If depressive symptoms cannot be alleviated with conventional approaches, brain stimulation methods can be helpful. These can also be combined well with pharmacotherapy and psychotherapy.
In depressive disorders, we usually assume that episodes of illness can be significantly shortened with guideline-based treatment. For many patients, this also offers hope for recovery and thus regaining their health and level of function. In clinical reality, however, we often encounter patients whose symptoms cannot be fully alleviated by conventional treatment, whose episodes of illness are particularly long-lasting and chronic.
Therapy resistance or pseudotherapy resistance?
Treatment success is reported in studies as response (>50% reduction in depression severity) or remission (scores below the cut-off for depression in specific scales, e.g., >10 points in the Montgomery Asberg Depression Scale). Depending on the therapy method, we see a response of the first treatment in about 50% of patients, while about 30% achieve remission. Consequently, in more than half of depression patients, the treatment strategy must be changed as soon as it becomes apparent that remission cannot be achieved. The proportion of those who remit to a new treatment becomes smaller with each treatment step. Thus, clinicians face the dilemma of having to modify ineffective therapies while at the same time decreasing the chances of remission with each additional treatment step. Overall, estimates suggest that approximately 30% of patients with depression develop treatment resistance, i.e., fail to respond to at least two antidepressant therapy attempts of sufficient duration and dosage. With a lifetime prevalence of 16-20%, quite a substantial amount of people face this so-called treatment resistance for depression.
It is particularly important to avoid and recognize so-called pseudotherapy resistance due to inadequate treatment. Pseudotherapy resistance can occur, for example, when adjustments are not made despite evidence that a treatment is not effective. It is not uncommon to see patients in clinical practice who have been treated for months with the same antidepressant at the same dosage without a clear response – or with psychotherapy techniques that have proven ineffective for depression.
Brain stimulation therapy can be combined well
The treatment of depression according to the guideline requires that the effectiveness of the treatment is repeatedly reviewed at regular, shorter intervals and that the treatment plan is adjusted. For this, there is a staged approach with different options and the best evidence to date for augmentation of a primary antidepressant agent with lithium. Modern depression treatment will also use a combination of disorder-specific psychotherapy (cognitive behavioral therapy or interpersonal psychotherapy),optimized pharmacotherapy, and brain stimulation techniques when appropriate, for moderate to severe depression.
Particularly in major depression, studies showed that guideline-compliant treatment according to algorithm led to remission significantly more often and faster than conventional treatment [1,2]. Adherence to treatment recommendations is thus extremely important for the course of the disease, especially at the beginning of therapy. However, for economic reasons, studies of the best methodological quality are available almost exclusively for acute and early depression. There, the evidence base is excellent. However, very few studies are able to depict the situation when treatment resistance has occurred with the necessary changes in strategy. Here, it comes down to the sensible combination of disorder-specific psychotherapy, intensified pharmacotherapy and brain stimulation techniques. In the tertiary care setting, we see patients who had already received several antidepressants for a sufficient length of time and in sufficient doses. However, we do not encounter consistent augmentation strategies with tricyclic antidepressants and lithium as standard. Also, few patients with chronic depression receive the specific psychotherapy methods that have the best evidence base here, such as Cognitive Behavioral Analysis System of Psychotherapy (CBASP) and Mindfulness Based Cognitive Therapy (MBCT).
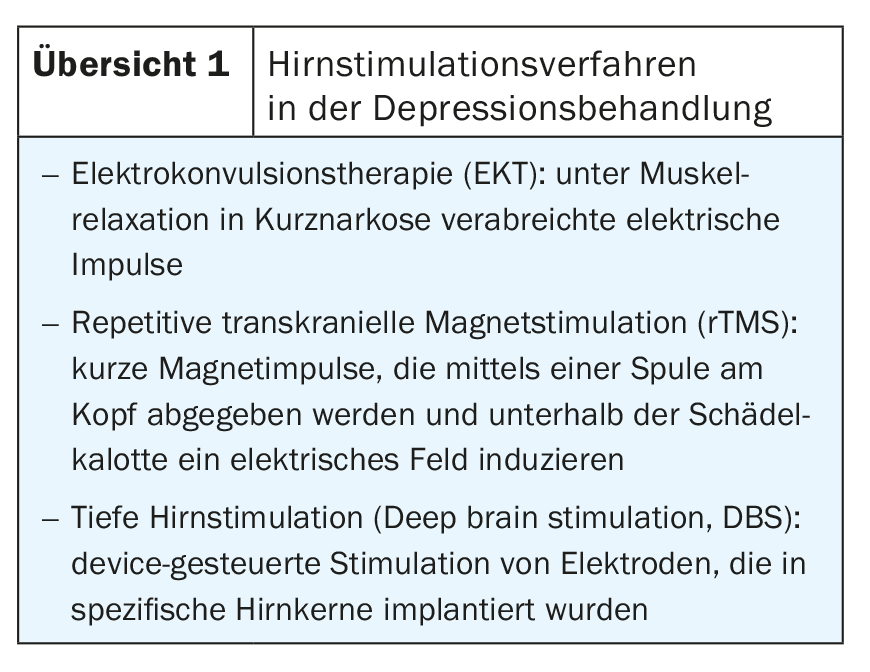
We usually offer patients with advanced treatment resistance a combination treatment of disorder-specific psychotherapy, intensified pharmacotherapy, and brain stimulation. One advantage of brain stimulation techniques (overview 1) is their excellent combinability with existing psychotherapy and pharmacotherapy.
