Psychological disorders such as depression or ACS-induced PTSD may occur after myocardial infarction. Therefore, psychological support for heart attack patients is central. This is because the psyche influences both the quality of life and the survival rate.
Cardiovascular disease remains the leading cause of death, particularly in industrialized countries. According to a study by the Robert Koch Institute, almost 40% of deaths in Germany and other industrialized countries are due to cardiovascular diseases (heart attack, coronary heart disease, stroke, etc.) [1]. In this context, myocardial infarction occupies a special position, as it is the number one cause of death both in Switzerland and worldwide. In Switzerland alone, approximately 30,000 people (every 250th person) suffer an acute coronary event (myocardial infarction or angina pectoris) every year, according to the Swiss Federal Statistical Office [2]. Acute coronary syndrome also represents an economic and medical challenge for the health care system, with more than 220,000 inpatient admissions per year (D) and substantial morbidity and mortality even after the acute event (approximately 60,000 persons/year, D) and a deterioration in quality of life [3]. Based on a large American database (The Global Registry of Acute Coronary Events, GRACE) initiated by the University of Massachusetts Medical School, the 5-year mortality after an acute coronary syndrome is nearly 40% [4].
Psychosocial stress as a risk factor
In this context, evidence-based prevention and treatment of myocardial infarction is of immense importance for public health. In addition to the classic risk factors for a cardiovascular event such as smoking, obesity, high blood pressure, lack of exercise, etc., psychosocial risk factors have also received increasing attention in recent years [5]. This gave rise to the relatively young discipline of psychocardiology.
Heart and psyche are closely related. In colloquial language, many expressions have become established that refer to this circumstance: the heart leaps for joy, the heart is heavy, the heart is broken, the heart has almost stopped with fright, etc. Several large-scale international studies have been able to show that the risk of suffering a heart attack is two to four times higher in people with depression and anxiety disorders [6,7]. After dyslipidemia and smoking, psychosocial stress is the third most important factor influencing the development of cardiovascular disease – ahead of obesity and hypertension.
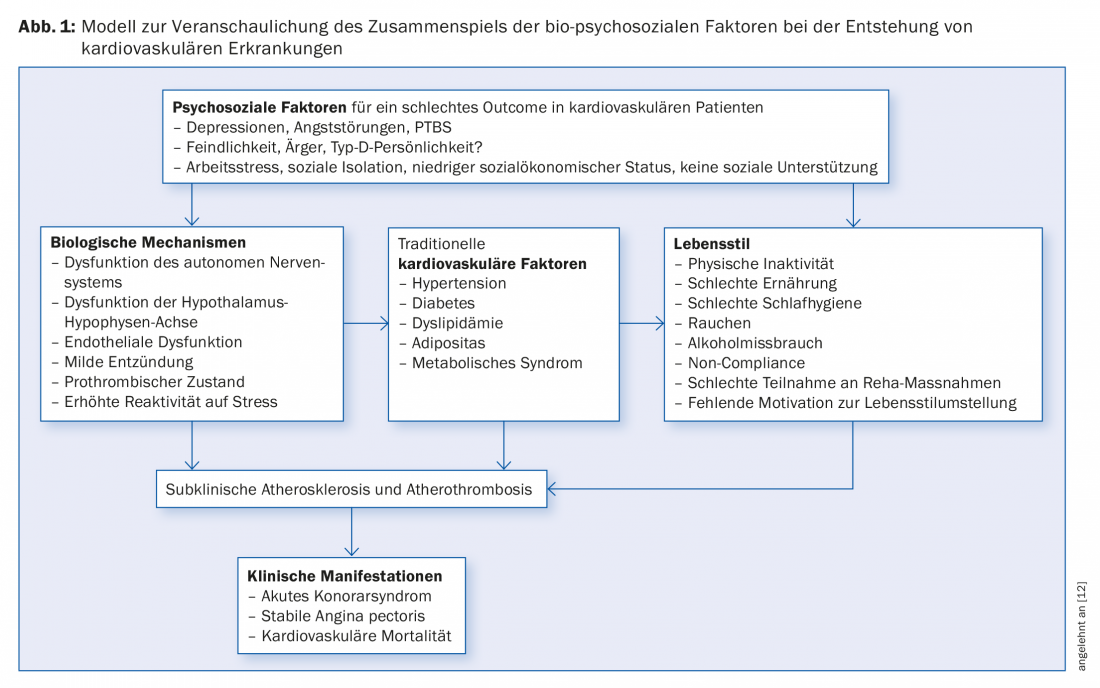
Prolonged psychosocial stress, which can later manifest itself in various mental illnesses, affects the cardiovascular system in two different ways, some of which overlap. In the neuropsychoimmunological sense, prolonged psychological stress leads to an increase in heart rate and hypertension, as well as a chronic increase in stress hormones (esp. cortisol). The latter causes a disturbance in fat and sugar metabolism, which under certain circumstances can worsen existing diabetes mellitus or lead to obesity. Overactivation of the sympathetic nervous system plays a central role. The immune system reacts with an inflammatory response [8]. The development of thrombi is favored [9].
