Studies have shown that early detection and treatment significantly improves the prognosis of psychotic disorder. Therefore, if psychotic development is suspected, early consultation with specialists is important.
Two case studies from the early intervention consultation at the Clinic for Child and Adolescent Psychiatry and Psychotherapy (KJPP) in Zurich:
14-year-old Senja reports a distinct fantasy world that she created for herself about five years ago and to which she repeatedly retreats in her free time. Increasingly, Senja seems to lose control over her fantasy world. It seems to her as if certain sinister figures from that world suddenly appear in the real world and haunt her. Sometimes she hears voices. In addition, Senja suffers from changes in her affect, such as depressive mood swings, severe lack of energy, and lack of emotion. In addition, she reports problems with concentration. She used to have no problem meeting school requirements, but now she struggles. She is described as very absent and unfocused. Time and again Senja is absent from class without excuse. She withdraws from her classmates. She is increasingly distrustful of her friends and feels that she can no longer trust them. She spends more and more time in her room, preoccupied with her fantasy world. Senja is registered by the treating therapist in the early detection consultation.
After a stressful period, 15-year-old Jonas has increasingly severe problems falling asleep until he can barely sleep. At night, the parents hear him walking around the apartment. He is no longer able to concentrate. In logical thinking Jonas shows himself incoherent, prolix, logorrheic and disorganized. He reports paranoid delusions. For example, he had the feeling that the family doctor had stolen his laptop. Once, convinced that he was sleeping in the wrong room, he had wanted to move all the furniture to another room in the middle of the night. In affect, he shows himself to be unstable and inconsistent. He cries, laughs and is verbally aggressive. The parents can hardly leave him alone. After being examined by the doctors at the Children’s Hospital, he was referred to the emergency service of the KJPP with the suspicion of acute onset psychosis.
Early detection and treatment of psychotic disorders in adolescence has gained importance in recent years. Early detection and specific treatment of (pre)psychotic symptomatology has been shown to be an important intervention to minimize the negative consequences of the disorder. Although most psychoses manifest in young adulthood, the first subtle changes in perception, thinking or mood usually occur in childhood and adolescence. These changes are called At Risk symptoms.
At Risk symptoms do not yet have the quality of psychotic symptoms, but may already have their own illness value. Several clinicians and researchers have argued that even At Risk symptoms should be treated, regardless of the rate of transition to psychotic illness, because the level of distress is sufficient to warrant treatment [1–4]. Thus, adolescents in the At Risk stage may be impaired in their psychological, cognitive, and psychosocial development without meeting the criteria for psychosis. Early intervention centers for psychosis have emerged worldwide in recent years [5].
From clarification to indication for treatment
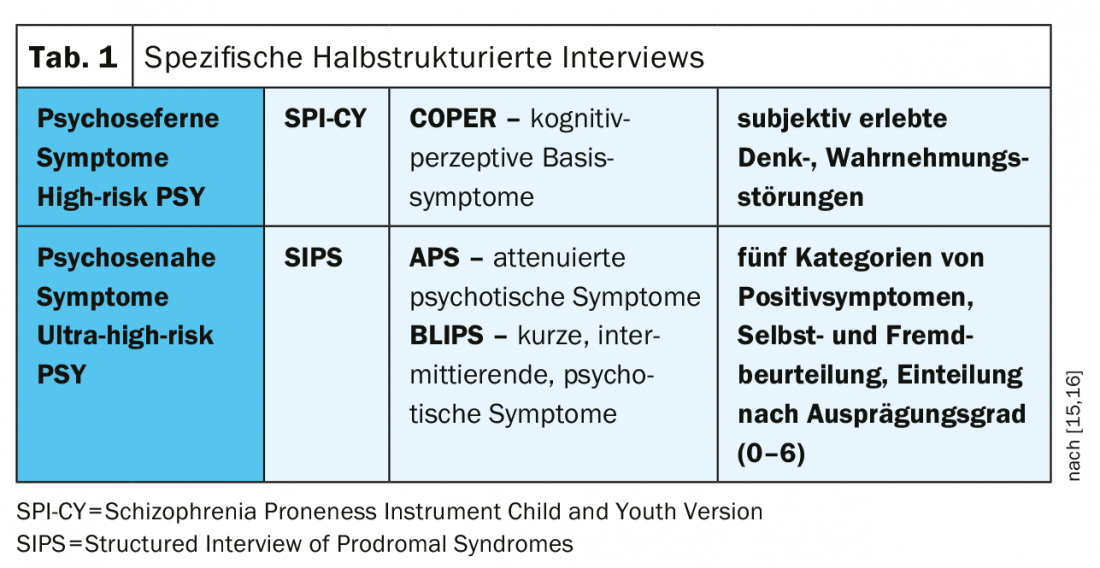
A specific diagnosis using semi-structured clinical interviews allows a qualitative and quantitative assessment of the symptomatology (tab. 1). Using these instruments, it is possible to determine whether the adolescents are still in the risk zone or whether the transition to psychosis has already occurred. In addition, it is important to assess comorbid disorders and rule out potential somatic causes.