Electroconvulsive therapy (ECT) unfairly discredited
Electroconvulsive therapy (ECT) has been used in the treatment of seriously ill patients for 80 years. For ECT, we have the best data and richest experience. ECT is particularly effective in severely ill patients with depression, especially psychotic symptoms, motor slowing, older age or the melancholic subtype. In general, ECT tends to be started too late in Switzerland. This treatment is usually used only when treatment resistance has occurred, although remission rates with ECT are particularly high in patients who have not yet achieved treatment resistance (65% vs. 48%) [3]. The treatment requires specific knowledge and especially the cooperation of anesthesiologists, since ECT is administered under muscle relaxation in short anesthesia. Unjustly, this form of treatment is discredited in public as “electroshock treatment”. Recent studies and meta-analyses even refute common fears that ECT could lead to brain damage or that severe cognitive deficits regularly occur [4–6]. Cognitive deficits can be prevented with the use of high-dose unilateral ECT [4]. ECT has excellent evidence in treatment-resistant cases [3,7] and is therefore an integral part of various international guidelines as well as the Swiss treatment recommendations. ECT is offered in some centers in Switzerland.
Repetitive transcranial magnetic stimulation (rTMS) is well tolerated
In addition to ECT, repetitive transcranial magnetic stimulation (rTMS) is also available to us today. The rTMS uses short magnetic pulses which are emitted by a coil on the head. The magnetic field induces an electric field directly below the cranial dome, which in turn leads to depolarization of cortical neurons [8]. The duration, frequency and pulse strength determine whether the nerve cells are stimulated or inhibited and how long this effect will last. In the treatment of depression, it has been shown to be helpful to either excitatory stimulate the left dorsolateral prefrontal cortex (DLPFC) or inhibit the right dorsolateral prefrontal cortex. Bilateral stimulation protocols simultaneously excite the left DLPFC and inhibit the right DLPFC. Newer protocols also target modulation of the ventromedial prefrontal cortex, but this is somewhat harder for TMS devices to reach. A recent meta-analysis shows that a number of different TMS protocols are very effective in achieving remission in placebo-controlled randomized trials, e.g., bilateral rTMS or high-frequency excitatory rTMS over the left DLPFC [9]. Most of these studies performed rTMS as an additional treatment to existing pharmacotherapy and psychotherapy (69%) for treatment-resistant depression (74%). rTMS continues to be the subject of active research aimed at greater effect or higher efficiency. For example, treatment intensity is an issue. High-frequency excitatory stimulation of the left DLPFC has been repeated 10-15 times in daily sessions from Monday to Friday in most protocols to date. In the process, the treatment lasted about 37 minutes. Encouragingly, in 2018, a controlled study demonstrated that a newer, excitatory rTMS protocol can achieve the same efficacy, with a time commitment of only three minutes per session [10]. This so-called “theta-burst” stimulation will be preferable to high-frequency treatment for reasons of practicability, while maintaining the same efficacy. Other open questions currently under discussion include prediction of treatment success, algorithms in the absence of efficacy (e.g., staged changes in stimulation targets), or the efficacy and frequency of rTMS maintenance therapy.
In the value of brain stimulation methods for treatment-resistant depression, rTMS occupies an interesting role. It is certainly less effective than ECT, but at the same time this treatment is much better tolerated than ECT and can be offered more easily. All that is required is the purchase of a TMS device and specific training on how to perform the treatment. However, the psychiatrist does not need the assistance of an anesthesiologist here as he does with ECT. Currently, however, there is also a lack of economic incentives to offer rTMS in practices or institutions, as there is no specific TARMED position on payment. In the future, however, rTMS will be part of the broad range of psychiatric treatment methods; especially in depression treatment, but also for other indications.
Deep brain stimulation (DBS) for severe cases of treatment resistance.