A prospective observational study also demonstrated that the increased risk in people with depression or anxiety disorders was partly due to their unhealthy lifestyle [10]. This study of more than 6500 patients illustrated that modifiable behavioral factors were responsible for the majority of the increase in risk (approximately 65%). The main factors here are smoking at almost 41% (people with mental comorbidities smoke twice as often as healthy people), physical inactivity at 22%, and alcohol consumption at less than 2%. Somatic risk factors were less significant in comparison, e.g., hypertension at 13% and elevated CRP as an inflammatory marker at approximately 6%. Thus, a large number of lifestyle factors can be identified that could be influenced preventively with appropriate measures. However, they are often not explored or explored inadequately. The complex interrelationships between the psyche and the circulatory system, which interfere at both the biological and psychological levels, are exemplified in Figure 1.
The role of psychological factors in myocardial infarction
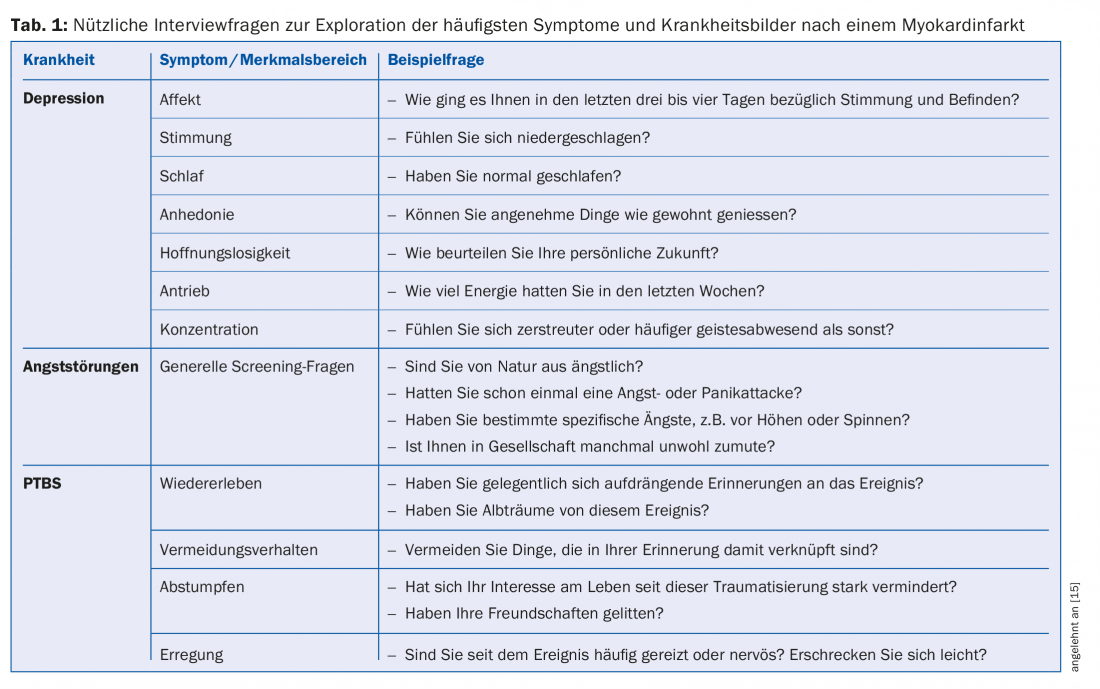
However, psychological factors also play a crucial role in the survival and quality of life of patients after or with cardiovascular disease. A heart attack is a traumatic event that makes affected patients aware of their helplessness or vulnerability and significantly affects their sense of physical integrity. In addition, as a result of the disease, they are dependent on long-term medication, which in turn is a constant reminder of the event. The most common sequelae after a cardiovascular event include depression, anxiety disorders, and post-traumatic stress disorder (PTSD) (Table 2).
