Perioperative anemia, blood loss, and allogeneic blood transfusions are associated with increased postoperative morbidity and mortality and prolonged hospital stay. About 40% of patients undergoing major surgery are anemic. Target group-specific approaches are in demand.
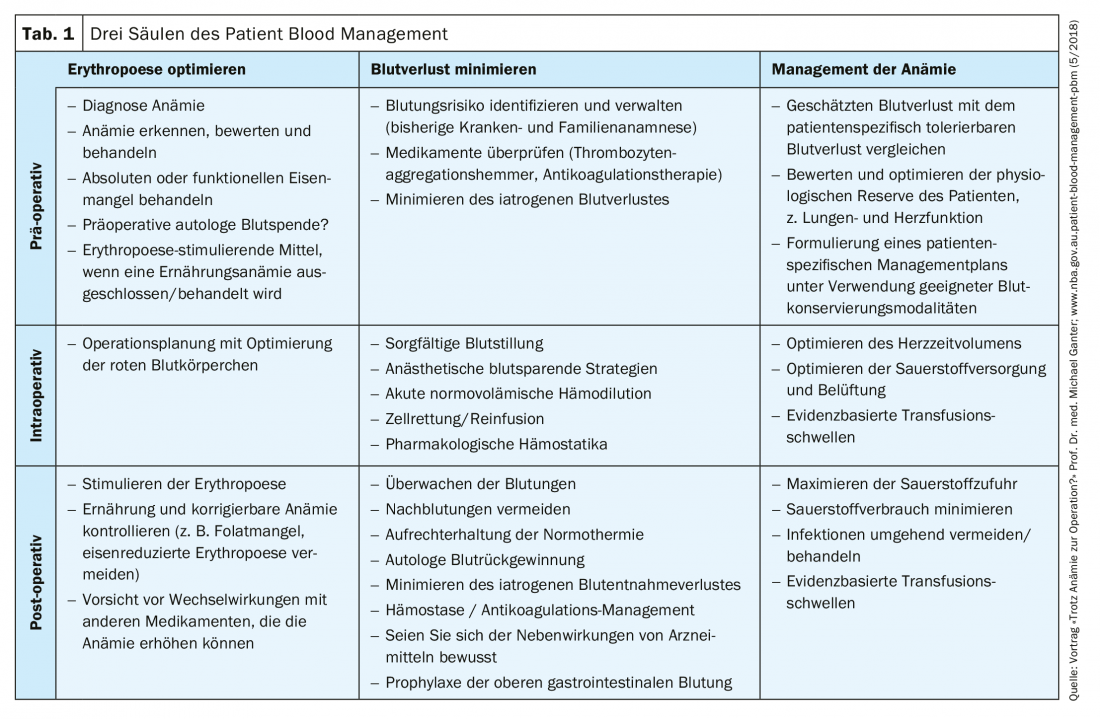
(Red) The importance of preoperative anemia is still underestimated, and its detection should lead to routine testing and treatment before elective surgery. Patient blood management (PBM) is a multimodal approach to address this problem. It focuses on three pillars: The detection and treatment of preoperative anemia; the reduction of preoperative blood loss; and the utilization and optimization of in individual physiologic reserve of anemia, including restrictive hemoglobin transfusion triggers (Table 1) . Patients undergoing major surgery (potential blood loss >500 ml), should be optimized if their hemoglobin concentration at screening is below 130 g/l. Evidence of anemia should be obtained as soon as possible after listing the surgeries – at least 14 days before surgery, ideally more than 30 days before – to allow sufficient time for optimization (Fig. 1). The most common cause of preoperative anemia is iron deficiency, which can be treated with iron therapy.
This is where the primary care physician comes in: laboratory tests to detect and diagnose anemia can be performed immediately after the decision to perform surgery is made in primary care. When anemia is discovered and treated, good communication between the general practitioner and the surgical team is critical to provide timely and effective treatment. Treatment of iron deficiency anemia should be performed with iron supplementation. If the interval between examination and surgery is > 6 weeks, oral iron treatment may be considered. However, gastrointestinal side effects may result in poor adherence to oral iron treatment. In practice, it is recommended to monitor the effectiveness of oral iron after four weeks of treatment. Intravenous iron is indicated when oral iron is poorly tolerated, ineffective (no increase in hemoglobin after 4 weeks), when time to surgery is insufficient, or when functional iron deficiency is present.