For patients with marked resistance to therapy who, for example, have not responded even to series of ECT treatments, there is the option of invasive brain stimulation methods. Deep brain stimulation (DBS) is a procedure used in the treatment of pharmacotherapy-resistant movement disorders, in which millimeter-thin electrodes are inserted into specific brain nuclei and can be targeted externally by means of a pacemaker. In the treatment of depression, goals in the reward system are primarily targeted. This involves using high-frequency electrical stimulation to send an interfering signal that makes dysfunctional circuitry less effective in depressed patients. In the reward system, the bilateral nucleus accumbens, the subgenual cingulate, the lateral habenula, or the anterior portion of the internal capsule have been the main stimuli [11]. All of these components are connected by the medial forebrain bundle, an important fiber strand in the reward system that itself can also be stimulated [12]. This fiber bundle is structurally altered in patients with chronic depression or melancholic depression [13,14]. In the treatment of depression, DBS is still in the experimental stage, as controlled trials can only be conducted on very small groups due to complexity and cost. Within the group of severely ill patients with clear resistance to therapy, however, impressive successes have been achieved, with 50-70% of these patients responding to treatment [15,16]. DBS is only offered in highly specialized centers such as the Neurocentre at Bern Inselspital, because the treatment requires close cooperation between psychiatry, neurosurgery and neurology. In addition to neurosurgery, careful adjustment of stimulation parameters over many weeks is complex. DBS is offered as an add-on therapy to existing pharmacotherapy and psychotherapy, which also need to be adjusted over the course of long-term DBS treatment.
Take-Home Messages
- Treatment according to therapy algorithms is particularly effective.
- Brain stimulation techniques can be excellently combined with pharmacotherapy and psychotherapy.
- ECT is safe and an integral part of the treatment chain for major depression. rTMS as a non-invasive procedure is user-friendly and effective.
- Invasive stimulation at the end of the treatment chain is possible and can help the seriously ill.
Literature:
- Bauer M, et al: Efficacy of an algorithm-guided treatment compared with treatment as usual: a randomized, controlled study of inpatients with depression. J Clin Psychopharmacol 2009; 29(4): 327-333.
- Adli M, et al.: How Effective Is Algorithm-Guided Treatment for Depressed Inpatients? Results from the Randomized Con-trolled Multicenter German Algorithm Project 3 Trial. Int J Neuropsychopharmacol 2017; 20(9): 721-730.
- Heijnen WT, Birkenhager TK, Wierdsma AI, van den Broek WW: Anti-depressant pharmacotherapy failure and response to subsequent electro-convulsive therapy: a meta-analysis. J Clin Psychopharmacol 2010; 30(5): 616-619.
- Semkovska M, et al: Bitemporal Versus High-Dose Unilateral Twice-Weekly Electroconvulsive Therapy for Depression (EF-FECT-Dep): A Pragmatic, Randomized, Non-Inferiority Trial. Am J Psychiatry 2016; 173(4): 408-417.
- Biedermann SV, et al: Improvement in verbal memory performance in depressed in-patients after treatment with electroconvulsive therapy. Acta Psychiatr Scand 2016; 134(6): 461-468.
- Takamiya A, et al: Effect of electroconvulsive therapy on hippocampal and amygdala volumes: systematic review and meta-analysis. Br J Psychiatry 2018; 212(1):19-26.
- UK ECT Review Group: Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 2003; 361(9360): 799-808.
- Lefaucheur JP, et al: Evidence-based guide-lines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol 2014; 125(11): 2150-2206.
- Brunoni AR, et al: Repetitive Transcranial Magnetic Stimulation for the Acute Treatment of Major Depressive Episodes: A Systematic Review with Network Meta-analysis. JAMA Psychiatry 2017; 74(2): 143-152.
- Blumberger DM, et al: Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimula-tion in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet 2018; 391(10131): 1683-1692.
- Schlaepfer TE, et al: Deep brain stimulation of the human reward system for major depression – rationale, outcomes and outlook. Neuropsychopharmacology 2014; 39(6): 1303-1314.
- Coenen VA, et al: Tractography-assisted deep brain stimulation of the superolateral branch of the medial forebrain bundle (slMFB DBS) in major depression. NeuroImage Clinical 2018; 20: 580-593.
- Bracht T, et al: White matter microstructure altera-tions of the medial forebrain bundle in melancholic depression. J Affect Disord 2014; 155: 186-193.
- Bracht T, et al: Limbic white matter microstructure plasticity reflects recovery from depression. J Affect Disord 2015; 170: 143-149.
- Bewernick BH, et al: Deep brain stimulation to the medial forebrain bundle for depres-sion- long-term outcomes and a novel data analysis strategy. Brain Stimul 2017; 10(3): 664-671.
- Bewernick BH, et al: Long-term effects of nucleus accumbens deep brain stimulation in treatment-resistant depression: evidence for sustained efficacy. Neuropsychopharmacology 2012; 37(9): 1975-1985.
InFo NEUROLOGY & PSYCHIATRY 2019; 17(2): 13-16.











