An update of the ROSCO panel evaluated the new classification system and updated evidence-based treatment recommendations. A symptom-oriented treatment strategy has proven effective in practice. With regard to pathophysiological relationships, there are some interesting new findings.
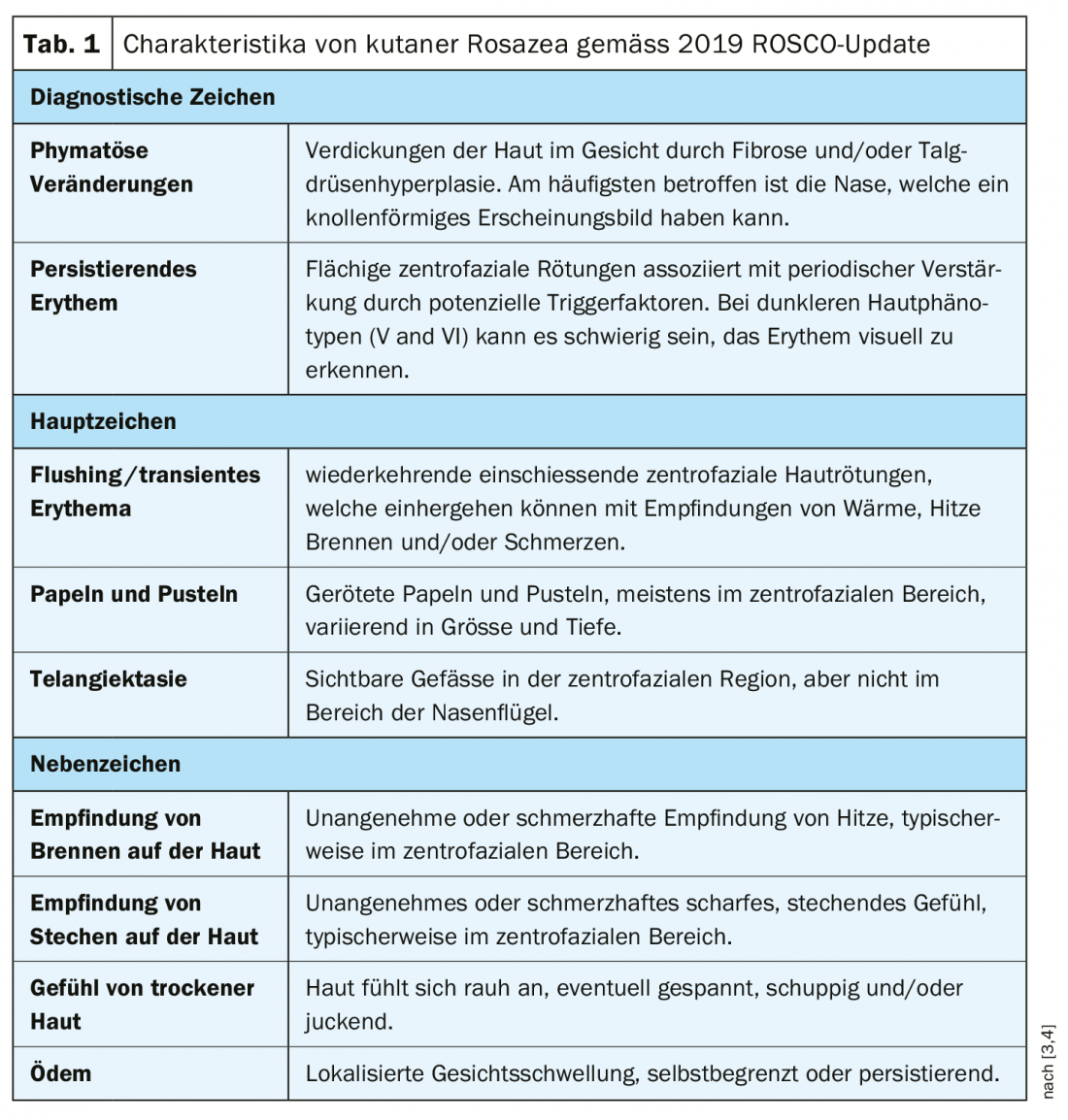
The characteristic rosacea symptoms manifest predominantly centrofacially, particularly affecting the forehead, nose, chin and cheeks. The previously used subtype classification (erythematous-teleangiectatic, papulopustular, phymatous, ocular rosacea) was replaced by a phenotype-based diagnosis in 2017 [1–3]. In a 2020 update published in the British Journal of Dermatology, the relevant international ROSCO (Rosacea COsensus) panel confirmed the adequacy of the new diagnostic classification [3]. This classification change is based on the realization that the earlier subtype classification does not sufficiently reflect the manifestations observed in practice, because in reality symptoms often overlap and transitions are fluid. Therefore, treatment should be primarily based on the symptoms of the disease. The main symptoms include flushing, persistent erythema, telangiectasia, papules with/without pustules, phymatous changes in the skin, and ocular manifestations [4] (Table 1). Burning, stinging, dry skin sensation, and circumscribed or diffuse edema are considered secondary diagnostic criteria. The primary goal of proper rosacea therapy is to significantly alleviate these clinical manifestations and symptoms. Depending on the severity of the symptoms, different active ingredients can be used and combined with each other.
Genetic predisposition and antimicrobial peptides.