Senja meets an Ultra High Risk (UHR) for developing psychosis due to her perceptual alterations (pseudo-hallucinations that she recognizes as not real), marked fantasy with magical thinking, and increased suspicion. All symptoms are rated as At-Risk symptoms because Senja is still able to do reality checks. In the test examinations she does not show any cognitive decline, nevertheless she experiences herself as clearly less concentrated and hardly able to learn. To this end, she meets the criteria for a moderate depressive episode.
In Jonas’ case, the connection to reality is no longer intact. He exhibits delusions and is significantly impaired in cognitions. After ruling out an organic cause, a diagnosis of acute psychotic disorder is made.
Psychosis treatment
In first-time sufferers, the focus is on symptomatic therapy. In most cases, antipsychotic pharmacotherapy is inevitable. The psychotic symptoms should be reduced and the patient’s ability to function should be restored. The goal is to rebuild reality control. The inpatient setting can provide the needed protected setting and professional treatment; at the same time, in a psychotic state, an acute inpatient admission can be experienced as traumatic. That’s why it’s important to work with family members to make the best possible decision for patients. However, in the case of danger to self or others or decompensation of the family system, emergency admission cannot be avoided.
At Risk symptoms focus on psychoeducation, symptom-focused psychotherapy, and treatment of comorbid disorders. More information can be found in EPA’s guidelines for early treatment of At Risk symptoms [4].
Drug treatment
Primarily, third-generation (aripiprazole) or second-generation (e.g., quetiapine) antipsychotics should be chosen as drug treatment: With comparable antipsychotic efficacy, they are better tolerated in terms of side effect profile than those of the first generation [6]. During the first week of treatment, when antipsychotic effects have not yet been achieved, adjunctive medication with benzodiazepines is helpful in reducing anxiety and tension. Children and adolescents may react more strongly than adults with adverse effects, therefore the initial dose should be increased slowly and taken in several doses per day to avoid concentration peaks. Typical initial adverse effects include fatigue, loss of concentration, and orthostatic disturbances. In addition, there may be a temporary increase in transaminase and alkaline phosphatase due to possible swelling of the epithelial cells of the bile duct during the first weeks of treatment. If there is little improvement after two weeks of treatment, switching to another antipsychotic is recommended because no improvement in symptoms is expected [7]. The duration of medication is based on recommendations for adults (at least one year for a first psychotic episode).
Psychotherapy
In psychotherapy for psychosis, individualized, resource-oriented interventions using behavioral therapy and systemic approaches, as well as psychoeducational family interventions, have been particularly effective [8–10]. Age-appropriate treatment services are essential to engage patients in longer-term therapeutic treatment.
The treatment of At Risk symptoms and psychoses of childhood and adolescence is multimodal and characterized by a strong networking of the help system. It must not only be based on the symptoms, but must also take into account the age-specific developmental tasks and address the individual difficulties of the respective patients. Children and adolescents often suffer massive social breakdowns as a result of psychosis, so that their normal further development is jeopardized. Coping skills in terms of stress management skills, problem solving skills and social skills are to be trained and improved. In addition to positive symptoms, it is important to recognize and treat negative symptoms such as listlessness, anhedonia or apathy, and cognitive decline as such.
Therapy manual for adolescents at increased risk of psychosis
Especially in adolescence, At Risk symptoms are common and lead to losses in functional level [11]. Unfortunately, the effectiveness of early interventions in child and adolescent psychiatry has been understudied, in part due to the lack of age-appropriate treatment manuals and the paucity of studies conducted in this age group to date. Thus, only three controlled trials of treatment interventions with adolescent At Risk patients could be included for the meta-analysis by Schmidt and her colleagues [4] [12–14].
