The Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations regarding initial pharmacotherapy for COPD patients remain unchanged in their 2021 update. However, that could soon change. Current studies suggest: the combination of long-acting beta2-sympathomimetic (LABA) and inhaled corticosteroid (ICS) is increasingly being sidelined.
In the established treatment regimen, patients classified as group A should be given either a long-acting muscarinic antagonist (LAMA) or a LABA. In Group B, a LAMA or LABA or the combination LABA/LAMA. “That means a little bit: Do what you want, nothing hurts,” criticized Prof. Dr. Felix Herth from the Department of Pneumology and Respiratory Medicine, Thoraxklinik Heidelberg (D) [1]. In the EMAX study [2], the effect of the different substances was tested for patient group B. Prof. Herth exemplified the results for the endpoint dyspnea score: the best impact on dyspnea was achieved with dual bronchodilation (Fig. 1), but all other endpoints also performed better. “So I hope that in 2022, when the study will find influence in the GOLD report, it will be recommended to do LAMA/LABA therapy, because the data were significantly better than for any monotherapy,” the expert said.
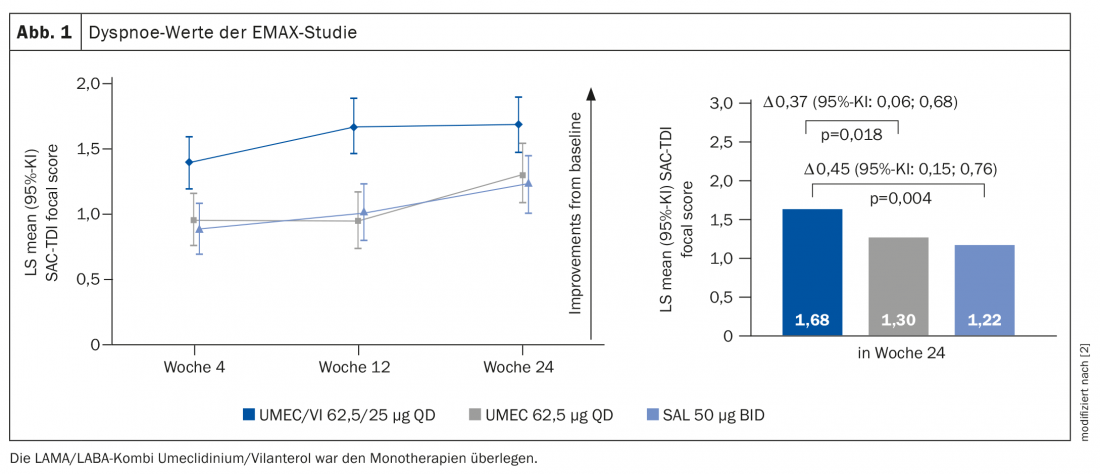
According to him, the study was also able to settle the question of whether there was a dependence on symptom burden. In the past, it was often assumed that a patient would only benefit from LAMA/LABA if they also had a lot of symptoms, i.e. a very high CAT. With a low CAT around 10-15, on the other hand, no benefit is to be expected. This rumor could now be put to rest: “No matter how mild or severe, the combination always beat the respective monosubstances.”
Triple significantly better
Meanwhile, there are also real-world data that have compared LAMA/LABA vs. LABA/ICS. This clearly showed that under everyday conditions, LAMA/LABA also performed better than LABA/ICS. “The question of whether I even need a combination LABA/ICS in a COPD patient, I now answer in the negative,” Prof. Herth therefore explained. “Because either he doesn’t exacerbate and doesn’t have an eosinophilia, then I’ll run LAMA/LABA. Or he exacerbates and has an eosinophilia, then I run triple.” The expert now considers the value of a LABA/ICS combo in COPD to be rather low: “The niche for this combo is getting narrower.”
Further information on this is also provided by the ETHOS study [3], in which – corresponding to pationten group D – triple therapy vs. combinations was investigated. The study authors randomized patients to triple therapy with two different doses or to a LAMA/LABA or a LABA/ICS group. The triple therapies proved to be significantly better in terms of exacerbation frequency. “The triple has very clear advantages over the two combinations if the patient is exacerbating and has eosinophilia,” Prof. Herth stated. These data are also consistent with the IMPACT study from last year. Thus, the effects were evidently substance-independent [4]. There was no difference between the two ICS doses. There are always pneumonia signals, especially at higher ICS doses, but these are significantly reduced compared with previous studies, the pulmonologist said.
Mortality reduction likely
Both ETHOS and IMPACT were also analyzed for mortality signal and both showed a reduction in mortality in the triple arm. Based on this, the question of whether triple therapy reduces mortality risk in a COPD patient with the correct indication has not been definitively proven. Prof. Herth admitted that patients in the studies were randomized differently in some cases (e.g. in some patients the cortisone was discontinued during the randomization phase, which can of course have effects, and there were also different collectives with regard to the asthma history) and that the results are therefore certainly open to discussion. What can be stated, however, is that “there are two large studies with large numbers of patients that have shown a mortality signal for the triple, so I do think that in a patient with many exacerbations and possibly an eosinophilia, a mortality reduction can certainly be expected with the triple therapy.”
The question remains whether there are also patients who should better not be treated with a corticosteroid? And what is the best way to evaluate them? There is a consensus paper on this from the ERS [5]. In this, two parameters are crystallized that indicate that a patient will not benefit from or should be treated with ICS: exacerbation history and eosinophil granulocyte count. Eosinophilia is rated higher in the paper in this regard. “So if a patient on triple therapy with ICS presents after a year without exacerbations, I would measure the eosinophils again – if their number proves to be high, I should definitely not stop,” Prof. Herth said. However, if eosinophils are low, discontinuation is certainly indicated, not least in view of the side effects that ICS can also cause.
Take-Home Messages
- Under everyday conditions in an unselected patient population, symptom control is better with LAMA/LABA than with LABA/ICS.
- In symptomatic patients with a prominent history of exacerbations, triple is superior to LAMA/LABA in terms of prevention of exacerbations.
- In certain patients (symptomatic, exacerbations on therapy), mortality reduction is likely with triple therapy.
- Consider exacerbation history + eosinophilic granulocytes (+ initial indication) when discontinuing ICS.
Sources:
- StreamedUp Best of Pneumo Update 2020, Jan. 14, 2021; www.streamed-up.com/best-of-pneumo-update
- Maltais F et al: Efficacy of umeclidinium/vilanterol versus umeclidinium and salmeterol monotherapies in symptomatic patients with COPD not receiving inhaled corticosteroids: the EMAX randomised trial. Respir Res 2019; 20: 238; doi: 10.1186/s12931-019-1193-9.
- Rabe KF et al: Triple Inhaled Therapy at Two Glucocorticoid Doses in Moderate-to-Very-Severe COPD. N Engl J Med 2020; 383: 35-48; doi: 10.1056/NEJMoa1916046.
- Lipson DA et al: Reduction in All-Cause Mortality with Fluticasone Furoate/Umeclidinium/Vilanterol in Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2020; 201: 1508-1516; doi: 10.1164/rccm.201911-2207OC.
- Chalmers JD et al: Withdrawal of inhaled corticosteroids in COPD: a European Respiratory Society guideline. Eur Respir J 2020; 55: 2000351; doi: 10.1183/13993003.00351-2020.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(2): 18-20.