According to current understanding, rosacea is a multifactorial disease with genetic predisposition. There are several recent empirical findings that support this thesis. Twin studies demonstrate at least 50% genetic determination in the occurrence of the disease [5]. The remaining 50% are due to environmental factors, such as UV radiation, temperature (extreme heat, cold), spicy foods, alcoholic beverages, and physical activity [5]. In a large-scale genome-wide association study with data from 22 952 individuals (2618 rosacea patients and 20 334 controls), two single nucleotide polymorphisms (SNPs) associated with rosacea could be identified [6]. Pathophysiologically, dysregulation of the innate and adaptive immune system, neuroinflammatory mechanisms, ultraviolet (UV) radiation, local inflammatory responses to cutaneous microorganisms, as well as alterations in vascular and lymphatic regulation appear to play a role [7]. The innate immune system secretes antimicrobial peptides at organism interfaces for the purpose of nonspecific defense against pathogens [4]. Cathelicidin LL-37, which occurs in humans, is one of these antimicrobial peptides and is produced by the skin. LL-37 plays a central role in rosacea pathogenesis and possesses antimicrobial as well as immunomodulatory and angiogenic properties. In rosacea patients, a specific pattern and increased cutaneous concentration of cathelicidin peptides could be detected due to increased production of cathelicidin precursor molecules and increased expression and activity of the serine protease kallikrein 5 [8]. The increased cathelicidin production and protease activity are induced by both the vitamin D signaling pathway, ER stress (ER: endoplasmic reticulum), and Toll-like receptor 2 (TLR2) [4,9].
