Overloading or incorrect loading, as well as wear and tear, can acutely affect the tendon or the tendon attachment. As a result, loss of function and pain occur. If tendinopathy is left untreated, it can lead to postural deformity and joint wear. In addition to pain relief, therapy goals include promoting tissue regeneration and restoring resilience. A wide range of conservative treatment options can be used.
Tendinopathies refer to painful and functionally restricted tendon structures with the potential risk of tendon rupture. “Jumper’s knee” often affects jump athletes, results from overuse of the patellar tendon, and leads to stress pain at the front of the knee. Other common locations of tendinopathy include rotator cuff, lateral elbow, and Achilles tendon. The diagnosis is primarily clinical with typical palpitations. In terms of imaging techniques, ultrasound is the gold standard. However, if there are indications of structural damage, a supplementary X-ray or MRI examination may be useful, said Harald Leemann, MD, senior physician and co-head of sports medicine, Zug Cantonal Hospital, on the occasion of the continuing education days of the College of Family Medicine [1].
Tendinopathy as a non-inflammatory tendon disease
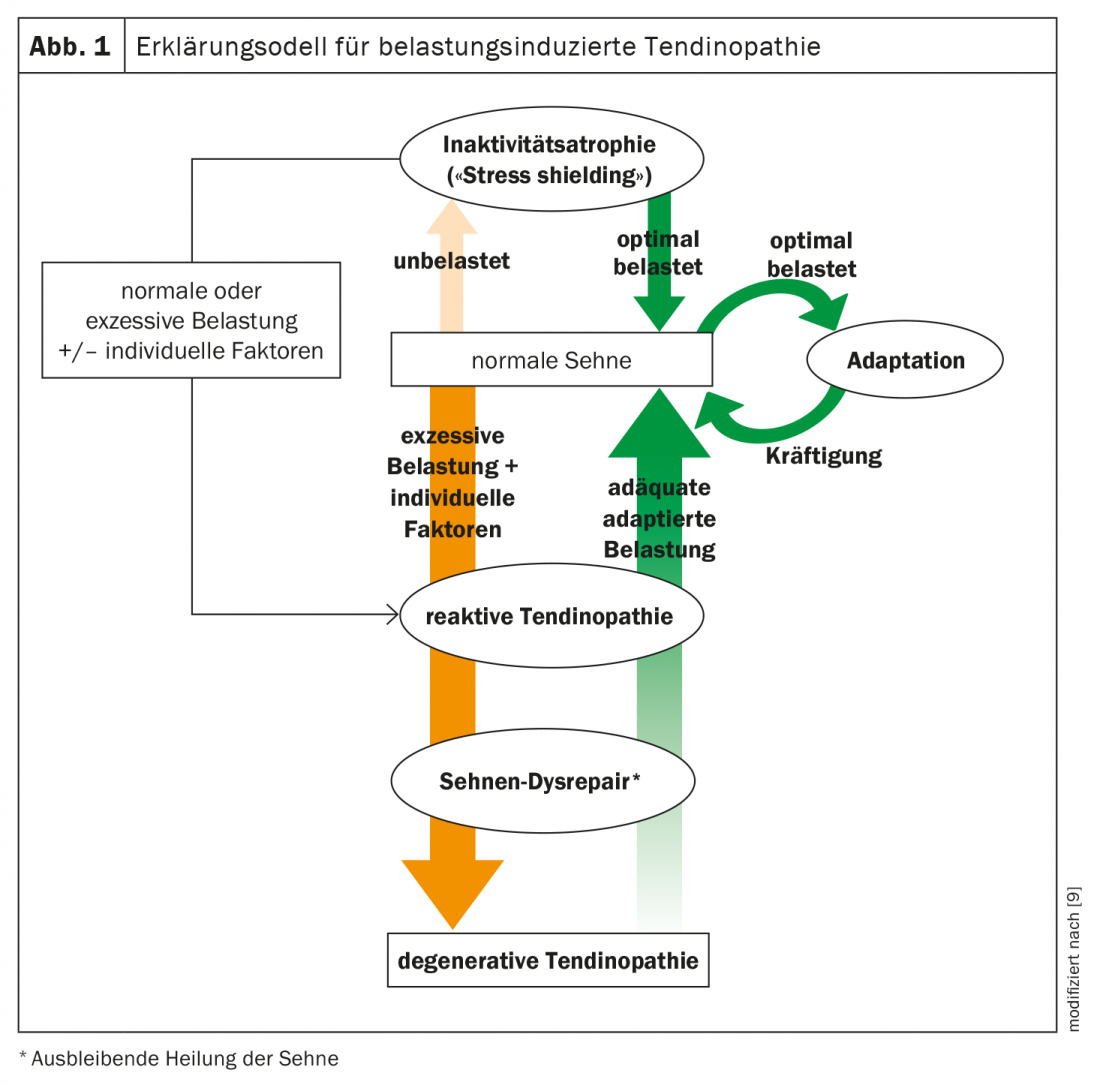
Whereas the clinical picture used to be understood as a classic inflammatory reaction, the current understanding is that it is a non-inflammatory tendon disease caused by overload, incorrect loading and degenerative processes (Fig. 1) [2]. Tendons transmit the forces generated by the muscle to the skeleton and thus contribute to different movement performances. Repetitive microtrauma can lead to degenerative tears in the tendon by exceeding the tensile and extensile stress limits [3]. An increase in muscle strength, for example as a result of training, must be accompanied by adequate adaptation of the tendon so that the tendon tissue is not affected by excessive stress due to the stretching that occurs [4]. The severity of the disease is primarily determined by when pain occurs. In mild tendinopathy, pain occurs each time a specific activity is completed. If it is a severe tendon disease, the pain occurs at the beginning, during and after the end of activities.