Cardiovascular disease and depression are the leading causes of disability in industrialized countries. According to forecasts, this will also be the case for countries with a low gross national product by 2030 [11]. Compared with the general population, depression is two to three times more common in patients with cardiovascular disease. After myocardial infarction, nearly two-thirds of all patients show depressive symptoms and in about 15% the formal criteria for major depression are met, depending on the study. If a heart attack patient suffers from depression, his risk of dying is increased by almost three times. The risk of rehospitalization or reinfarction is also significantly higher and increases with the severity of depression. This is independent of whether the depression existed before the event or developed afterward; thus, both subtypes are important. The interactions between depression and cardiovascular health are multifaceted and multifactorial. They range from an unhealthy lifestyle with low physical activity, smoking, and unhealthy diet, to neuropsychoimmunological changes in hormone balance and coagulation, to quality of life effects such as mobility and loss of work. These complex relationships have only been partially explored.
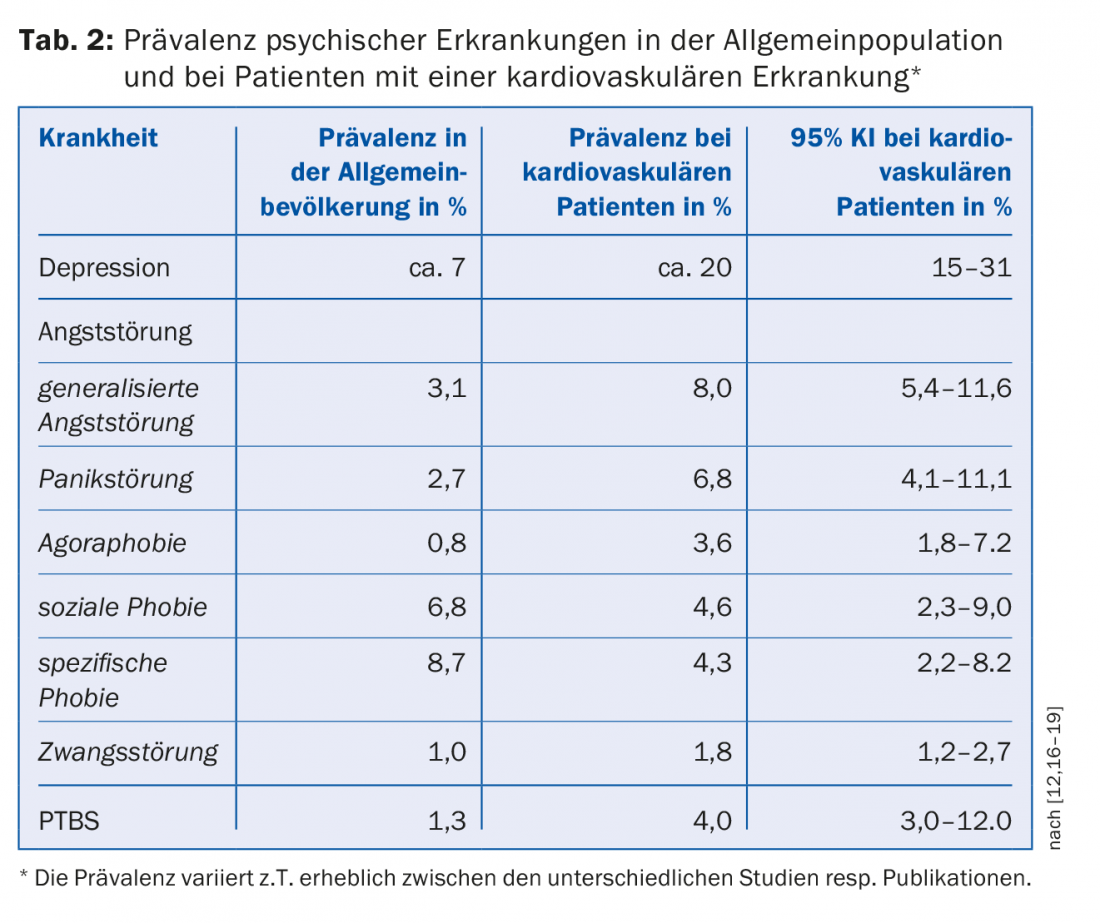
In approximately 16% of all myocardial infarction patients, various anxiety disorders are found, sometimes overlapping with depression. Generalized anxiety disorder is the most common form and also has the worst outcome [12]. Analogous to depression, anxiety disorder significantly increases the risk of myocardial infarction. There is also strong evidence that depression and anxiety in a mixed form pose a higher risk in terms of morbidity and mortality than the individual disorders.
Acute coronary syndrome-induced posttraumatic stress disorder (ACS-induced PTSD) is also receiving increasing attention. Full-blown PTSD occurs after myocardial infarction in about 4% of patients, and another 12% show symptoms typical of PTSD, such as flashbacks or avoidance behavior. Since about 15% of all people suffer