Updated treatment recommendations
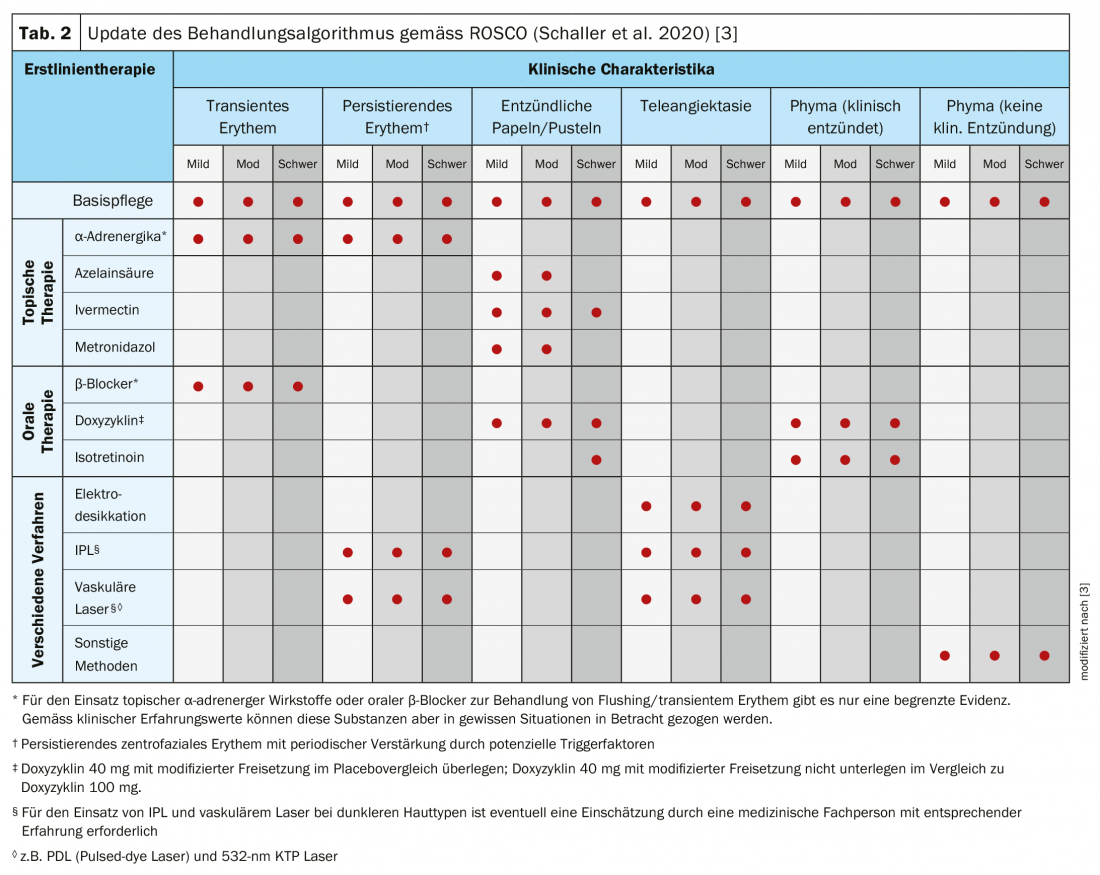
Phenotype-based diagnostic classification should allow for more targeted treatment and facilitate follow-up measurements of treatment success [10,11]. There is currently a lot going on in the area of rosacea drug discovery: there are over 150 ongoing studies on this in the ClinicalTrials.gov database [2,12]. An updated evidence-based recommendation for first-line therapy was published as part of the ROSCO project in 2019 (Tab. 2). On the occasion of the EADV Annual Meeting 2019, Prof. Bernard Cribier, MD, Strasbourg (F), summarized some of the most important findings from his point of view [2]:
Target 1 – Vessels (erythema, telangiectasia, flushing): According to a Cochrane Review published in 2019, a reduction of erythema and telangiectasis can be induced by using Nd:YAG and IPL [2,10]. With regard to topical treatment, in the REVEAL study [13], the active ingredient oxymetazoline 1x/d, which belongs to the group of sympathomimetics, proved to be effective and safe in reducing erythema in the setting of moderate to severe rosacea. At 52 weeks after baseline, more than one-third of patients achieved an improvement of at least 2 levels in both the Clinician Erythema Assessment Scale and the Subject Self Assessment Scale at 3 and 6 hours after application, respectively. There are long-term efficacy data on carvedilol from a smaller study in which sustained relief was achieved with respect to distinct facial flushing by 12.5 mg/d used over a 6-month period [14]. Botulinum toxin resulted in a reduction of erythema in several empirical studies [2].
Target 2 – Inflammation: Among the nonspecific drugs, doxycycline as well as ivermectin, metronidazole, and azelaic acid have shown a reduction in mediators of the constitutive immune system [2]. Potential therapeutic targets include Toll-like receptors, mast cells, and the enzyme kallicrein [15]. The latter is a key factor involved in the production of LL37 and pro-inflammatory mediators. Toll-like receptors play an important role in the activation of the innate immune system.