Conservative treatment options for tendinopathies
In the case of tendinopathy, complete unloading and immobilization of the tendon or joint is not indicated. Adequate loading is important, the speaker emphasizes: “A tendon needs loading. The tendon does not like to have pressure, but it likes to have tension,” says Dr. Leemann. However, overloading must be avoided, as the tendons react to this with structural maladaptations. In addition to treatment with analgesics and physiotherapy, extracoporeal shock wave therapy is increasingly being used to treat tendinopathies. In general, the therapy of tendinopathies should be adapted to the individual complaints.
The conservative treatment measures recommended by the Society for Orthopedic Traumatologic Sports Medicine include the following therapeutic pillars [5]:
Addressing triggering factors: The first step is to identify the triggers of tendinopathy. Intrinsic factors include endocrine disease, anthropometric measures (BMI, hip-waist index), axial deviations (e.g., valgus deformity), movement-related errors. Extrinsic factors include changing flooring, equipment (footwear), medications (e.g., fluoroquinolones, statins, glucocorticoids).
Symptomatic Acute Therapy: In symptomatic acute therapy, switching from a ‘high impact’ sport to a less stressful form of exercise is an option. Whereby this is rather difficult with top athletes. In these cases, load modification is appropriate. Local antiphlogistic measures (e.g. cooling) act as a third option for symptomatic acute treatment.
Interventional therapy/injection therapy: In addition to sclerotherapy, this also includes glucocorticoids and PRP (“Platelet-Rich Plasma”). However, the speaker advises against corticosteroid infiltrations. He said there is evidence of a short-term effect of up to three months, but in the medium and longer term, a deterioration in condition may occur. This is one of the findings of a study published in the Clinical Journal of Sport Medicine [6]. “Cortisone does not belong in and around tendons,” summarizes the speaker. With regard to PRP, the problem is that it is not currently covered by health insurance and people are often unwilling to spend money on it. PRP is the peritendinous application of platelet-rich plasma centrifugate of the patient’s own blood. By secreting pro-inflammatory substances and growth factors, thrombocytic α-granules can promote local regeneration processes [10].
Drug therapy: Regarding drug treatment, NSAIDs are often used in the short term. NSAIDs (e.g., ibuprofen or diclofenac) taken over the course of a few days can help relieve pain and improve function. However, prolonged use of oral NSAIDs is not advisable because of the usually absent local inflammation and potential side effects [3]. Other drugs available include Traumeel® or glycerol nitrates [7].
Physical therapy: Among physical therapies, therapeutic ultrasound and shock wave therapy are particularly recommended. Shock wave therapy alters the environment of the treated tissue and can promote regeneration by releasing mediators that promote healing and bone-building factors [8].
Physiotherapy: From the field of classical physiotherapy, manual therapy, training therapy, fascia release techniques and eccentric training can be applied. Fasciae are connective tissue structures that hold other structures of the body together and are important for stability. Through fascia therapy, fascia can be loosened, providing pain relief as well as improved mobility.
Technical care: As another pillar of conservative treatment options, technical care measures are available such as orthoses or shoe inserts.
Congress: College of Family Medicine 2021
Literature:
- Leemann H: Sports Medicine, Harald Leemann, MD, College of Family Medicine Continuing Education Days, June 24-25, 2021.
- Strengthening Healthy Tissue – Tendinopathies of the Lower Extremity, physiopraxis 18(11/12)/2020, www.thieme.de/de/physiotherapie/gesundes-gewebe-kraeftigen-tendinopathien-der-unteren-extremitaet-162568.htm, last accessed Aug. 19, 2021.
- Voss P, Kyburz D: Tendinopathies and insertional tendinopathies. the informed physician _05_2018, 16-19. www.tellmed.ch, last call 19.8.2021
- Bohm S, Mersmann F, Arampatzis A : Functional adaptation of connective tissue by training. Dtsch Z Sportmed. 2019; 70: 105-110, www.zeitschrift-sportmedizin.de/funktionelle-anpassung-von-sehnen/
- GOTS Expert Meeting: Muscle and Tendon Injuries 2016, www.gots.org/expertenmeeting-muskel-und-sehnenverletzungen
- Hart L: Corticosteroid and other injections in the management of tendinopathies: a review. Clin J Sport Med 2011; 21(6): 540-541
- Drug Information, www.swissmedicinfo.ch, last accessed 8/19/2021.
- Gelenk-klinik-en, https://gelenk-klinik.de/konservativ/stosswellentherapie.html, last accessed 19.8.2021
- Cook JL, Purdam CR: Istendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathyBritish Journal of Sports Medicine 2009; 43: 409-416.
- Miller LE, et al: Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: systematic review and meta-analysis of randomised injection-controlled trials. BMJ Open Sport Exerc Med 2017; 3: e000237.
HAUSARZT PRAXIS 2021; 16(9): 24-25 (published 9/18-21, ahead of print).