a heart attack in the course of their lives, this problem affects many patients. According to a meta-analysis, ACS-induced PTSD doubles the risk of mortality and reinfarction after myocardial infarction [13]. However, this new entity of disease-related PTSD needs further research, especially with regard to potential treatment options.
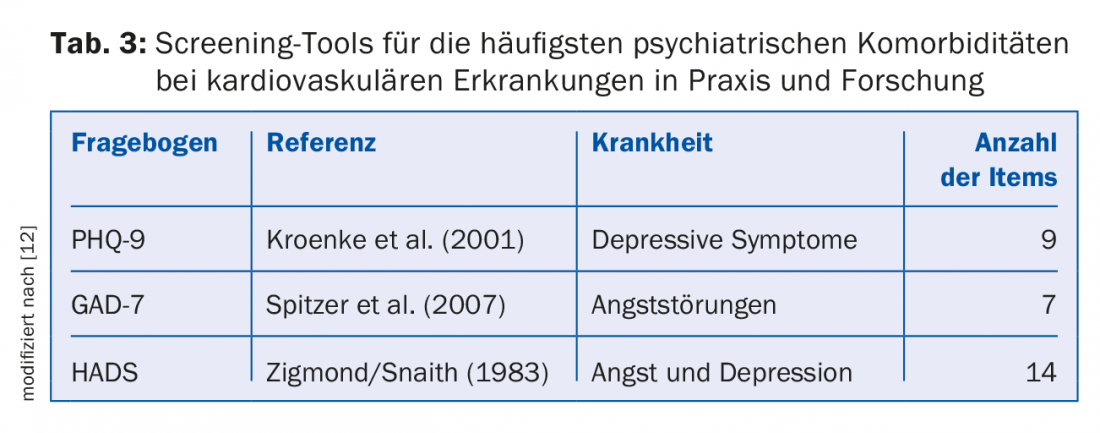
With the higher survival rate after an acute coronary syndrome (decrease in in-hospital mortality of approximately 0.5% per year) and excellent cardiac medications and treatment options, other factors such as quality of life, longer-term mortality, and rehospitalization rates are becoming more important. Since quality of life and mortality also depend significantly on the patient’s mental status, myocardial infarction patients should be specifically screened for psychiatric comorbidities using appropriate tools (Table 3) as well as adequately treated. In other words, screening is only effective if it is used as a basis for evidence-based therapy. Numerous treatment methods exist, and in principle a combination of drug therapy and psychological support is useful, to which the general practitioner can draw attention [14]. Outpatient or inpatient cardiac rehabilitation is able to reduce the relative mortality risk by about 25%. During rehabilitation, patients can be informed about the importance of psychosocial risk factors and further treatment options. Self-help groups are also helpful, and the effect of positive emotions is also considered proven. In the case of drug approaches, the advantages and disadvantages must be weighed on a case-by-case basis. For SSRIs, the benefits dominate because in addition to improving depression/anxiety, they also lead to better compliance. However, tricyclic antidepressants should not be used because of their unfavorable cardiovascular risk profile. In addition, lifestyle changes in terms of stress reduction, avoidance of noxious substances, healthy diet, physical activity and better stress management should be pursued, as these factors have an equal impact on heart and psyche.