Target 3 – Neurovascular component: This involves dysregulated interactions between nerve endings and vessels of the upper dermis and epidermis. The most common primary feature of all forms of cutaneous rosacea is transient or persistent erythema on the face. Perilesional erythema of papules or pustules based on sustained vasodilation and plasma extravasation induced by inflammatory infiltrates. In contrast, transient erythema is characterized by rapid kinetics independent of papules and pustules. Among the current treatment options for facial erythema, topical brimonidine gel 0.33%, a member of the selective α2-adrenoceptor agonist group, has proven effective [16].
Target 4 – Demodex folliculorum: Topical applications of ivermectin and permethrin showed anti-parasitic effects. In a smaller study [17], a dual anti-inflammatory and anti-parasitic effect of topically applied ivermectin 1% was shown to be effective. Treatment was given over a period of three months and resulted in a reduction in the number of demodex by over 95%. For diagnostic purposes and for monitoring the progress of treatment, dermoscopy has proven useful [18]. It has been shown that there is a strong association between rosacea and the density of Demodex colonization, with an indirect relationship suspected [2]. The use of doxycycline, metronidazole, and azelaic acid can improve the clinical condition. There have been 72 different species of Demodex identified in rosacea [19].
Target 5 – Microbiota in general: From studies, it is known that the skin microbiome generally varies greatly from individual to individual and that a specific bacterial colonization can persist for months or years. The role of various bacterial strains as commensals or pathogenic microorganisms in rosacea disease is not yet fully understood. It is considered certain that systemic antibiotic treatment (e.g., tetracyclines, macrolides, beta-lactamines) modulates the composition of the microbiota [2,20].
Target 6 – Skin barrier: there are findings of increased transepidermal water loss as well as decreased hydration of the stratum corneum [21]. The specific modifications of the skin barrier are correlated with the severity of rosacea. Deterioration of pathogenetically altered constitutive immunity appears to be accompanied by deterioration of the skin barrier. Hydration of the skin barrier shows a correlation with inflammatory activity and can be positively influenced by therapy with minocycline [22].
Target 7 – Sebaceous glands: a high number of sebaceous glands in the skin is associated with expression of thymic stromal cells (TSLP) and specific immunological control mechanisms, which is impaired in rosacea. Treatment with oral low-dose isotretinoin was found to be significantly more effective in papulopustular rosacea compared with placebo (57.4% vs. 10.4%, p<0.0001) [23]. This is also the related conclusion of a Cochrane Review published in 2019 [10]. Accordingly, a dose of 0.10 to 0.15 mg/kg/d isotretinoin achieves the best efficacy. For the indication of edematous rosacea (“Morbihan’s disease”), a low isotretinoin dose of 0.5 mg/kg/d is most promising and shows good long-term results [2].
Target 8 – UV exposure, alcohol and smoking: With regard to UV radiation exposure, it has been found that the cathelicidin peptide LL37, which is characteristic of rosacea, leads to increased sensitivity with regard to UVB radiation. This reflects interactions between UV radiation, vessels, and the constitutive immune system [24]. Regarding alcohol, there was a dose-dependent increase in the risk of rosacea incidence. [25]. With regard to smoking as a possible risk factor, the evidence is inconsistent [26].
Literature:
- Tan J, et al: Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017; 176(2): 431-438.
- Cribier B: Rosacea: from the new spectrum to the new therapies. Prof. Bernard Cribier, MD, EADV Madrid, Oct. 12, 2019.
- Schaller M, et al: Recommendations for rosacea diagnosis, classification and management: update from the global ROSacea COnsensus 2019 panel. British Journal of Dermatology 2020; 182(5): 1269-1276.
