BCL-2 inhibition represents a milestone in the history of blood cancer treatment. Approved for the treatment of relapsed or refractory chronic lymphocytic leukemia (CLL), oral small molecule is now also being investigated for the treatment of acute myeloid leukemia (AML) and other indications.
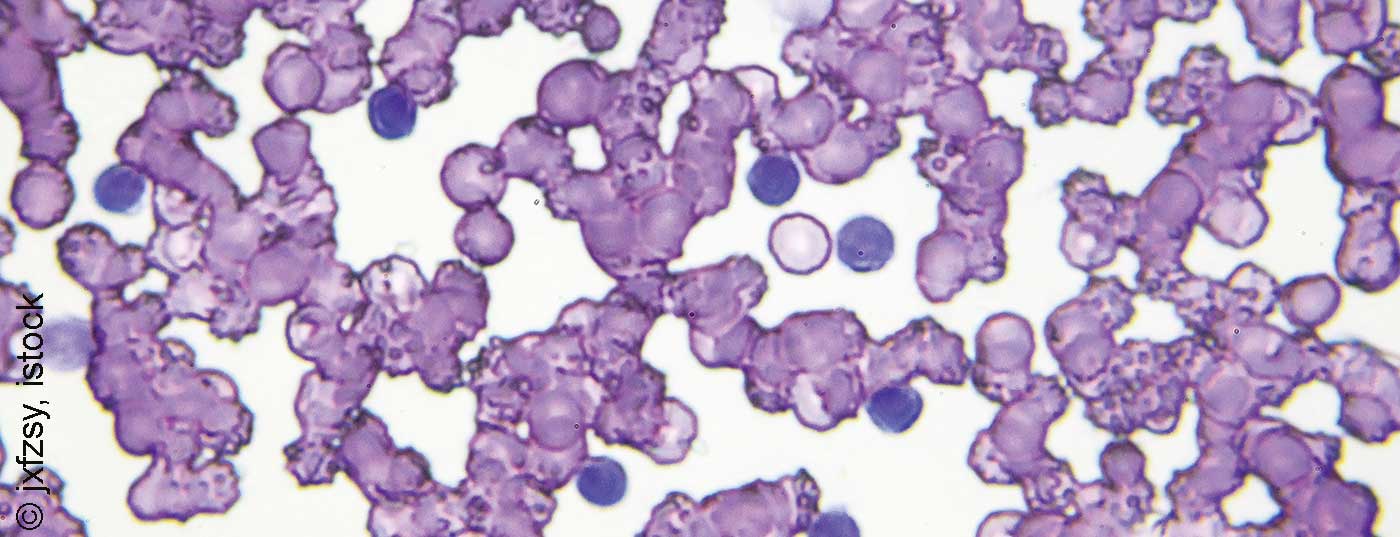
Selective binding of the inhibitor to the anti-apoptotic BCL-2 protein solubilizes proteins such as BIM and BAX. These interact and restore the signaling cascade of programmed cell death. Release of cytochromes c from mitochondria activates caspases, which ultimately lead to apoptosis of the cancer cell. The dependence of malignant cells on survival-promoting proteins has been shown in various hematologic diseases. Overexpression of BCL-2 is found not only in CLL, but also in AML, acute lymphoblastic leukemia (ALL), follicular lymphoma (FL), diffuse large B-cell lymphoma (DLBCL), and various solid tumors, said Prof. Thorsten Zenz, MD, Zurich. It is also now known that BCL-2 inhibitors can induce apoptosis both alone and in combination with agents that increase BCL-2 dependence. This finding was the basis for further studies to investigate the use of venetoclax (Venclyxto®) in other indications.
Therapy development in CLL
In patients with chronic lymphocytic leukemia who progressed on or after ibrutinib, the BCL-2 inhibitor showed promising results in an interim analysis of a multicenter, open-label, non-randomized phase II study. After a median follow-up of 14 months, 65% of patients showed a response according to iwCLL criteria. 9% had a complete remission or complete remission with incomplete recovery in the bone marrow, 3% a nodular partial remission and 52% a partial remission. Progression-free survival was 75% at 12 months, as reported by Assoc. Prof. PD Dr. Dr. Philipp Staber, Vienna.
The current results of the three-year follow-up of the open-label, multicenter, randomized Phase III MURANO study, which evaluated venetoclax in combination with rituximab in patients with relapsed or refractory CLL compared to bendamustine plus rituximab, are also encouraging. Progression-free survival was 71.4% vs. 15.2%. “A higher rate of undetectable minimal residual disease was also achieved at 62%, which was maintained during subsequent monotherapy with venetoclax,” the expert said. “The therapy algorithm for2nd line CLL treatment should be reconsidered according to these data.”
However, something could also be happening in first-line therapy, looking at the results of the randomized phase 3 clinical trial CLL14. The combination of venetoclax plus obinutuzumab versus obinutuzumab plus chlorambucil was studied in CLL patients with coexisting disease who had not received prior treatment. Progression-free survival was 88.2% vs. 64.1% at 24 months.
Alternatives to classical chemotherapy
In acute myeloid leukemia, the BCL-2 inhibitor in combination with azacitidine causes an inhibition of oxidative phosphorylation in AML stem cells, PD Dr. Christoph Röllig, Dresden, explained the mode of action of the effective new therapeutic approach in elderly patients with AML diagnosed for the first time. A combination of venetoclax with HMA could also replace intensive chemotherapy, as suggested by initial study results.
Source: Symposium “The Next Chapter In BCL-2 Inhibition” on the occasion of SOHC, June 28, 2019, Zurich.
InFo ONCOLOGY & HEMATOLOGY 2019; 7(4): 30 (published 9/20/19, ahead of print).