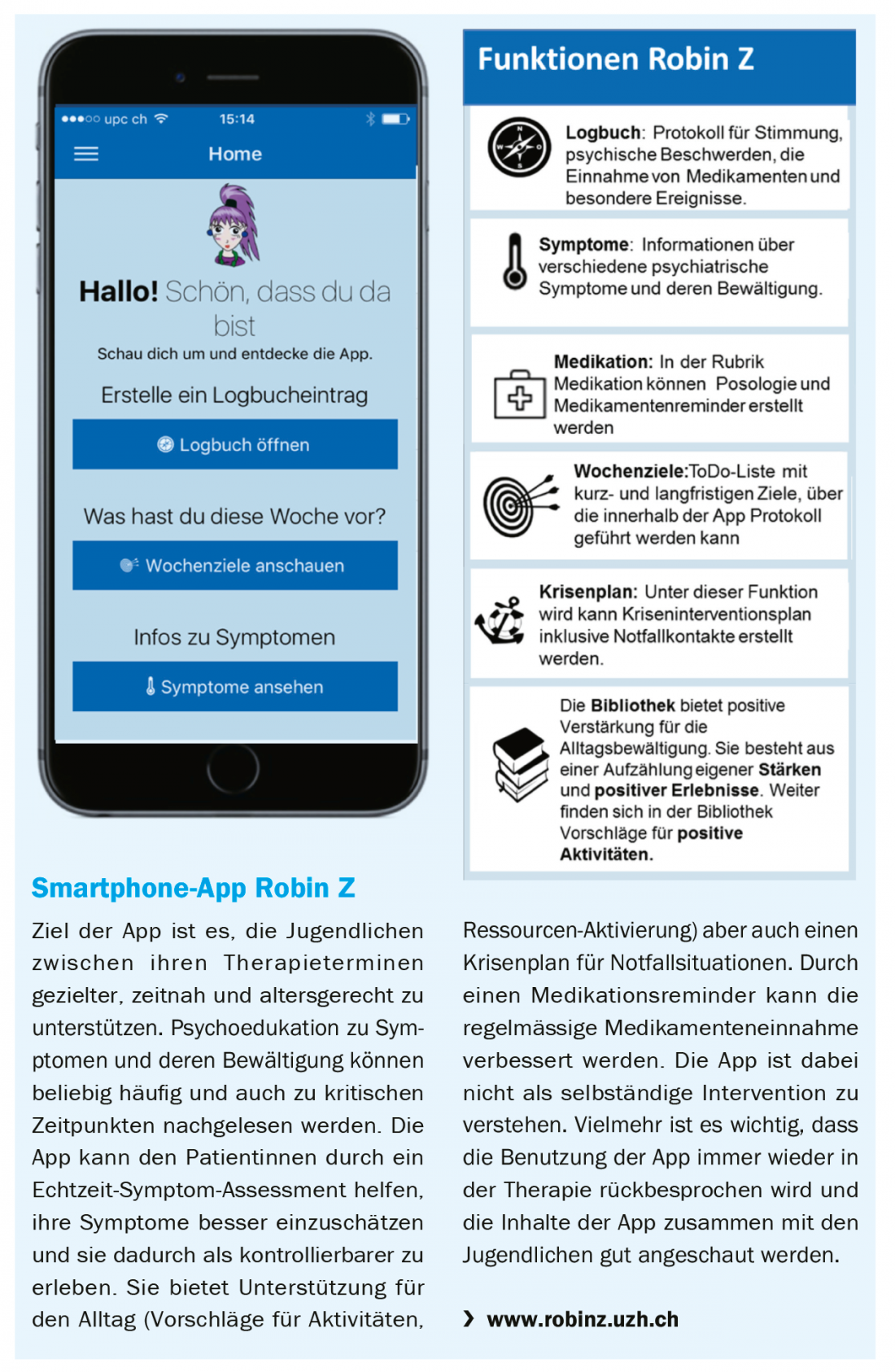
As part of the early psychosis consultation at the Department of Child and Adolescent Psychiatry and Psychotherapy, a treatment program for at-risk patients has been developed in recent years with age-appropriate interventions based on methods previously found to be effective for adults. The therapy program consists of a therapy manual and an app (box) for adolescent female patients. The effectiveness of the therapy program is currently being evaluated as part of a clinical intervention study.
