Many patients complain of persistent symptoms after they have recovered from SARS-CoV-2 infection. In such cases, the first path usually leads to the family doctor, but the armamentarium available to the general practitioner does not always lead to a clear diagnosis. Which patients should receive further pulmonary diagnostics – and especially when?
The first 8 weeks after infection can still be counted as the acute phase without any problems; during this period, apart from the possibility of thromboembolic events, there is no need to worry much about complications, said Prof. Dr. Thomas Bahmer, a pulmonologist at the Schleswig-Holstein University Hospital, Kiel Campus (D). If symptoms persist after 2-3 months, performance is impaired, and the primary care physician’s examination with laboratory and ECG does not provide clarity, then diffusion capacity and body plethysmography are the next step. Thereafter, a review should be performed to determine what type of imaging and further diagnostics are indicated.
The most important markers that can be used to assess the severity of illness and progression of SARS-CoV-2 infection are, first, of course, the number, type, and severity of symptoms, the need for hospitalization, oxygen therapy, and the type of treatment. But also the question of existing pre-existing conditions and medication must be considered. “What helps and I definitely recommend is the use of structured questionnaires to elicit symptomatology,” explained Prof. Dr. Bahmer (Tab. 1). In addition, from a pneumological point of view, the findings of other practitioners should always be taken into account if the patient has previously been seen by a general practitioner, cardiologist or ENT specialist, and in rarer cases also by a neurologist or psychiatrist.

One year tracking
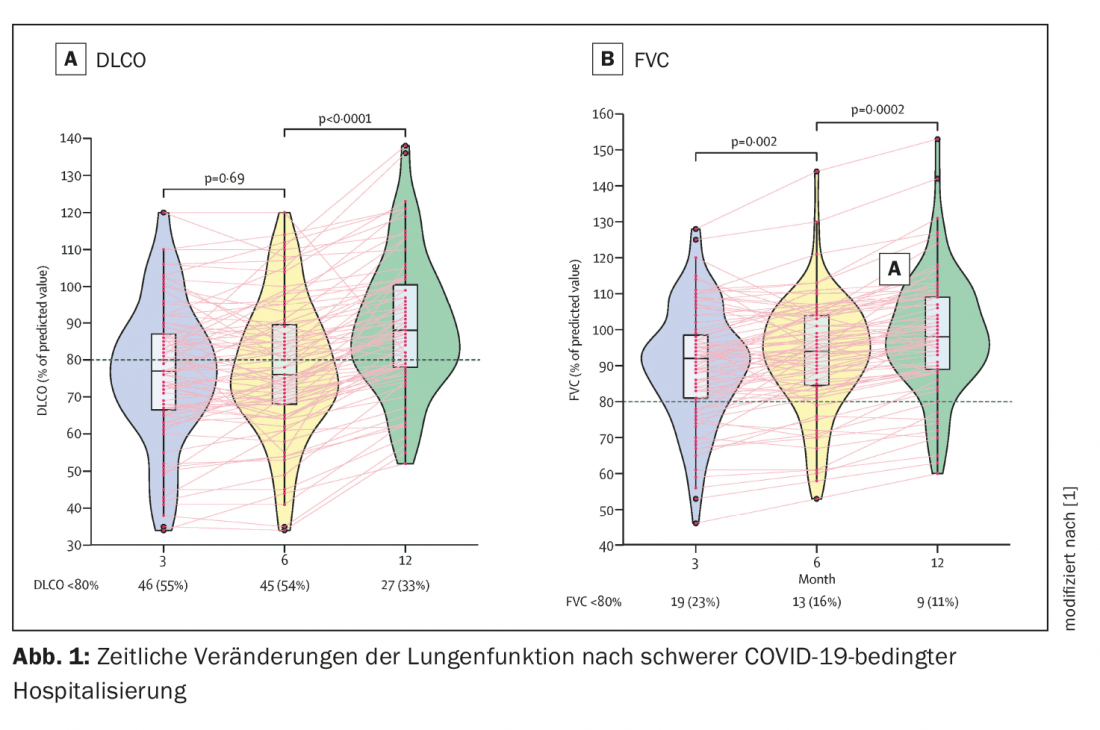
The physician presented a Chinese study that included 83 patients (57% male, 43% female) aged 52-66 years from a hospital in Wuhan. The proportion of nasal oxygen vs. HFNC or NIV was 45% vs. 55%, and none received steroid therapy in the acute phase. They all underwent severe acute illness with respiratory rate >30/min,SpO2 <94% at rest, pO2/FiO2 <300 mmHg, and image morphologically a 50% progression within 24-48 hours.
Concomitant or complicating risk factors were excluded, that is, patients were hospitalized and received oxygen administration but had not been ventilated and had no preexisting conditions such as arterial hypertension, diabetes, cancer, or chronic lung disease. They were also exclusively non-smokers.
For one year, this population was followed up with both CT and pulmonary function and questionnaires. Evaluation of lung function showed that it can take up to one year for diffusion capacity to return to the normal range. One-third of patients still had a DLCO of less than 80% at 12 months. “The first 6 months remained relatively unchanged, only then was there a leap toward normalization,” said Prof. Bahmer (Fig. 1). In the case of forced vital capacity (FVC), 11% were also still suffering from limitations after one year. The 6-minute walk test and mMRC also show similar patterns.