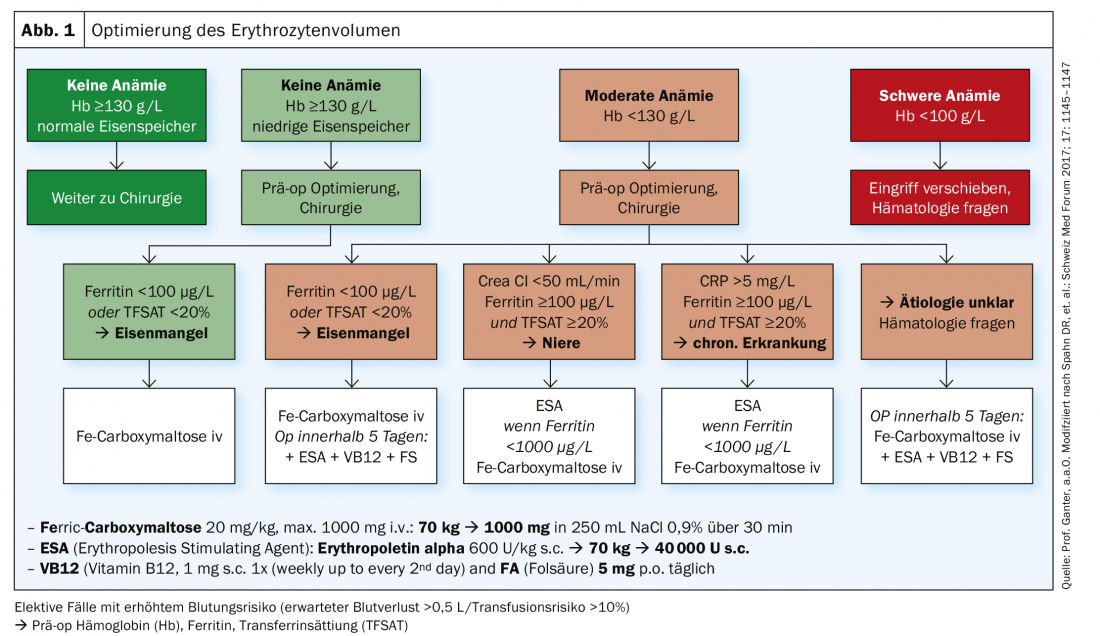
Caveat for iv supplementation: patients must be monitored (oxygen saturation, heart rate and non-invasive blood pressure) for 30 minutes afterwards during an iron infusion (which takes 15-30 minutes)! Resuscitation equipment and trained personnel should be available.
Iron deficiency anemia has a complex origin, including nutrient deficiency and a chronic inflammatory state leading to absolute iron deficiency, functional iron deficiency, or iron deposition. Absolute iron deficiency is a condition in which iron stores are severely reduced, resulting in anemia. Functional iron deficiency, on the other hand, refers to inadequate iron mobilization despite normal or elevated iron stores. An important role in iron binding is played by inflammation, in which upregulation of hepcidin, a hormone produced in the liver that is regulated by iron stores and erythropoietic activity, inhibits intestinal iron absorption and increases iron binding in liver and macrophages, also known as anemia in chronic disease. Hepcidin thus prevents absorption of dietary iron from the gastrointestinal tract, resulting in iron-restricted erythropoiesis and functional iron deficiency. Such a condition is the most common cause of anemia in patients undergoing cardiac surgery. In general, chronic diseases, inflammatory diseases, and malignancies are common triggers of functional iron deficiency in surgical patients. Functional iron deficiency is the most common cause of anemia in chronic disease and occurs in approximately 50 percent of anemic surgical patients.
Source: Iron Academy 2019
HAUSARZT PRAXIS 2019; 14(6): 18-20 (published 5/24/19, ahead of print).