More and more people worldwide are becoming newly infected with STDs such as syphilis. Since symptoms disappear independently, the disease is often underestimated by patients. PD Dr. med. Clara Lehmann, medical director of the MVZ Infectiology (University of Cologne) informed about diagnostic possibilities and therapeutic approaches at the congress of the DGIM. First-line therapy is still penicillin.
A steady increase in new lues infections was reported by the European Centre for Disease Prevention and Control (ECDC) for Europe at the end of 2017. In 1493, Columbus’ ships had imported syphilis from the new continent to the old world. Today, the USA is also recording rising infection figures again. Since 2010, more and more people worldwide have become infected with the bacterium Treponema pallidum, the causative agent of syphilis.
The tricky thing about this venereal disease, which progresses in stages, is that symptoms disappear without treatment, but syphilis takes a chronic course if left untreated and can affect all organ systems, as PD Dr. med. Clara Lehmann, Medical Director of the MVZ Infectiology at the University of Cologne, explained.
Penicillin remains first-line therapy
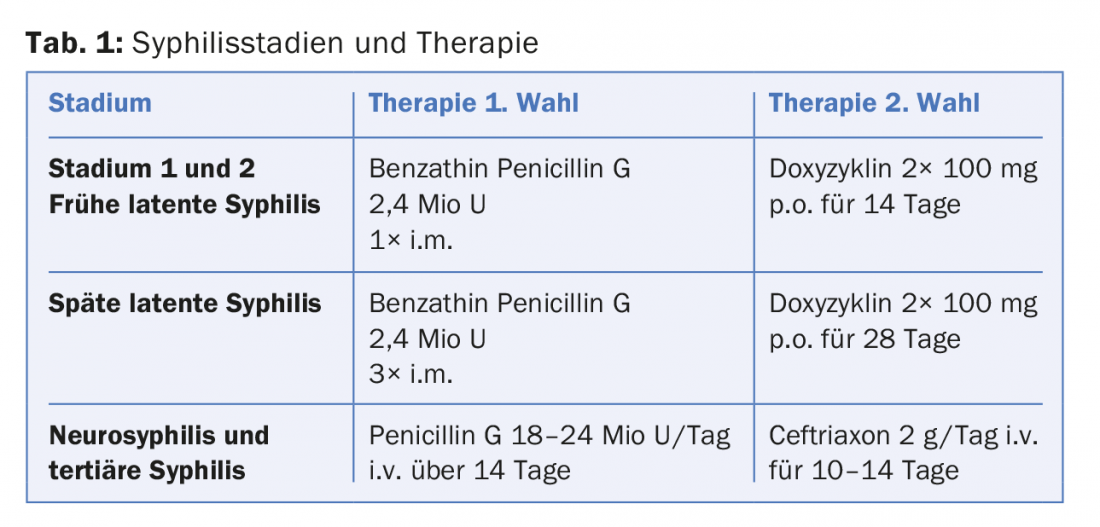
The good news beforehand: The disease can still be treated well with penicillin. A single intramuscular injection of benzylpenicillin-benzathine can cure a fresh infection. Late latent syphilis usually requires only three intramuscular penicillin injections at weekly intervals, whereas variants of neurosyphilis and tertiary forms require intravenous administration over 14 days. Here, ceftriaxone may also be considered as an alternative to penicillin (Table 1).
Infection through unprotected sex
Primary infection occurs through pathogen contact via minimal mucosal lesions. The greatest risk is faced by men who have sex with men. Men represent the largest patient population in Europe today; the proportion of infected women was only 6.2% in 2015. The currently observed increase in infections among homosexual men is explained by a higher willingness to engage in risky sexual behavior.
Effective therapy for HIV infection has caused the number of changing partners and the proportion of risky sexual contacts to rise again. HIV can now be treated so that the viral load is below the detection limit. This means that those affected can no longer infect their partner during unprotected sex, with the result that fewer condoms are used.
About three weeks after unprotected sex, a painless ulceration develops at the site of entry. The incubation period is comparatively long, with a doubling time of 30 hours, due to the slow growth of the spirochetes. A painless hard chancre (ulcus durum) occurs on the penis as a so-called primary effect. This heals without therapy within 3-8 weeks. It is usually accompanied by regional lymphadenitis. Because it is a painless lesion, sufferers do not always seek help, which is why it often goes unnoticed. Primary effects, however, may also manifest as infection in the mouth or anus.
Disseminated spirochete infection: the monkey of diseases
Although the initial immune response leads to spontaneous healing of the durum ulcer, the spread of the infection is not prevented without therapy: The pathogens spread unnoticed throughout the body. Several weeks to months after primary onset, generalized disease begins in about one-quarter of untreated patients. In this second stage, the disease manifests as macular or papular exanthema, also known as “keel measles.” It is a generalized, symmetrical rash on the trunk and extremities with pathognomonic involvement of the palmae and plantae. In addition, flat nodules form in skin folds.
Systemic symptoms such as fever, general malaise, headache, and myalgias occur as part of the hematogenous and lymphatic spread of the pathogens; inflammatory markers are often elevated as well. Persistent lymphadenopathy or enlarged, sometimes painful, inguinal lymph nodes may indicate syphilis. “These symptoms also disappear again spontaneously,” says Dr. Lehmann, “and those affected often don’t realize they have syphilis.” The highly variant clinical picture complicates the diagnosis. It is important to think of syphilis as a differential diagnosis and to examine sexual partners as well. However, latent infections are just as possible. In this case, only serology is positive before the disease turns into a chronic infection, he said. A prerequisite for contact infection (contagion) is the presence of treponemal lesions.
Clinical course: tertiary stage and neurosyphilis
The third stage, which can occur from about the third year after the (untreated) infection, is characterized by a cellular defense reaction with simultaneous pathogen depletion. Inflammatory granulomas (gums) on the skin and internal organs are characteristic of this phase of the disease. In the tertiary stage, destruction of one or more organs occurs in the worst case. In the cardiovascular system, vessels and valves may be affected, e.g. in the form of aortic insufficiency or aortic aneurysm.
Patients with neurosyphilis may present with typical symptoms of meningitis or be noted for meningovascular complications such as dementia (approximately 20 years after initial infection). Tabes dorsalis, formerly the most common form of neurosyphilis, is the result of degeneration of the posterior strands of the spinal cord; typical symptoms are pain shooting into the lower abdomen and legs (lancinating), as well as paresthesias and ataxia.
Diagnostics: Serology
A distinction is made between non-specific and specific test procedures. The non-specific VDRL (Venereal Disease Research Laboratory) test is based on the reaction of patient serum with a cardiolipin antigen. It becomes positive in the fifth week of illness and is suitable as a screening method as well as for follow-up. The RPR test (Rapid Plasma Reagin) is a rapid test. Both tests are markers of acute infection and are suitable for assessing the success of therapy. The TPHA test (Treponema pallidum hemagglutination test) serves as a specific test. This detects syphilis infection at any given time.
Source: 124. DGIM Congress, Old and New Plagues: Sexually Transmitted Diseases (STD), April 14-17, 2018, Mannheim, Germany.
Further reading:
- Clement ME, et al: Treatment of syphilis: a systematic review. JAMA 2014; 312(18): 1905-1917.
- Gandhi RT: Case records of the Massachusetts General Hospital. Case 40-2014. A 57-year-old man with inguinal pain, lymphadenopathy, and HIV infection. N Engl J Med 2014; 371(26): 2511-2520.
DERMATOLOGIE PRAXIS 2018; 28(3): 40-41