After 9-12 months mostly improvement
Among patients who still have diffusion gas restriction at 12 months, women are more likely to be affected, but this appears to be the only risk factor for persistent restriction. Most patients also show improvement in CT findings after 9-12 months. Residual symptoms are mainly milk glass changes (24%), rarely septal thickening (5%), reticular drawing proliferation (4%) or subpleural compaction (1%). After a year, even more of those patients and the after-effects who had already shown a more severe course of the disease in the acute phase generally suffered, the expert said.
The Hamburg City Health Study [2] also considered patients with mild courses, more than 90% of whom had a non-hospitalized course. Here, although the data 9-10 months after SARS-CoV-2 infection show minimal changes in functional values (total lung capacity somewhat reduced, airway resistance somewhat increased), the results, although statistically significantly different, were for the most part within the normal range.
|
Procedure for post-COVID
|
Treatment Pathways
The S1 guideline Post-COVID/Long-COVID [3] recommends pneumologic care for dyspnea, thoracic symptoms, and persistent cough. In any case, diffusion gas measurement should be performed, as well as forced spirometry and body plethysmography at rest. Under stress, the 6-minute walk test and spiroergometry should be used. In imaging, whether chest X-ray is sufficient or CT needs to be done depends on the diffusion gas measurement or D-dimers. In addition, a screening polygraph is suggested. Nonspecific provocation testing, if needed, can address the question of whether one is dealing with post-infectious hyperresponsiveness.
Post-infectious cough is known to often respond well to inhaled corticosteroids. High FeNO levels are considered indicators of a good response to ICS. No hyperresponsiveness and low FeNO conversely indicate that ICS are not effective.
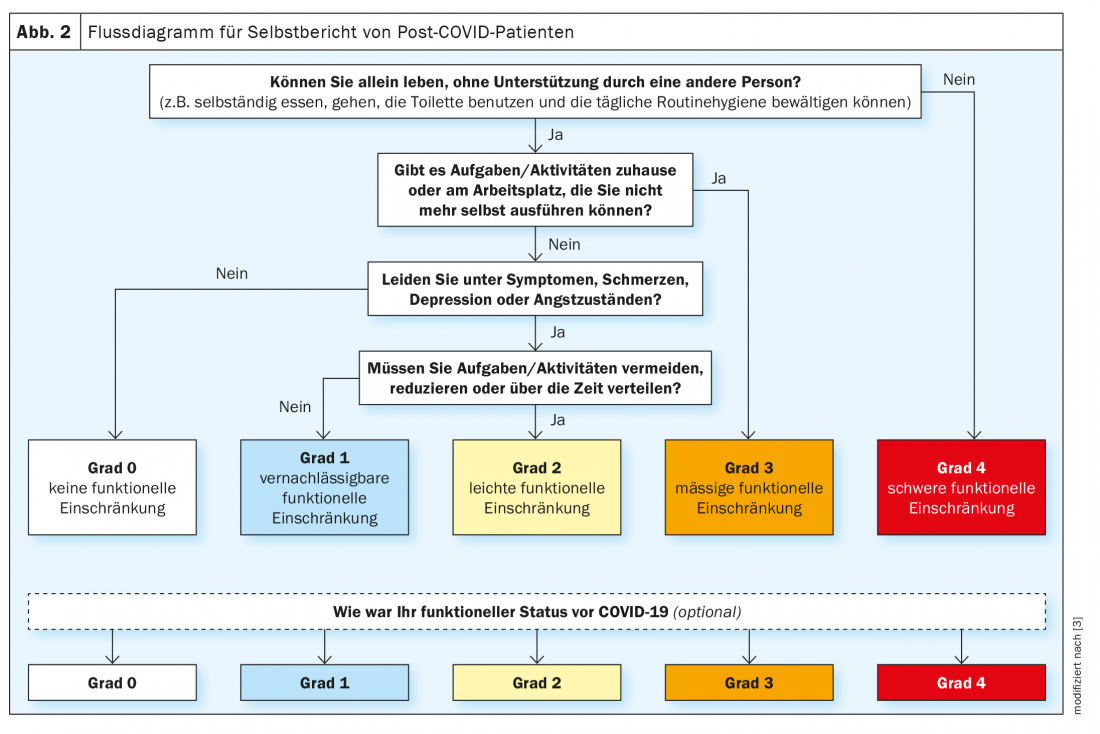
For the management of patients, he said, it is important to work together to develop a plan to get them out of their performance limitations and to give them an awareness that, on the one hand, it will get better over time, but on the other hand, it may take some time. Scoring systems such as those presented in the guideline (Fig. 2) are therefore important and can be given to patients to help them determine progress, Prof. Bahmer said.
Source: 128. Congress of the German Society for Internal Medicine (DGIM)
Literature:
- Wu X, Liu X, Zhou Y, et al: 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalization: a prospective study. Lancet Respir Med 2021; 9: 747-754; doi: 10.1016/S2213-2600(21)00174-0.
- Petersen EL, Goßling A, Adam G, et al: Multi-organ assessment in mainly non-hospitalized individuals after SARS-CoV-2 infection: The Hamburg City Health Study COVID programme. European Heart Journal 2022; 43 (11): 1124-1137; doi: 10.1093/eurheartj/ehab914.
- Koczulla AR, Ankermann T, Behrends U, et al: S1 guideline post-COVID/long-COVID 2021; AWMF registry number 020-027.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 2(4): 17-18.