- Reinholz M, et al: Pathogenesis and clinic of rosacea as key for symptom-oriented therapy. JDDG 2016; 14(S6): https://doi.org/10.1111/ddg.13139_g
- Aldrich N, et al: Genetic vs Environmental Factors That Correlate With Rosacea: A Cohort-Based Survey of Twins. JAMA Dermatol. 2015; 151: 1213-1219.
- Chang AL, et al: Assessment of the genetic basis of rosacea by genome-wide association study. J Invest Dermatol. 2015; 135: 1548-1555.
- Cribier B: Pathophysiology of rosacea: redness, telangiectasia, and rosacea. Ann Dermatol Venereol. 2011; 138 (Suppl. 3): S184-191.
- Yamasaki K, et al: Increased serine protease activity and cathelicidin promotes skin inflammation in rosacea. Nat Med 2007; 13: 975-980.
- Reinholz M, et al: LL-37: an antimicrobial peptide with a role in inflammatory skin disease. Ann Dermatol. 2012; 24: 126-135.
- Van Zuuren EJ, et al: Interventions for rosacea based on the phenotype approach: an updated systematic review including GRADE assessments. Br J Dermatol 2019; 181(1): 65-79.
- Gallo RL, et al: Standard classification and pathophysiology of rosacea: the 2017 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol 2018; 78: 148-155.
- ClinicalTrials.gov: https://clinicaltrials.gov/
- Draelos ZD, et al: Efficacy and safety of oxymetazoline cream 1.0% for treatment of persistent facial erythema associated with rosacea: Findings from the 52-week open label REVEAL trial. JAAD 2018; 78(6): 1156-1163.
- Pietschke K, Schaller M: Long-term management of distinct facial flushing and persistent erythema of rosacea by treatment with carvedilol. Journal of Dermatological Treatment 2018; 29(3): 310-313.
- Mascarenhas NL, et al: TRPV4 Mediates Mast Cell Activation in Cathelicidin-Induced Rosacea Inflammation. Journal of Investigative Dermatology 2017; 137: 972-975.
- Steinhoff M, Schmelz M, Schauber J: Facial Erythema of Rosacea – Aetiology, Different Pathophysiologies and Treatment Options. Acta Derm Venerol 2016; 96: 579-586.
- Schaller M, et al: Dual anti-inflammatory and anti-parasitic action of topical ivermectin 1% in papulopustular rosacea. JEADV 2017; 31(11): 1907-1911.
- Friedman P, et al: Usefulness of dermoscopy in the diagnosis and monitoring treatment of demodicidosis. Dermatol Pract Concetp 2017; 7(1): 6.
- Murillo N, Aubert J, Raoult D: Microbiota of Demodex mites from rosacea patients and controls. Microb Pathogenesis 2014; 71-72: 37-40.
- Woo YR, et al: Characterization and Analysis of the Skin Microbiota in Rosacea: Impact of Systemic Antibiotics. J Clin Med 2020; 9(1): 185; https://doi.org/10.3390/jcm9010185
- Kim J, et al: Clinical assessment of rosacea severity: oriental score vs. quantitative assessment method with imaging and biomedical tools. Skin Research and Technology 2016; 23 : 186v293.
- Ni Raghallaigh S, Powell FC: Epidermal hydration levels in patients with rosacea improve after minocycline therapy. British Journal of Dermatology 2014; 171: 259-264.
- Sbidian E, et al: A randomized-controlled trial of oral low-dose isotretinoin for difficult-to-treat papulopustular rosacea. Journal of Investigative Dermatology 2016; 136(6): 1124-1129.
- Kulkarni NN, et al: Innnate immune dysfunction in rosacea promotes photosensitivity and vascular adhesion molecule expression. J Invest Dermatol 2020; 140(3): 645-655.e6.
- Lj S, et al. Alcohol intake and risk of rosacea in US women. J Am Acad Dermatol 2017; 76(6): 1061-1067.e2.
- Li S, et al: Cigarette smoking and risk of incident rosacea in women. Am J Epidemiol 2017; 186(1): 38-45.
DERMATOLOGY PRACTICE 2020; 30(5): 42-45