which has made significant progress over the last decade. In particular, the importance of early rehabilitation was recognized. The regenerative capacity and plasticity of the spinal cord are now the target of intensive research activity. Our understanding of the mechanisms that control repair processes in the central nervous system has improved greatly over the past 20 years. In particular, the nerve growth inhibitory protein Nogo-A and its receptor NgR1, but also other mechanisms, limit the regenerative capacity in the central nervous system. Several experimental approaches have been developed to overcome these limitations [12]. If it is possible to favorably influence the regenerative potential of the myelon after injury, this would significantly improve the prognosis for many patients. Another promising area of research involves stem cell therapy. Replacement of the defunct neurons and glial cells and functional recovery can be achieved by surgical transplantation of stem or progenitor cells of various origins such as human fetal tissue, genetically modified cell lines, and embryonic or somatic (adult) stem cells [13]. A recent multicenter study also in Switzerland with intramedullary transplantation of human multipotent neural stem cells in patients with cervical and thoracic spinal cord injuries demonstrated that this method is safe and can be performed without the risk of neurological deterioration, although long-term results are still pending [14]. In addition to basic research, translational research must also be further expanded in order to develop new, promising therapeutic methods for these severely impaired patients.
Take-Home-Message
- Surgical treatment for paraplegic lesions aims to microsurgically remove the compression of the neural structures that still exists in most cases and, if necessary, to restore the stability of the spine.
- Incomplete paraplegic lesions with residual compression, onset of paralysis after a free interval, ascending neurologic deficits, and unstable or open spinal injuries usually require surgical treatment.
- Surgical restoration of spinal stability and function is a prerequisite for rapid mobilization during subsequent rehabilitation.
Literature:
- Holtz A, Levy R: Spinal Cord Injury. Oxford University Press 2010; ISBN 978-0-19-970681-5.
- Fehlings MG, Tetreault LA, et al: A Clinical Practice Guideline for the Management of Acute Spinal Cord Injury: Introduction, Rationale, and Scope. Global Spine J 2017; 7(3 Suppl): 84S-94S.
- Kirshblum SC, Waring W, et al: Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011; 34(6): 547-554.
- Charles YP, Steib JP: Management of thoracolumbar spine fractures with neurologic disorder. Orthop Traumatol Surg Res 2015; 101(1 Suppl): S31-40.
- Mizuno J, Nakagawa H, et al: Clinicopathological study of “snake-eye appearance” in compressive myelopathy of the cervical spinal cord. J Neurosurg. 2003; 99(2 Suppl): 162-168.
- Hadley MN, Shank CD, et al: Guidelines for the Use of Electrophysiological Monitoring for Surgery of the Human Spinal Column and Spinal Cord. Neurosurgery 2017; 81(5): 713-732.
- Deletis V, Seidel K, et al: Intraoperative identification of the corticospinal tract and dorsal column of the spinal cord by electrical stimulation. J Neurol Neurosurg Psychiatry 2018; doi: 10.1136/jnnp-2017-317172 [Epub ahead of print].
- Dea N, Gokaslan Z, et al: Spine Oncology – Primary Spine Tumors. Neurosurgery 2017; 80(3S): 124-130.
- Weingarden SI, Graham PM, et al: Falls resulting in spinal cord injury: patterns and outcomes in an elderly population. Paraplegia 1989; 27: 423-427.
- Epstein NE, Hollingsworth R: Diagnosis and management of traumatic cervical central spinal cord injury: A review. Surg Neurol Int. 2015; 6(Suppl 4): 140-153.
- Fehlings MG et al: Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 2012; 7(2): e32037.
- Filli L, Schwab ME: The rocky road to translation in spinal cord repair. Ann Neurol 2012; 72(4): 491-501.
- Andres RH, Meyer M, et al: Restorative neuroscience: concepts and perspectives. Swiss Med Wkly 2008; 138(11-12): 155-172.
- Levi AD, Okonkwo DO, et al: Emerging safety of intramedullary transplantation of human neural stem cells in chronic cervical and thoracic spinal cord injury. Neurosurgery 2018; 82(4): 562-575.
InFo NEUROLOGY & PSYCHIATRY 2018; 16(3): 4-10.