Take-Home Messages
- Patients with myocardial infarction should also be asked about psychosocial stress and screened for mental illnesses such as depression, anxiety disorder, or PTSD, and treated if necessary, given the improved chances of survival. This can significantly improve quality of life and reduce mortality and hospitalization rates.
- The primary care physician should be sensitized to the importance of the psyche in cardiovascular disease and ask specifically about symptoms of mental illness (Table 1).
Literature:
- Robert Koch Institute: DEGS1: Basic publication with results. Basic Healthbl 2013; 56: 607-884.
- Swiss Federal Statistical Office: Cardiovascular Diseases. 2018. www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/krankheiten/herz-kreislauf-erkrankungen.html (accessed 06/30/2018).
- BÄK, KBV, AWMF: Nationale VersorgungsLeitlinie Chronische KHK, Langfassung. 2016.
- Tang E, Wong C, Herbison P: Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J 2007; 153(1): 29-35.
- Rozanski A: Behavioral Cardiology. JACC 2014; 64(1): 100-110.
- Smyth A, et al: Physical Activity and Anger or Emotional Upset as Triggers of Acute Myocardial Infarction. The INTERHEART Study. Circulation 2016; 134: 1059-1067.
- Małyszczak K, Rymaszewska J: Depression and anxiety in cardiovascular disease. Cardiologia Polska 2016; 74(7): 603-609.
- Wirtz P, von Känel R: Psychological Stress, Inflammation, and Coronary Heart Disease. Curr Cardiol Rep 2017; 19: 111.
- Austin A, Wissmann T, von Känel R: Stress and hemostasis: an update. Semin Thromb Hemost 2013; 39(8): 902-912.
- Hamer M, Molloy G, Stamatakis E: Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol 2008; 52(25): 2156-2162.
- Hare DL, et al: Depression and cardiovascular disease: a clinical review. Eur Heart J 2013; 35(21): 1365-1372.
- Pedersen S, et al: Psychosocial perspectives in cardiovascular disease. Eur J Prev Cardiol 2017; 24(3, Suppl.): 108-115.
- Edmondson D, et al: Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 2012; 7(6): e38915.
- von Känel R: Evidence-based psychocardiology – or what remained of type A behavior. Praxis 2016; 105(25): 1483-1491.
- Carlat D: The psychiatric interview. Bern 2013: Huber.
- Celano C, et al: Anxiety Disorders and Cardiovascular Disease. Curr Psychiatry Rep 2016; 18(11): 101.
- Edmondson D, von Känel R: Post-traumatic stress disorder and cardiovascular disease. Lancet Psychiatry 2017; 4(4): 320-329.
- von Känel R, et al: Early Psychological Counseling for the Prevention of Posttraumatic Stress Induced by Acute Coronary Syndrome: The MI-SPRINT Randomized Controlled Trial. Psychother Psychosom 2018; 87(2): 75-84.
- Shruthi DR, et al: Psychiatric comorbidities in acute coronary syndromes: six-month follow-up study. Indian J Psychiatry 2018; 60(1): 60-64.
HAUSARZT PRAXIS 2018; 13(8): 31-35