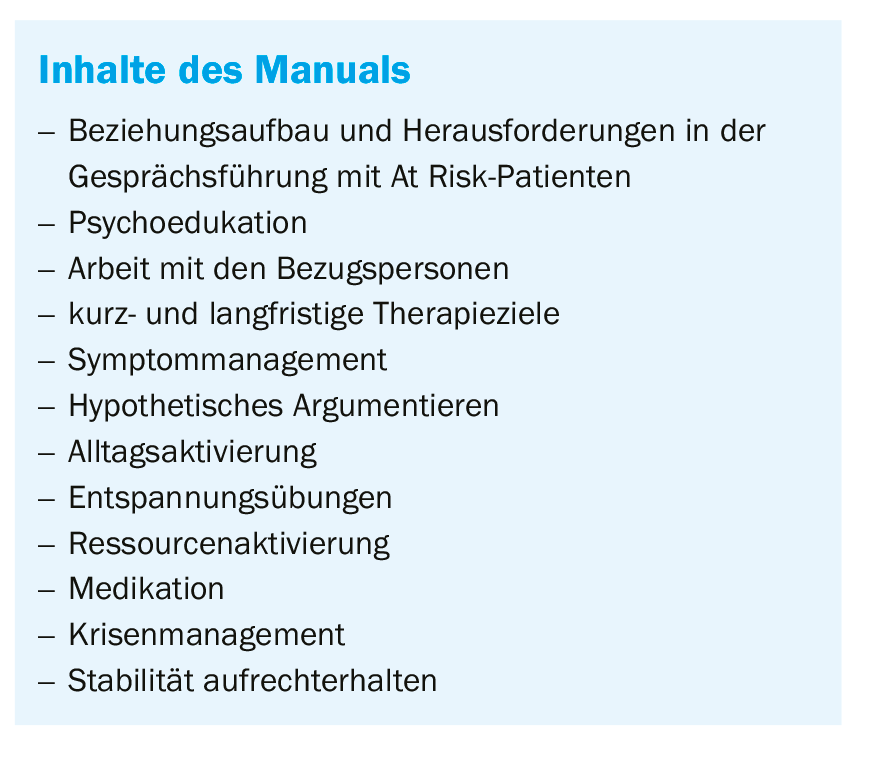
The manual is based on the recommendations of the European Guidelines of the European Psychiatric Association EPA for therapeutic interventions in at-risk patients [4] (overview) . It was written on the basis of cognitive behavioral therapy, solution-focused therapy and systemic therapy approaches. This is an individualized approach, and it is at the discretion of the therapeutic professional which of the individual modules to prioritize for each patient.
Group therapy
In addition to individual therapy, a group setting can be an important support for adolescents. Dialectical Behavioral Training for the Prevention of Mental Disorders (DBT 2P) is offered to adolescents with At Risk symptoms as well as first time sufferers at the Early Intervention Clinic in Zurich. The group training will discuss how to deal with the risk symptoms and psychotic symptoms. In an exchange between therapists and affected persons, the adolescents can receive helpful input regarding symptom management and coping with everyday life. In addition, social skills, dealing with stress, self-activation in everyday life and the promotion of self-confidence are important components of the group training.
Cognitive Remediation
In addition to improved management of positive and negative symptomatology, improvement of impaired cognitive function should be sought. To this end, a cognitive training plan is drawn up after individual cognitive deficits have been assessed. In this process, the individual cognitive areas in which difficulties exist are trained with computer-assisted training. The transfer of the training contents into everyday life should be accompanied by a specialist. In addition, strategies can be developed to compensate for the losses in everyday life (e.g. with regard to attention, executive functions, problem-solving skills).
Senja receives psychotherapeutic treatment during one year. Monthly family meetings are held. At the beginning of treatment, the focus is on dealing with At Risk symptoms. While Senja initially withdraws strongly into her world, she is able to detach herself better from her fantasy world in the course of therapy. At Risk symptoms have declined, and the focus of treatment is now on issues such as self-worth, finding identity, and the process of detachment from the nuclear family. Senja participates in group therapy despite initial resistance. Interactions with peers help her become more confident about her social skills. In this way, she is able to question her distrustful thought patterns more and more in the exchange in the group and reduces her distrust of others. She is dating more often again and investing in her friendships.
For Jonas, an inpatient admission seems necessary initially. However, the family wants to try outpatient first and the parents agree to provide the son’s increased care needs. The mother takes a leave of absence from work and the father reduces his workload. Regular appointments are held twice a week in the outpatient setting. Treatment with aripiprazole and lorazepam can counteract the severity of the symptoms. In executive functions and concentration Jonas still shows cognitive losses, he regularly attends the cognitive training and shows first small progress. With sufficient stabilization of the symptomatology, reduced school attendance now succeeds well; contact with peers is very important to him and contributes to a sense of normality.
Take-Home Messages
- Studies have shown that early detection and treatment significantly improves the prognosis of psychotic disorder. Therefore, if psychotic development is suspected, early consultation with specialists is important.
- In first-time sufferers, the focus is on symptomatic therapy. Drug treatment with antipsychotics is usually necessary.
- Psychotherapy is recommended for At Risk symptoms with a focus on psychoeducation, symptom management, and comorbid disorders.
- Age-appropriate treatment programs that address the specific needs of adolescents are important in motivating young sufferers to seek therapy.
Literature:
- Bertolote J, McGorry P: Early intervention and recovery for young people with early psychosis: consensus statement. Br J Psychiatry Suppl 2005; 48: s116-119.
- Correll CU, et al: Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol Psychiatry 2010; 51(4): 390-431.
- Fusar-Poli P, et al: Lessons learned from the psychosis high-risk state: toward a general staging model of prodromal intervention. Psychol Med 2014; 44(1): 17-24.
- Schmidt SJ, et al: EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry 2015; 30(3): 388-404.
- Maric NP, et al: Survey of the European Psychiatric Association on the European status and perspectives in early detection and intervention in at-risk mental state and first-episode psychosis. Early Interv Psychiatry 2018; doi: 10.1111/eip.12682. [Epub ahead of print]
- Pagsberg, AK, et al: Early Non-response to Antipsychotic Medication in Adolescents with First-episode Psychosis is a Reliable Predictor of Ultimate Non-response and Non-remission: Results from the 12-week TEA Trial. In: Early Intervention In Psychiatry 1999; 12: 88.
- Myrto, et al. 2015 [exakte Q-Beschreibung fehlt]
- Armando M, Pontillo M, Vicari S: Psychosocial interventions for very early and early-onset schizophrenia: a review of treatment efficacy. Curr Opin Psychiatry 2015; 28(4): 312-323.
- Baker K, Howell C, Findling RL: Current Treatment Trends of Psychosis in Youth with Schizophrenia. Curr Opin Psychiatry 2016; 3(1): 1-14.
- Pinquart M, Oslejsek B, Teubert D: Efficacy of systemic therapy on adults with mental disorders: A meta-analysis. Psychother Res 2016; 26(2): 241-257.
- Velthorst E, et al: Potentially important periods of change in the development of social and role functioning in youth at clinical high risk for psychosis. Dev Psychopathol 2018; 30(1): 39-47.
- Bechdolf A, et al: Preventing progression to first-episode psychosis in early initial prodromal states. Br J Psychiatry 2012; 200(1): 22-29.
- McGorry PD, et al: Randomized controlled trial of interventions for young people at ultra-high risk of psychosis: Twelve-month outcome. J Clin Psychiatry 2013; 74(4): 349-356.
- Miklowitz DJ, et al: Family-Focused Treatment for Adolescents and Young Adults at High Risk for Psychosis: Results of a Randomized Trial. J Am Acad Child Adolesc Psychiatry 2014; 53(8): 848-858.
- Schultze-Lutter F, Koch E: Schizophrenia Proneness Instrument, Child and Youth Version (SPI-CY). Rome: Giovanni Fioriti Editore, 2010.
- Miller TJ, et al: Prodromal Assessment with the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive Validity, Interrater Reliability, and Training to Reliability. Schizophrenia Bulletin 2003; 29(4): 703-715.
InFo NEUROLOGY & PSYCHIATRY 2019; 17 (3): 8-12.











